1.1 Preparation for kidney failure:
Patients who reach CKD stage 4 (estimated GFR < 30 mL/min/1.73 m2) should receive timely education about kidney failure and options for its treatment, including kidney transplantation, PD, HD in the home or in-center, and conservative treatment. Patients' family members and caregivers also should be educated about treatment choices for kidney failure. (B)1.2 Estimation of kidney function:
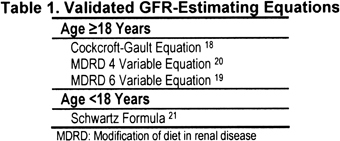
Estimation of GFR should guide decision making regarding dialysis therapy initiation. GFR should be estimated by using a validated estimating equation (Table 1) or by measurement of creatinine and urea clearances, not simply by measurement of serum creatinine and urea nitrogen. Table 2 and Table 3 summarize special circumstances in which GFR estimates should be interpreted with particular care. (B)1.3 Timing of therapy:
When patients reach stage 5 CKD (estimated GFR < 15 mL/min/1.73 m2), nephrologists should evaluate the benefits, risks, and disadvantages of beginning kidney replacement therapy. Particular clinical considerations and certain characteristic complications of kidney failure may prompt initiation of therapy before stage 5. (B)
Optimum timing of treatment for patients with CKD prevents serious and uremic complications, including malnutrition, fluid overload, bleeding, serositis, depression, cognitive impairment, peripheral neuropathy, infertility, and increased susceptibility to infection. However, all forms of kidney replacement therapy entail important trade-offs. As GFR decreases, patients and physicians must weigh many risks and benefits. Decision making is more complex for older and more fragile patients. Together, patients and physicians must continually reconsider whether the anticipated physiological benefits of solute clearance and extracellular fluid (ECF) volume control now outweigh the physical risks and psychosocial toll of therapy. In some cases, social and psychological factors may lead to earlier dialysis therapy initiation, and in some cases, to later initiation. The initiation of dialysis therapy remains a decision informed by clinical art, as well as by science and the constraints of regulation and reimbursement.
For some patients, conservative therapy, without dialysis or transplantation, is the appropriate option.27-29 If the patient makes this choice, the health care team should strive to maximize QOL and length of life by using dietary and pharmacological therapy to minimize uremic symptoms and maintain volume homeostasis. These include, but are not limited to, use of low-protein diets, ketoanalogs of essential amino acids, loop diuretics, and sodium polystyrene sulfonate. Nephrologists also should be familiar with the principles of palliative care30 and should not neglect hospice referral for patients with advanced kidney failure.
Preparation for Kidney Failure (CPG 1.1)
Timely Education in Stage 4 CKD
Timely patient education as CKD advances can both improve outcomes and reduce cost.31 Planning for dialysis therapy allows for the initiation of dialysis therapy at the appropriate time and with a permanent access in place at the start of dialysis therapy. Planning for kidney failure should begin when patients reach CKD stage 4 for several reasons. The rate of progression of kidney disease may not be predictable. There is substantial variability in the level of kidney function at which uremic symptoms or other indications for dialysis appear. Patients vary in their ability to assimilate and act on information about kidney failure. Local health care systems vary in the delays associated with patient education and scheduling of consultations, tests, and procedures. Results of access creation procedures vary, and the success or failure of a procedure may not be certain for weeks or months. Timely education will: (1) allow patients and families time to assimilate the information and weigh treatment options, (2) allow evaluation of recipients and donors for preemptive kidney transplantation, (3) allow staff time to train patients who choose home dialysis, (4) ensure that uremic cognitive impairment does not cloud the decision, and (5) maximize the probability of orderly and planned treatment initiation using the permanent access.
Predialysis education to inform the patient and support persons about the relative value of various renal replacement modalities offers a freedom of choice that must be honored. Education and choice of modality also are vital to the timely placement of vascular or peritoneal access, training for home dialysis, and actual timing of the initiation of the selected first modality. A comprehensive preemptive discussion of these issues will enable patients and their support groups to make rational decisions and will serve to involve patients as active participants in their personal health care. Playing an active role in one's own health care, although thwarting the natural defense mechanism of denial, reduces risks from negligence and psychological depression that have been associated with poor outcomes after dialysis therapy is started.32
Contingency Plans
Optimal timing of vascular access creation may depend on plans regarding transplantation and/or PD treatment. Early attempts at native vein arteriovenous (AV) fistula creation are particularly important in patients who are: (1) not transplant candidates or (2) lack potential living kidney donors and also seem unlikely to perform PD. For patients hoping to undergo “preemptive” transplantation, thus avoiding dialysis treatment, the decision about whether to attempt AV fistula creation at CKD stage 4 (and, if so, when in stage 4) depends on the nephrologist's estimate of the likelihood that preemptive transplantation will be accomplished. For patients interested in performing PD, the decision about whether to attempt AV fistula creation at CKD stage 4 depends on the nephrologist's estimate of the probability that PD will be successful. The benefits of planning for kidney failure treatment are reflected in the literature comparing the consequences of early and late referral of patients with CKD to nephrologists.33-36
Education of Health Care Providers and Family Members
Optimally, education in preparation for kidney failure will include not only the patient, but also other individuals who are likely to influence his or her decisions. These may include family, close friends, and primary care providers. Their understanding of such issues as the impact of interventions designed to slow progression, the absence of symptoms despite underlying kidney disease, transplantation eligibility, the choice between PD and HD, and the choice and timing of vascular access may have critical consequences for the patient.
Estimation of Kidney Function (CPG 1.2)
Use of GFR-Estimating Equations and Clearances Rather Than Serum Creatinine to Guide Dialysis Initiation
Variability in creatinine generation across the population makes serum creatinine level alone an inaccurate test for patients with kidney failure likely to benefit from dialysis treatment. For most patients in CKD stages 4 and 5, estimating equations based on values of serum creatinine and other variables approximate GFR with adequate accuracy. For most patients, measured clearance does not offer a more accurate estimate of GFR than prediction equations.37
Variation in Creatinine Generation
It is well established that creatinine generation may be unusually low in patients with a number of conditions and may be increased in individuals of unusually muscular habitus (Table 2). In these situations, GFR estimated by using creatinine and urea clearances may be substantially more accurate (compared with radionuclide GFR) than results of creatinine-based estimating equations. In patients for whom endogenous creatinine generation is likely to be unusually low or high, GFR should be estimated by using methods independent of creatinine generation, such as measurement of creatinine and urea clearances.
Variation in Tubular Creatinine Secretion
Several drugs are known to compete with creatinine for tubular secretion, and advanced liver disease has been associated with increased tubular creatinine secretion (Table 3). Decreased secretion will result in artifactually low GFR estimates, and increased secretion will result in overestimation of GFR by means of estimating equations. In patients for whom tubular creatinine secretion is likely to be unusually low or high, the consequent bias to all creatinine-based measures should be considered in interpreting GFR estimates.
Timing of Therapy (CPG 1.3)
Initiation of Kidney Replacement Therapy
This guideline is based on the assumption that overall kidney function correlates with GFR. Because the kidney has many functions, it is possible that 1 or more functions will decrease out of proportion to the decrease in GFR. Therefore, caregivers should be alert to signs of declining health that might be directly or indirectly attributable to loss of kidney function and initiate kidney replacement therapy (KRT) earlier in such patients. However, they should consider that dialysis therapy is not innocuous and does not replace all functions of the kidney and that HD-related hypotension may accelerate the loss of RKF. This may particularly be true of HD.
Individual factors—such as dialysis accessibility, transplantation option, PD eligibility, home dialysis eligibility, vascular access, age, declining health, fluid balance, and compliance with diet and medications—often influence the decision about the timing of when to start dialysis therapy. It may be optimal to perform kidney transplantation or begin home dialysis before patients reach CKD stage 5. Even when GFR is greater than 15 mL/min/1.73 m2, patients may have a milder version of uremia that may affect nutrition, acid-base and bone metabolism, calcium-phosphorus balance, and potassium, sodium, and volume homeostasis. Conversely, maintenance dialysis imposes a significant burden on the patient, family, society, and health system. This is complicated further by the potential risks of dialysis therapy, especially those related to dialysis access and dialysate. These considerations necessitate conservative management until GFR decreases to less than 15 mL/min/1.73 m2, unless there are specific indications to initiate dialysis therapy. Thus, the recommended timing of dialysis therapy initiation is a compromise designed to maximize patient QOL by extending the dialysis-free period while avoiding complications that will decrease the length and quality of dialysis-assisted life.
Theoretical considerations support initiation of dialysis therapy at a GFR of approximately 10 mL/min/1.73 m2, and this was the recommendation of the 1997 NKF KDOQI HD Adequacy Guideline.38-40 In 2003, mean estimated GFR at the initiation of dialysis therapy was 9.8 mL/min/1.73 m2. This mean value reflects lower average values (~7 to 9 mL/min/1.73 m2) for young and middle-aged adults and higher average values (~10 to 10.5 mL/min/1.73 m2) for children and elderly patients. Average GFR at initiation has increased in all age groups since 1995; it has increased most in the oldest patients.41
It is difficult to make a recommendation for initiating KRT based solely on a specific level of GFR. Several studies concluded that there is no statistically significant association between renal function at the time of initiation of KRT and subsequent mortality.42-45 However, others suggested that worse kidney function at initiation of KRT is associated with increased mortality or morbidity.40-46 When corrections are made for lead-time bias, there is no clear survival advantage to starting dialysis therapy earlier in comparative outcome studies of patients initiating dialysis therapy at higher versus lower GFRs.47-48
Furthermore, it now is clear from observational registry data from the United States, Canada, and the United Kingdom48A that patients with comorbidities initiate dialysis therapy at higher levels of estimated GFR.41,49,50 It is reasonable to assume that this practice is based on experience and the speculation, hope, and/or impression that dialysis therapy may alleviate or attenuate symptoms attributed to the combination of the comorbidity plus CKD. Because symptoms of early uremia are fairly nonspecific, one can expect that patients with symptoms associated with their comorbidities would initiate dialysis therapy early. Healthy and hardy patients with less comorbidity likely will develop symptoms at a later stage than a frailer, early-starting comparative group. Frail patients who start dialysis therapy earlier do not live as long as hardy patients who start dialysis later. However, this remains merely an interpretation of observational data. A more definitive answer may emerge from properly designed prospective trials. One such trial expects to report in 2008. The Initiating Dialysis Early and Late (IDEAL) Study from New Zealand and Australia is a prospective, multicenter, randomized, controlled trial (RCT) to compare a broad range of outcomes in patients starting dialysis therapy with a Cockcroft-Gault GFR of 10 to 14 versus 5 to 7 mL/min/1.73 m2.51
In 2000, the NKF KDOQI CPG on Nutrition in CKD advocated that—in patients with CKD and estimated GFR less than 15 mL/min/1.73 m2 who are not undergoing maintenance dialysis—if: (1) protein-energy malnutrition develops or persists despite vigorous attempts to optimize protein-energy intake, and (2) there is no apparent cause for it other than low nutrient intake, initiation of KRT should be recommended.52 Furthermore, those guidelines set forth measures for monitoring nutritional status and identifying its deterioration. Those guidelines are consistent with the present recommendations.
Individuals vary tremendously in the physiological response to uremia and dialysis treatment. Patients expected to experience uremic complications often survive much longer than the physician anticipates, without apparent adverse consequences. Patients also vary in their willingness and ability to adhere to a medical regimen intended to forestall the need for dialysis treatment. Health care systems and providers vary greatly in their capability to monitor patients with advanced kidney failure safely without dialysis treatment. At best, the decision to initiate dialysis treatment or perform preemptive transplantation represents a joint decision by patient and physician, reflecting their mutual understanding of the compromises and uncertainties. It requires clinical judgment based on clinical experience.