Several actions and precautions are recommended to preserve and enhance RKF.
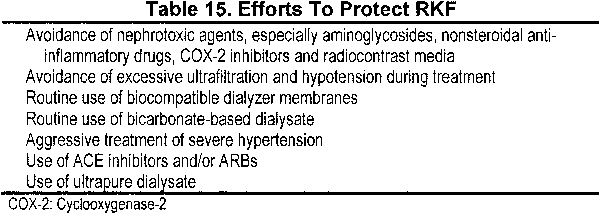
6.1 Angiotensin-converting enzyme (ACE) inhibitors and/or angiotensin receptor blockers (ARBs) are agents of choice in HD patients with significant RKF and who need antihypertensive medication. Other measures to protect native kidneys are listed in Table 15.
6.2 Insults known to be nephrotoxic (eg, see Table 16) in patients with normal or impaired kidney function should be assumed, in the absence of direct evidence, to be nephrotoxic for the remnant kidney in HD patients and therefore should be avoided.
6.3 Prerenal and postrenal causes of decrease in RKF should be considered in the appropriate clinical setting.
Although the contribution of RKF to survival is well documented for patients managed with PD, the impact is less clear for those requiring HD. Most studies assumed that RKF is negligible and report survival as a function of delivered Kt/Vurea, ignoring the potential benefits associated with RKF. However, recent data support the notion that RKF is an important predictor of survival and delivered Kt/Vurea can be adjusted to reflect the presence of renal function.81,230
RKF is an important contributor to dialysis adequacy, and adequacy was shown to impact on morbidity and mortality in patients with CKD stage 5.53 In contrast to HD, RKF provides continuous clearance of both small and large solutes and helps attenuate the large fluctuations in fluid balance and blood pressure that are more pronounced in anuric patients. Urine volume permits more fluid and potassium intake, relaxing overall dietary restrictions and reducing the fluctuations in body fluid volumes between dialysis treatments that contribute to volume overload syndromes, hypertension, and cardiac hypertrophy.351 Preservation of residual renal mass also has the potential to provide beneficial endocrine and potentially other functions that are not yet discovered.
To measure RKF, Kr can be calculated from a 24-hour urine collection for urea clearance. As for PD, 24-hour urine collections should be obtained at least every 4 months or when a decrease in RKF is suspected (eg, decreasing urine output or recent exposure to a nephrotoxin). Precautions and actions that have been recommended to preserve RKF are listed in Table 15.
The nephrotoxic insults listed in Table 16 are well known to cause injury to normal kidneys and kidneys damaged by a variety of diseases. It is reasonable to presume that these insults also are harmful to the remnant kidney and should be avoided if RKF is to be preserved for as long as possible. Please refer to the Guideline for Preservation of RKF in PD patients in the NKF KDOQI PD Adequacy Guidelines for further discussion of this topic.
Episodes of intravascular volume depletion that frequently occur during HD probably contribute to more rapid loss of RKF; therefore, efforts to maintain hemodynamic stability should be routine. Strategies to minimize hypotension during HD include avoidance of excessive ultrafiltration, maintaining the target hematocrit, reduction in dialysate temperature, increasing dialysate sodium concentration, and predialysis administration of an agonist, such as midodrine. Avoidance of hypotension also helps ensure delivery of adequate dialysis and minimize symptoms during HD. Paradoxically, loop diuretics, which are implicated as a cause of worsening renal function when used overzealously in patients with CKD, probably benefit HD patients because they reduce the requirement for fluid removal during dialysis.
The more prolonged preservation of RKF in HD patients observed in more recent years has been attributed to numerous factors, including more widespread use of biocompatible membranes, high-flux dialysis, and use of bicarbonate instead of acetate buffers. There is general disagreement about which of these factors, if any, plays a role (Table 17). A recent prospective randomized study suggested that ultrapure water, when combined with high-flux dialysis, may benefit native kidney function.232,352 Another study of high-flux biocompatible membranes with bicarbonate buffer and ultrapure water showed a decrease in RKF similar to that in a contemporary group of CAPD patients.229 The more prolonged exposure to membranes during nocturnal and daily-dialysis regimens hopefully will shed more light on membrane contributions.
Despite some early concerns about irreversible drug-induced renal disease,353 it is now generally accepted that the decrease in renal function observed in most patients treated with ACE inhibitors and ARBs is reversible and renoprotective, even in patients with CKD stage 5.230 However, the drug-induced decrease in GFR causes an increase in levels of BUN, creatinine, and other solutes and may decrease urine output; thus, consequences in HD patients are not all benign. Irreversible loss of renal function may occur in patients with ischemic renal disease treated with ACE inhibitors.
Severe hypertension is well known to damage normal kidneys acutely (malignant hypertension) and can cause ongoing damage over a period of years (hypertensive nephrosclerosis). In addition, most kidney diseases, especially those like diabetes that target the kidney vasculature or glomeruli, are exacerbated by hypertension. In some patients initiating HD therapy, the kidneys may have been damaged more acutely by severe hypertension. Control of hypertension after initiating dialysis therapy has been associated with improvement in RKF, sometimes allowing discontinuation of dialysis therapy.354 These patients should be identified from the beginning, and special attention should be given to controlling blood pressure for the purpose of preserving and possibly improving RKF.
The Work Group encourages PD as a first choice of modality for patients initiating KRT for reasons outlined in the NKF KDOQI PD Adequacy Guidelines, but also as a means of preserving RKF. However, most patients are not candidates for self-dialysis outside of a clinic; thus, HD remains the most common initial modality choice for new patients. The same attention that is given to RKF in PD patients should be directed to this much larger group of HD patients.
Use of the nephrotoxic agents listed in Table 16 is not always contraindicated because they may be required in special circumstances to relieve pain (eg, nonsteroidal anti-inflammatory drugs), treat a difficult problem (eg, ultrafiltration during dialysis), or complete a vital diagnostic test (eg, coronary angiogram).