There is ample evidence in the non-CKD population that optimal control of blood pressure influences mortality. In the HD population, available evidence indicates that control of a patient's fluid volume influences outcome. Volume and blood pressure are linked; thus, it is important to optimize ultrafiltration and dry weight to control blood pressure in an effort to improve patient outcome.
5.1 The ultrafiltration component of the HD prescription should be optimized with a goal to render the patient euvolemic and normotensive. This includes counseling the patient on sodium and fluid restriction, adequate ultrafiltration, and the use of diuretics in patients with RKF. (A)
5.2 Daily dietary sodium intake should be restricted to no more than 5 g of sodium chloride (2.0 g or 85 mmol of sodium). (A)
5.3 Increasing positive sodium balance by “sodium profiling” or using a high dialysate sodium concentration should be avoided. (B)
RATIONALE
The volume status of a maintenance dialysis patient is mainly a function of sodium intake, water intake, urine output, and removal of excess fluid by ultrafiltration during dialysis. Because cellular membranes are freely permeable to water, the osmotic gradient generated by the addition of dietary sodium to the ECF compartment causes water to move from cells into the ECF space, thus expanding ECF volume at the expense of the intracellular fluid compartment. The increase in ECF osmolality stimulates the thirst center of the hypothalamus, increasing water intake. Thus, the combined influence of both positive sodium and water balances causes expansion, primarily of the ECF volume.108 Such volume expansion can be especially marked in dialysis patients with poor RKF.
Poor volume control can exacerbate hypertension and its myriad detrimental effects on the cardiovascular system.109-112 Early reports of risks associated with excessive sodium and water were inconclusive, but analysis of USRDS Waves 3 and 4, when adjusted for comorbidity, showed that weight gain between dialyses of more than 4.8% (ie, 3.4 kg in a 70 kg person), a reflection of excessive sodium and water intake, is associated with increased mortality.113 Although a precise definition of dry weight is not possible in each patient, methods have been described for controlling volume and blood pressure and are reviewed here. A thorough examination of the approach to deriving a true “dry” weight is beyond the scope of the Work Group. The reader is referred to standard dialysis texts for detailed information.
Achievement of Optimal “Dry” Weight (CPG 5.1)
A patient's true dry weight, defined as the weight when fluid volume is optimal, can be determined accurately, but the method is not readily available in clinical settings (eg, use of multiple-frequency bioimpedance spectroscopy).114 Instead, dry weight usually is determined clinically by evaluating level of blood pressure, evidence of fluid overload, and the patient's tolerance of ultrafiltration aimed to arrive at the estimated target weight.115 It should be noted that a patient can have fluid excess in the absence of gross clinical evidence of volume expansion,116 a phenomenon termed “silent overhydration.”117 During dialysis, as the patient's dry weight is approached, the rate at which the vascular compartment refills from fluid in the adjacent tissue spaces is reduced.118 If UFR is reduced toward the end of dialysis, the reduced compensatory refilling process may be adequate to support the patient's depleted blood volume, thereby avoiding hypotension and muscle cramping. When the blood volume is refilled and blood pressure improves, more rapid ultrafiltration can be resumed. For a fluid-overloaded dialysis patient, this step-by-step process of identifying, or “probing,” for the true dry weight through ultrafiltration—but without inducing hypotension—should be accomplished gradually over a number of dialysis treatments (usually over 4 to 12 weeks, but it may require as long as 6 to 12 months) until evidence of fluid overload is in abeyance.119-121 For patients with diabetes mellitus (autonomic dysfunction) or cardiomyopathy, this process of approaching the dry weight may take longer because plasma refilling can be low even in the presence of an expanded volume.
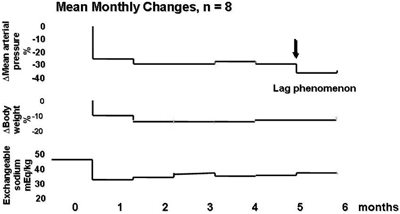
From the very beginning of the dialysis therapy, concomitant with ultrafiltration probing, dietary sodium should be restricted and use of a high dialysate sodium concentration and sodium profiling should be avoided. While decreasing the patient's fluid volume, net fluid losses ideally should not exceed 1 to 2 kg/wk, and by restricting dietary sodium and fluid intake, weight gain between dialyses should not exceed 1 kg during the week and 1.5 to 2 kg during the weekend.121 It should be noted that during this dry weight–probing stage, in 90% of patients, ECF volume becomes normal within a few weeks, but the elevated blood pressure continues to decrease for another 8 months or longer. See Fig 5 for a description of this “lag phenomenon.”122-125 As patients lose excess fluid and their hypertension improves, therapy with antihypertensive medications can be systematically tapered or discontinued.121
Fig 5. Illustration of the “lag phenomenon.” The secondary decrease in blood pressure seen at 5 months unassociated with a change in ECV was observed in all 8 patients studied. Reprinted with permission.125
Tolerance to ultrafiltration varies among patients. The slow approach to achievement of dry weight is appropriate for most patients, but for patients with cardiac failure or severe complication-associated hypertension, more aggressive ultrafiltration may be required acutely.126 Some patients may require slow ultrafiltration during a longer time than 4 hours 3 times weekly.115 To improve fluid removal during dialysis and reduce morbidity, monitoring blood volume during HD has been recommended. However, use of monitoring devices has met with varying degrees of success; some investigators have obtained satisfactory results,127-130 whereas other have had disappointing results.131 Further studies are required to clarify this important issue.
Hypotension during dialysis has many adverse effects and potential life-threatening consequences. By impairing tissue perfusion, low blood pressures can compromise dialysis adequacy.132 Hypotension induced by overzealous ultrafiltration also may contribute to loss of RKF and, in predisposed patients, coronary and/or cerebral ischemia.121 To avoid hypotension, dry weight should be systematically reevaluated after each dialysis treatment. It was suggested that a dialysis log summarizing the relevant information, such as body weights, blood pressures, and intradialytic incidents, is essential to provide a longitudinal dynamic view of ECF volume and blood pressure changes.133 Dry weight may change, for example, when a newly dialyzed patient becomes less uremic, regains appetite, and gains muscle and nonfluid weight (reflected by an increase in serum creatinine level), or when a patient has an intercurrent illness and loses muscle and tissue weight.
Hypertension: Prevalence, Pathogenesis, and Risks (CPG 5.1)
It is noteworthy that 60% to 90% of maintenance HD patients have hypertension.41,109,134-138 Despite the use of multiple medications, hypertension in these patients often is poorly controlled.109,111,124,136,139 For example, among the first 1,238 maintenance HD patients enrolled in the HEMO Study, less than 30% had blood pressures that were considered normotensive by the Joint National Committee (JNC) VI standards.111 In another study of 2,535 clinically stable adult HD patients, 86% were found to be hypertensive. Within this hypertensive group, only 30% had their blood pressure under adequate control, 58% were inadequately treated, and 12% were not treated at all.109
With regard to the pathogenesis, it generally is recognized that the majority of hypertensive HD patients develop hypertension because of fluid overload secondary to sodium and water retention.123,133,140-142 A high predialysis or interdialysis blood pressure may be related to excessive sodium and water ingestion during the interdialysis period,126,136 a high dialysate sodium level,143,144 or sodium profiling,145 whereas a high postdialysis blood pressure may reflect inadequate achievement of dry weight.113,146 There may be exceptions to these simple explanations of the effects of sodium and water retention on a patient's blood pressure. For example, blood pressures in a small number of patients with CKD stage 5 were found to respond less readily compared with the majority when challenged with similar degrees of fluid retention.112,134 Conversely, reduction of fluid excess in a hypervolemic and hypertensive dialysis patient may not bring about a prompt decrease in blood pressure until ECV is less than a certain threshold value. These clinical observations suggest that the relationship between ECV and blood pressure in some patients may be sigmoidal, rather than linear, and that volume overload leads to an increase in blood pressure only when physiological autoregulation can no longer cope with the fluid excess.147
For some patients, the conventional dialysis time is too short for their ultrafiltration requirements to be readily fulfilled. Attempts to accelerate ultrafiltration in these patients may precipitate hypovolemia and hypotension. Normal saline frequently is administered and ultrafiltration is slowed or discontinued, at least temporarily. As a consequence, at the end of the dialysis session, not only has the originally targeted fluid excess not been removed, but the infused saline also has expanded ECV further. More sodium and water will accumulate during the succeeding interdialysis period, contributing further to a chronic state of baseline volume expansion in association with persistent hypertension.
It should be noted that each 10 mm Hg increase in mean arterial blood pressure is correlated independently with the development of progressive concentric LVH, de novo ischemic heart disease, and de novo congestive cardiac failure.148 The leading cause of death in maintenance HD patients is CVD,149 which is responsible for at least 50% of HD deaths in the United States.112 Apart from fluid overload, there are other significant pathogenic factors for hypertension in dialysis patients,150 such as arterial stiffness151,152 caused by arteriosclerosis, salt-related reduction in nitric oxide formation,153-155 sympathetic nervous system overactivity,156 activation of the renin-angiotensin system,157 presence of other vasoconstrictors,126 lack of vasodilators,126 erythropoietin therapy,158 genetic predisposition,112 and other as yet poorly defined causes. Although it is generally recognized that hypertension requires control in hypertensive dialysis patients,110,147,159,160 the ideal target blood pressure is unknown at present.161 In patients with reduced vascular and cardiac compliance, blood pressure goals may need to be higher. Vigorous contraction of plasma volume in such patients should be avoided to allow adequate tissue perfusion during ultrafiltration when hypotension is prone to occur.161 However, some have recommended that attempts be made to decrease these high pressures as much as possible to achieve optimal survival.162 Finally, some dialysis patients with low predialysis blood pressures also have a high mortality rate.148,163,164 Risk for death in these patients may reflect cardiac failure, coronary artery disease, malnutrition, inadequate dialysis, or other serious illnesses that can decrease blood pressure.110,161,165 It is likely that the cardiovascular problems in some of these patients result from poorly treated prior hypertension. Thus, there is every incentive to control blood pressure as early as possible before cardiac damage leads to permanent hypotension and an almost certain early death.166
In a small number of patients, blood pressure paradoxically increases after dialysis. The mechanism of this elevation is not fully understood.147 Some hypertensive patients for whom blood pressure increases while fluid is removed during dialysis may respond to still more fluid removal by undergoing repeated isolated ultrafiltration sessions, with eventual better blood pressure control.167 However, attempts to remove excess fluid from these patients by using ultrafiltration should be conducted with special care.147
Recommended Sodium Intake (CPG 5.2)
The normal daily sodium chloride intake in the United States varies from 5.8 to 17.4 g (2.3 to 6.9 g [100 to 300 mmol] of sodium),168 while both the American Heart Association169,170 and Institute of Medicine171 recommend a daily tolerable upper intake level for sodium chloride of no more than 5.8 g (2.3 g [100 mmol] of sodium) for the average healthy adult. The Institute of Medicine also recommends that because older individuals, African Americans, and people with chronic diseases, including hypertension, diabetes, and kidney diseases, are especially sensitive to the blood pressure–increasing effects of salt, they should consume less than the tolerable upper intake level. The European Society of Hypertension and European Society of Cardiology recommend a daily sodium chloride intake of 4.7 to 5.8 g (1.8 to 2.3 g [80 to 100 mmol] of sodium) for patients with arterial hypertension.172 Finally, use of a low-sodium chloride diet, namely, less than 5.8 g (2.3 g [100 mmol] of sodium) also was found to decrease blood pressure in individuals without hypertension.173
Thus, the daily sodium chloride intake suggested for dialysis patients (namely, no more than 5 g [ie, 2.0 g [85 mmol] of sodium]) is consistent with recommendations for healthy adults by US health research groups and for patients with essential hypertension by European health organizations. It also is recommended for dialysis patients by various investigators.133,141,174-176 A 5-g sodium chloride diet in a 70 kg anuric compliant patient should bring about a 1.5-kg average interdialysis weight gain on a conventional thrice-weekly regimen.141 Most dialysis patients should be able to tolerate this degree of ultrafiltration requirement. A more stringent daily sodium chloride limitation amounting to 2.5 to 3.8 g (1 to 1.5 g [43 to 65 mmol] of sodium) has been recommended for hypertensive dialysis patients.121,126 In patients who happen to lose appreciable amounts of sodium through either RKF or extrarenal routes, sodium restriction can be modified and tailored to those losses. Patients who are accustomed to a more liberal sodium intake might lose their appetites and become malnourished if sodium restriction is instituted too abruptly and too strenuously. In such patients, sodium limitation can be introduced gradually to provide ample time for taste adjustments. Most patients find that they do not miss the sodium if they cut back gradually.176A For patients who cannot tolerate sodium restriction at all, to combat sodium and water excess, more prolonged and/or more frequent dialysis treatments (including periodic isolated ultrafiltration) may be required (see Prolonging Dialysis Treatments).
When observing a low-sodium diet, in addition to refraining from adding salt during cooking and at the dining table, canned, processed, and salty-tasting food should be avoided.172,175 A low-sodium diet does not equate to tasteless food. Many varieties of flavor enhancers are available to make food more appealing and palatable.143 Moreover, after exposure to salt restriction for 8 to 12 weeks, the appeal of low-sodium foods in both normotensive and hypertensive individuals is enhanced.177 Sodium restriction does not require a reduced intake of other essential nutrients.178
Sodium Restriction and Blood Pressure Control (CPG 5.2)
That excessive sodium intake can aggravate hypertension and adequate sodium restriction can prevent or ameliorate hypertension is well known.169 As early as the middle of the last century, limiting daily sodium intake of non-CKD hypertensive patients with a rice and fruit diet was shown to reduce ECF volume and blood pressure during a period of weeks as excess sodium was excreted in urine.179 This observation pertaining to the benefit of sodium limitation may relate to the rarity of hypertension among individuals of populations living in very remote areas who consume a low-sodium diet (median daily intake, 17 to 51 mmol).180
Among dialysis patients, myriad observational and interventional studies of patients with CKD have shown that restricting sodium intake is an essential tool for volume and blood-pressure control.124,125,140,141,165,175,181-192 Apart from its effect in nonuremic hypertensive patients, a sodium-poor rice and fruit diet also was shown to improve the hypertension of patients with renal failure.193,194 These observations echo those in PD patients, for whom decreasing sodium in the diet is crucial for the achievement of dry weight and effective control of blood pressure.195
Since infancy, most of us are accustomed to consuming a larger quantity of salt than we need.196 Restricting salt intake in HD patients is tantamount to requiring them to change their customary lifestyle. Changing one's lifestyle is always a difficult undertaking. However, moderating one's sodium intake is a small price for a patient with CKD to pay if one wishes to avoid the devastating effects of relentless excess sodium and water accumulation on morbidity and mortality.
Prolonging Dialysis Treatments
Elevated blood pressures can be decreased satisfactorily with aggressive ECF volume control, achieved by limiting sodium intake and performing adequate ultrafiltration.182 Success using this strategy has been reported in studies from Tassin, France, showing that hypertension is improved substantially with a combination of dietary sodium limitation (85 to 100 mmol/d of sodium) and dialyzing slowly for 8 hours 3 times per week.197 Sodium limitation decreased patients' average weight gain between dialyses to 1.7 kg, less than 3% of mean BW.133 Both the limited weight gain (ie, ultrafiltration requirement) and long period of ultrafiltration combined to ensure that symptoms during dialysis were minimized and dry weight was achieved.133 Upon initiation of HD treatments, 89% of patients were hypertensive despite therapy with antihypertensive medications. However, after 3 months of the described strategy, only 5% of those patients still required the use of such medications.197 Of course, because the Tassin patients were dialyzed longer than patients treated with a conventional regimen, it could be argued that these patients fared better because they had better removal of small and middle molecules, improved nutrition, and better phosphate control. However, a comparison study of mortality rates in conventionally dialyzed patients from Nottingham, United Kingdom, concluded that the improved control of blood pressure was the most likely and predominant cause of better results shown by the Tassin patients.198
It should be noted that adequate control of blood pressure as a consequence of dietary sodium restriction (<100 mmol/d of sodium) and appropriate ultrafiltration with175 or without185,199 a low-sodium dialysate (135 mmol/L) also was shown in patients treated with a conventional thrice-weekly (4 to 5 hours per treatment) dialysis regimen. In addition to blood pressure control, patients also showed regression of LVH and a decrease in left atrial and left ventricular systolic and diastolic pressures.185,199
For conventionally dialyzed patients (3 sessions per week, ≤4 hours per session) who are still overloaded despite maximally tolerable ultrafiltration, the recently proposed: (1) short-daily (2 to 3 hours for each treatment, 6 or 7 treatments per week) regimen;200-202 (2) long (8 hours for each session) nocturnal thrice-weekly regimen;197,203 and (3) long (8 hours for each session) nocturnal (6 to 7 nights per week) regimen204,205 all were reported to remove excess fluid and improve hypertension satisfactorily.110 A longer weekly treatment time (5 hours per session, 3 times per week) also was shown to cause less hypotension during dialysis and less postdialysis postural hypotension compared with its shorter counterpart (4 hours per session, 3 times per week).206 Alternatively, periods of isolated ultrafiltration can be added to a standard treatment regimen.199
Dietary Water Restriction
When a patient is advised to restrict sodium intake, does he or she need to be advised to limit water intake too? It was suggested that attempts at water restriction commonly are futile if sodium limitation is not observed simultaneously. Reducing a patient's water intake alone is not prudent most of the time because the increased ECF osmolality brought about by the excessive sodium ingestion stimulates thirst, followed by water consumption and hence isotonic fluid gain.207,208 Advising patients to limit their water intake without curtailing their sodium intake will cause suffering from unnecessary thirst. Some of these patients may even feel guilty if they fail to resist the urge to drink in the face of marked thirst.143 However, although excessive water intake accompanies the ingestion of excess salt, other factors can have a role in stimulating drinking. Such factors include hyperglycemia, elevated blood angiotensin levels, and ingestion of such drugs as clonidine.209 Thus, to ensure complete safety, patients should be watched carefully to make sure they do not accumulate more fluid than recommended.
Pathogenesis of the Lag Phenomenon
The exact mechanism responsible for the lag phenomenon is still not fully understood.122,125,174 Its occurrence may be related to the appearance of lower peripheral vascular resistance caused by relaxation of endothelial smooth muscle.174 In this regard, it was shown that p38 mitogen-activated protein kinase (p38MAPK) promotes the formation of asymmetric dimethylarginine (ADMA). The latter, in turn, can inhibit the action of nitric oxide synthase and hence the production of nitric oxide. Sodium chloride was suggested to bring about p38MAPK release and hence ADMA synthesis.153 The consequent decrease in endothelial nitric oxide formation leads to failure of arteriolar muscle to relax. It should be noted that high ADMA concentrations have been found in plasma of patients with CKD stage 5.154,155 In recent studies involving experimental animals with chronic renal failure, high sodium chloride intake decreased nitric oxide synthase expression in certain areas of the brain, resulting in activation of the sympathetic nervous system and hypertension.210 In addition, there is evidence that sodium overload may cause reversal of the inhibition of Na+, K+-ATPase through endogenous ouabain. This step would bring about an increase in intracellular sodium and calcium concentrations, subsequently causing an increase in vascular tone and blood pressure.211 Sodium restriction should lead to the opposite effects. The contention that sodium limitation can cause vascular relaxation is consistent with the observation that long-term dialysis patients maintained for years on a low-salt diet have peripheral vascular resistance that is lower than that of healthy controls.212 Thus, it is entirely possible that sodium restriction may work in ways other than that of simple ECF volume contraction.
Use of Diuretics
To promote loss of sodium and water from dialysis patients, large doses of potent loop diuretics, such as furosemide, bumetanide, or torsemide, can be administered.213-216 However, diuretic therapy is effective only when RKF is high enough to provide daily urine output of at least 100 mL.217 The effectiveness of this therapy may not last long,209 possibly because of a further inevitable decline in renal function. Loop diuretics should be used with caution because of the possibility of ototoxicity.218,219 The incidence of ototoxicity appears to be greater with furosemide and much less with bumetanide or torsemide.213,214
Dialysate Sodium Concentration (CPG 5.3)
High concentrations of sodium in dialysate reduce the removal of sodium during dialysis and ultrafiltration.143,144 In the 1960s, when a dialysis treatment typically lasted 6 hours, dialysate sodium levels were in the realm of 135 mmol/L.144 However, since the early 1970s, with the advent of shorter treatments (3 times per week for ≤4 hours per treatment), removal of the required amount of excess fluid became more difficult. To overcome this difficulty, it became necessary to increase dialysate sodium to a greater concentration (eg, to the region of ≥140 mmol/L in the 1990s).143,220 Although increasing dialysate sodium concentration can decrease morbidity both during and between treatments, such dialysates can aggravate thirst, fluid gain, and hypertension.143,144,220,221 Similar consequences were found in patients treated with sodium profiling, a technique that increases dialysate sodium concentration early in treatment (eg, 145 to 155 mmol/L), followed by a progressive decrease (linear, step, or logarithmic) to a lower value (eg, 135 to 140 mmol/L) at the end of dialysis.145 It should be noted that the patient's postdialysis serum sodium concentration is a function of the time-averaged dialysate level, not the terminal level of sodium in dialysate.222 Reviews of the large volume of literature on this topic showed that sodium profiling is of uncertain benefit.144,145,223 Some investigators had satisfactory experiences with a dialysate sodium concentration of 138 mmol/L in a large number of patients. During these studies, the dosage of antihypertensive medications often had to be decreased or discontinued.
Use of appropriate ultrafiltration techniques, dietary sodium restriction, and lower dialysate sodium concentrations160,224 has been instrumental in attaining a true dry weight and amelioration of hypertension in many maintenance HD patients.133 Reembracing the time-honored and useful, yet inexpensive, tool of dietary salt restriction should serve to promote the health of HD patients. During the process of controlling ECF volume and decreasing predialysis weight, the development of hypotension during dialysis or hypertension between dialysis treatments should not be construed as a failure of volume control to normalize blood pressure. The lag phenomenon noted previously should be taken into consideration when evaluating patients with persistent hypertension.112 To more easily control hypertension in most dialysis patients, use of a high dialysate sodium concentration and sodium profiling should be discouraged.
Finally, application of appropriate ultrafiltration with every dialysis treatment, the incessant vigilance to target and subsequently to maintain a true dry weight (which is subject to change because of loss or gain of nonfluid body tissue), and confirmation that a patient is compliant with a sodium-restricted diet combine to demand a considerable amount of time from members of the health care team. However, to obtain favorable results, an intense, totally committed, and prolonged effort—with a high degree of motivation—is required from caregivers, as well as from the patients themselves.112