Appropriate planning allows for the initiation of dialysis therapy at the appropriate time with a permanent access in place at the start of dialysis therapy.
1.1 Patients with a glomerular filtration rate (GFR) less than 30 mL/min/1.73 m2 (CKD stage 4) should be educated on all modalities of kidney replacement therapy (KRT) options, including transplantation, so that timely referral can be made for the appropriate modality and placement of a permanent dialysis access, if necessary. (A)
1.2 In patients with CKD stage 4 or 5, forearm and upper-arm veins suitable for placement of vascular access should not be used for venipuncture or for the placement of intravenous (IV) catheters, subclavian catheters, or peripherally inserted central catheter lines (PICCs). (B)
1.3 Patients should have a functional permanent access at the initiation of dialysis therapy.
- 1.3.1 A fistula should be placed at least 6 months before the anticipated start of HD treatments. This timing allows for access evaluation and additional time for revision to ensure a working fistula is available at initiation of dialysis therapy. (B)
- 1.3.2 A graft should, in most cases, be placed at least 3 to 6 weeks before the anticipated start of HD therapy. Some newer graft materials may be cannulated immediately after placement. (B)
- 1.3.3 A peritoneal dialysis (PD) catheter ideally should be placed at least 2 weeks before the anticipated start of dialysis treatments. A backup HD access does not need to be placed in most patients. A PD catheter may be used as a bridge for a fistula in “appropriate” patients. (B)
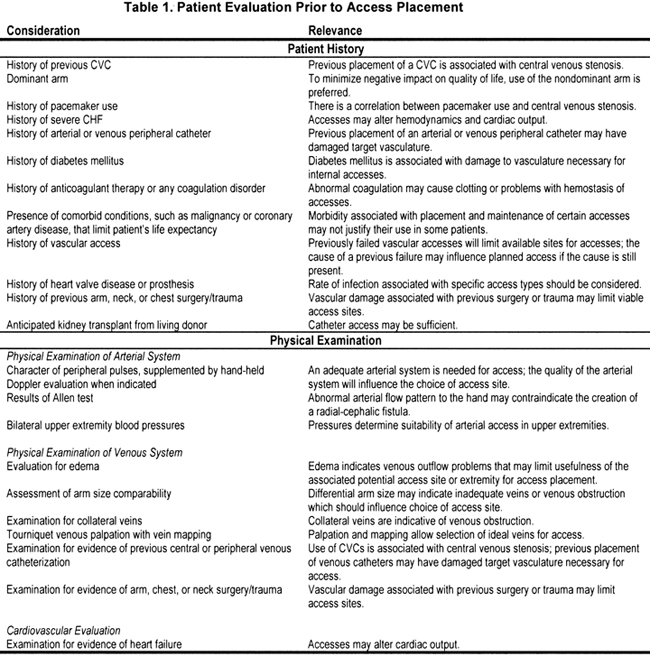
1.4 Evaluations that should be performed before placement of a permanent HD access include (Table 1):
- 1.4.1 History and physical examination, (B)
- 1.4.2 Duplex ultrasound of the upper-extremity arteries and veins, (B)
- 1.4.3 Central vein evaluation in the appropriate patient known to have a previous catheter or pacemaker. (A)
Since implementation of the NKF KDOQI Vascular Access Guidelines in 1997, which encouraged increased placement of fistulae, CMS has embraced this recommendation with the implementation of the Fistula First Breakthrough Initiative (FFBI). This initiative endorses the goals recommended by the NKF KDOQI: fistula rates of 50% or greater for incident—and at least 40% for prevalent—patients undergoing HD. The FFBI promotes the placement of fistulae in all suitable HD patients. Working through the ESRD Networks, the FFBI promotes the placement of fistulae using 11 “Change Concepts” that encourage the development of specific strategies; these 11 Change Concepts have been identified to help the kidney community improve the rate of fistula placement. Five of these strategies emphasize the same goals as CPG 1 and Clinical Practice Recommendation (CPR) 1: education of patients regarding fistulae, protection of vessels, vessel mapping, and sufficient lead-time for fistula maturation (NVAII; www.fistulafirst.org). The breakthrough initiative has reset the goal for fistula creation to 65% by 2009.
Characteristics of a patient's arterial, venous, and cardiopulmonary systems will influence which access type and location are most desirable for each patient.22-27 The patient's life expectancy and planned duration of CKD stage 5 therapy also can influence the type and location of the access. All patients should be evaluated as in Table 1.
Venipuncture complications may render veins potentially available for vascular access unsuitable for construction of a primary fistula. Patients and health care professionals should be educated about the need to preserve veins to avoid loss of potential access sites in the arms and maximize chances for successful fistula placement and maturation. Subclavian vein catheterization is associated with central venous stenosis.28-30 Significant subclavian vein stenosis generally will preclude the use of the entire ipsilateral arm for vascular access. Thus, subclavian vein catheterization should be avoided for temporary access in patients with kidney disease.31 The incidence of central vein stenosis and occlusion after upper-extremity placement of peripherally inserted long-term catheters (PICCs) and venous ports was 7% in 1 retrospective study of 150 patients.32 PICCs also are associated with a high incidence of upper-extremity thrombosis. The incidence of upper-extremity venous thrombosis varies between 11% and 85%, which leads to loss of potential upper-extremity fistulae.33-35 Because of the substantial risk for loss of useable upper-extremity veins and central venous stenosis with PICCs, the Work Group recommends strongly that PICCs not be used in patients with CKD.
Ideally, patients should have a functional permanent access at the time of dialysis therapy initiation. Function implies that the access not only delivers adequate blood flow for dialysis, but may be cannulated easily. In general, such an access has a flow of approximately 600 mL/min, is less than 0.6 cm below the surface of the skin, and has a minimal diameter of 0.6 cm (Rule of 6s) Both the size and anatomic qualities of venous and arterial components of primary fistulae can influence fistula maturation time. An aggressive policy of primary fistula creation may result in failures in patients with marginal anatomy. However, timely attempts to create a primary fistula before the anticipated need for dialysis therapy will allow adequate time for the fistula to mature and will allow sufficient time to perform another vascular access procedure if the first attempt fails, thus avoiding the need for temporary access. Early referral of a patient with CKD to a nephrologist is needed to facilitate CKD therapy with medications and diets that preserve kidney function. In addition, counseling patients about CKD stage 5 treatment options is essential to plan for ideal access (ie, PD and HD access) (see CPG 2) (Table 1).
The Work Group's consensus is that maturation of an AVG access site—defined as reduction of surgically induced swelling and the graft's adherence to its tunnel tissue—usually requires about 3 weeks. Thus, ideally, AVGs should be placed 3 to 6 weeks before use.
Long-term catheters are the method of choice for temporary access of longer than 1 week duration. Catheters are suitable for immediate use. To maximize their use-life, they should not be inserted until needed. However, the Work Group recommends that a catheter be used for dialysis access for as brief a period as necessary (see CPG 2).
A vein must be mature, both physically and functionally, before use for vascular access. The time required for fistula maturation varies among patients. The Work Group does not advise use of the fistula within the first month after construction because premature cannulation of a fistula may result in a greater incidence of infiltration, with associated compression of the vessel by hematoma and permanent loss of the fistula. In general, allowing the fistula to mature for 6 to 8 weeks before investigating the reason for failure to mature is appropriate (see CPG 2). For a fistula to be considered successful, it must be usable. In general, a working fistula must have all the following characteristics: blood flow adequate to support dialysis, which usually equates to a blood flow greater than 600 mL/min; a diameter greater than 0.6 cm, with location accessible for cannulation and discernible margins to allow for repetitive cannulation; and a depth of approximately 0.6 cm (ideally, between 0.5 to 1.0 cm from the skin surface). This combination of characteristics can be remembered easily as the Rule of 6s.
Although there are no definitive data in the literature, any intervention that increases blood flow to the extremity may improve the chances of successful fistula development. Therefore, regular hand-arm exercises, with or without a lightly applied tourniquet, are recommended until the fistula matures. Failure of a fistula to mature occasionally is caused by venous side branches that drain critical flow from the primary vessel. Ligating these side branches may result in successful maturation (see CPG 6).
Studies relating to preoperative venous imaging/mapping for AVF construction underwent systematic review. Duplex ultrasound is the preferred method for preoperative vascular mapping. Vascular mapping in preparation for the creation of a vascular access refers to the evaluation of vessels, both arterial and venous, of patients with CKD who have selected HD therapy, and it should be performed in all patients before placement of an access. Preoperative vascular mapping was shown to substantially increase the total proportion of patients dialyzing with fistulae.36-39 Several studies support the 2.0- to 2.5-mm vein diameter threshold for successful creation of a fistula.39,40 Radiocephalic fistulae constructed in veins less than 2.0 mm in diameter had only a 16% primary patency at 3 months compared with 76% for those with veins greater than 2.0 mm.40 In a pivotal study,39 a threshold of 2.5-mm vein diameter, assessed by using duplex ultrasound, was used; this resulted in an increase in fistula creation to 63% compared with a retrospective 14% rate in the absence of vascular mapping.22 A similar study using the same duplex ultrasound criteria showed a fistula increase from 34% in historical controls to 64%. Importantly, in this study, duplex ultrasound altered the surgical plan based entirely on the surgeon's clinical evaluation, resulting in increased placement of fistulae.41
There is no generally accepted “standard” for what constitutes vascular mapping. The arterial evaluation should include pulse examination, differential blood pressure measurement, assessment of the palmar arch for patency, arterial diameter assessed by using duplex ultrasound, and the presence of arterial calcification. A preoperative arterial diameter less than 1.6 mm has been associated with a high failure rate in radiocephalic fistulae.42,43 Other studies suggested that a minimum diameter of 2.0 mm is required for successful fistula creation.39 Venous evaluation should include a luminal diameter of 2.5 mm or greater, continuity with the proximal central veins, and absence of obstruction.39 The central veins may be assessed indirectly by using duplex ultrasound.44 Compared with invasive venography, duplex ultrasound had a specificity of 97% and sensitivity of 81% for detecting central vein occlusion.45 Alternatively, venography or magnetic resonance angiography (MRA) may be used to evaluate central veins.46 (See CPR 1.4 for suitable imaging studies for central veins).
There has been no study comparing vascular access surgery based only on the clinical evaluation to preoperative vascular mapping outcomes. Such a study would be the equivalent of requiring a randomized prospective study comparing the efficacy of pulmonary clinical evaluation (tactile fremitus and auscultation, ie, physical examination only) with a chest radiograph (imaging) in identifying lung pathological states. Such a study is unlikely, based on current data showing that vascular mapping increases fistula creation. Although the level of evidence of a prospective randomized trial is not available, the Work Group consensus based on many studies supports vascular mapping as a guideline.