The use of aseptic technique and appropriate cannulation methods, the timing of fistula and graft cannulation, and early evaluation of immature fistulae are all factors that may prevent morbidity and may prolong the survival of permanent dialysis accesses.
3.1 Aseptic techniques:
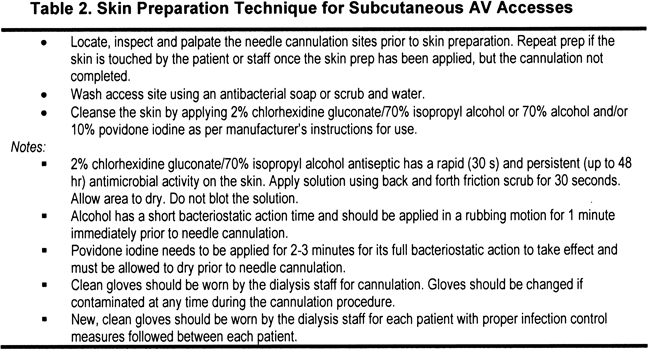
- 3.1.1 For all vascular accesses, aseptic technique should be used for all cannulation and catheter accession procedures. (See Table 2.) (A)
3.2 Maturation and cannulation of fistulae:
- 3.2.1 A primary fistula should be mature, ready for cannulation with minimal risk for infiltration, and able to deliver the prescribed blood flow throughout the dialysis procedure. (See Table 3.) (B)
- 3.2.2 Fistulae are more likely to be useable when they meet the Rule of 6s characteristics: flow greater than 600 mL/min, diameter at least 0.6 cm, no more than 0.6 cm deep, and discernible margins. (B)
- 3.2.3 Fistula hand-arm exercise should be performed. (B)
- 3.2.4 If a fistula fails to mature by 6 weeks, a fistulogram or other imaging study should be obtained to determine the cause of the problem. (B)
3.3 Cannulation of AVGs:
Grafts generally should not be cannulated for at least 2 weeks after placement and not until swelling has subsided so that palpation of the course of the graft can be performed. The composite PU graft should not be cannulated for at least 24 hours after placement and not until swelling has subsided so that palpation of the course of the graft can be performed. Rotation of cannulation sites is needed to avoid pseudoaneurysm formation. (See Table 4.) (B)
3.4 Dialysis catheters and port catheter systems:
Infection-control measures that should be used for all HD catheters and port catheter systems include the following:
- 3.4.1 The catheter exit site or port cannulation site should be examined for proper position of the catheter/port catheter system and absence of infection by experienced personnel at each HD session before opening and accessing the catheter/port catheter system. (B)
- 3.4.2 Changing the catheter exit-site dressing at each HD treatment, using either a transparent dressing or gauze and tape. (A)
- 3.4.3 Using aseptic technique to prevent contamination of the catheter or port catheter system, including the use of a surgical mask for staff and patient and clean gloves for all catheter or port catheter system connect, disconnect, and dressing procedures. (A)
There is considerable evidence that the use of maximal sterile precautions, as opposed to clean aseptic technique, for cannulation of AV accesses and catheter accession is both impractical and unnecessary.222-225 However, the importance of strict dialysis precautions226 and aseptic technique222 cannot be overemphasized in the prevention and minimization of all access infection.227 Despite the general acceptance of the importance of standard precautions for hand washing and glove changes, these simple acts to minimize transmission of disease frequently are skipped. An audit in a selection of Spanish HD units examined opportunities to wear gloves and wash hands per the standard preventive guidelines (high-risk activities of connection, disconnection, and contact between patients during dialysis). Gloves were worn by only 19% and hands were washed after patient contact on only 32% of all occasions.228 Mandatory hand washing before patient contact occurred only 3% of the time. A decade later, wearing of gloves improved to 92%, but the practice of hand washing before or after these patient-oriented procedures remained low at 36% after and 14% before such activities.229 Greater adherence was found in acute than in long-term HD units. A greater patient-nurse ratio independently influenced hand-washing rates. With the increasing microbial resistance to mainstream antibiotics,230 infection prevention must be considered the first rule of vascular access maintenance.231 Data from prospective studies in both Canada and the United States clearly show that great variability exists between centers in infection rates, indicating the need to have not only a national registry, but also a local (ie, in-center) infection surveillance program.232-234 Increased awareness at the individual center level is key to stemming access infection and its extreme consequences, such as endocarditis and metastatic infections (eg, spinal abscesses), conditions that are disabling at best, sometimes fatal, and prohibitively costly to treat.235,236
In the effort to prevent infection, it is not only staff that must be vigilant to potential breaks in technique and the need for the appropriate use of masks. Patients also must be taught that lapses in their use of masks and poor personal hygiene are known to increase their risk for infection. Patients with type 2 diabetes are at increased risk for nasal staphylococcal carriage and catheter-related bacteremia (CRB) as a result.237,238
Maturation and Cannulation of Fistulae (CPG 3.2)
If the fistula is created with both adequate inflow artery and outflow vein, the increased flow in the vein should be immediately apparent postoperatively, evidenced by larger appearance and the presence of a continuous audible and palpable thrill along the vein, as well as actual flow measurements.126 Experienced staff should examine the fistula and the outflow vein each time the patient comes to dialysis to monitor the maturation progress. Aspects of the physical examination are summarized in Table 5. The ability of “trained, experienced dialysis nurses” to accurately predict eventual fistula maturity is excellent.72 This is even more reason to have a protocol for regular clinical examination in place in dialysis centers to teach the skills of physical examination (see CPG 4 and CPG 5) to all staff members and assess the developing fistula and not focus on the access in current use only. The optimal time to do this examination is before fluid removal because hypotension can confound the findings. Patients who are not yet on dialysis therapy should be taught how to perform self-examination and be given appropriate contact information for questions and concerns. Poor prognostic signs, such as significant decrease in the thrill, should be referred immediately back to the surgeon or the interventionalist for prompt evaluation and intervention. At a minimum, all newly created fistulae must be physically examined by using a thorough systematic approach by a knowledgeable professional 4 to 6 weeks postoperatively to ensure appropriate maturation for cannulation.239 The steps for cannulation are summarized in Table 3.
Protocol for Initial Cannulation of AVFs
If the physical assessment has shown that the fistula is adequately matured, ideally, the next step is to perform a trial cannulation. In general, the earliest that this situation occurs is when the vein diameter is greater than 0.4 cm, has a flow greater than 500 mL/min,59 and at least 1 month has elapsed since fistula creation60 (Table 3). If possible, the trial cannulation of the fistula should be done on a nondialysis day. This serves to eliminate any potential complications associated with the administration of heparin.
If a trial cannulation is not possible, it is best to perform the initial cannulation of the new access at the patient's midweek HD treatment. Performing the initial cannulation midweek helps avoid such complications as fluid overload and elevated chemistry test results associated with the weekends.
To ensure that the needle is placed properly, needle placement should be confirmed with a normal saline flush before connecting the needles to the blood pump and starting the pump. Blood return alone is not enough to show good needle placement. One option to easily check for proper needle placement is the use of “wet” needles. The needle is purged of air and the saline in the attached syringe is used to flush the needle. If an infiltration has occurred, the normal saline is less harmful to the surrounding AVF tissue. The wet needle also prevents the risk for a blood spray or spill if dry needles are used for cannulation and the caps are opened to “bleed out” the needle from the air. The opening of the needle is a risk for blood exposure to the dialysis team member, patient, and nearby patients. For these reasons, use of a wet needle is a safer technique for the AVF, patient, and dialysis team members, especially for the initial AVF cannulation. This option should be considered as part of the dialysis unit's cannulation policy and procedures. The recommended procedure is described next.
Needle selection for the initial cannulation is critical. One method used to select the appropriate needle size is a visual and tactile examination. This examination allows the cannulator to determine which needle gauge would be most appropriate, based on the size of the vessels in the fistula. Alternately, place 17 G and 16 G needles with the protective cap in place (prevents a needle stick) over the cannulation site. Compare the vein size with the needle size with and without the tourniquet applied. If the needle is larger than the vein with the tourniquet, it is too large and may infiltrate with cannulation. Use the needle size that is equal to or smaller than the vein (without the tourniquet) for the cannulation.
The smallest needle available, usually a 17 G, typically is used for initial cannulation attempts. It is important to keep in mind that blood flow delivered by a 17 G needle is limited. Prepump arterial monitoring is recommended to ensure that blood pump speed does not exceed that which the needle can provide. Prepump arterial pressure should not exceed −250 mm Hg. Based on performance of the fistula using a 17 G needle, the decision to increase the needle size for subsequent cannulation can be made.
A needle with a back eye should always be used for the arterial needle to maximize the flow from the access and reduce the need for flipping the needle.
Cannulation Tips
Infiltrations, Problems, and Tips
Fistula Hand-Arm Exercise (CPG 3.2.3)
Strengthening the forearm by using isometric exercises to increase handgrip strength (eg, squeezing a rubber ball with or without a lightly applied tourniquet) may increase blood flow, thereby enhancing vein maturation,240 and has been shown to significantly increase forearm vessel size,127,241 thereby potentially increasing flow through a fistula created using these vessels. The resulting muscle mass increase also may enhance vein prominence. Exercise also may decrease superficial fat. Correction of anemia also could increase cardiac output and decrease peripheral resistance, potentially resulting in increased flow through the fistula.
Access Flow for Dialysis in Fistulae (CPG 3.3)
After appropriate physical examination, a fistulogram is the gold standard for evaluating poor maturation of the fistula if the patient is already on dialysis therapy. Use of a non-nephrotoxic contrast material, carbon dioxide, or ultrasound should be used for patients not yet on dialysis therapy. Although a fistula can maintain patency at lower blood flows than grafts, thrombosis still occurs and, if not treated promptly, can lead to permanent loss of the access. Thrombosis rates can be reduced by prospective correction of problems.242 Delivery of dialysis is flow dependent: access flow less than 350 mL/min is likely to produce recirculation and inadequate delivery of dialysis. (See the HD Adequacy Guidelines.) Some centers have used diluted contrast (25%), and there are now published data that suggest this diluted contrast does not adversely impact residual kidney function.639 The images are of acceptable quality. The appropriate intervention for poor maturation is based on the cause of the dysfunction and may involve PTA of stenotic lesions, ligation or occlusion of vein branches (if the problem is simply > 1 major outflow vein),122,243 and/or surgical intervention, including revision of the anastomosis.75,125,126
Cannulation of AVGs (CPG 3.4)
Manufacturers' guidelines are based on the time needed for tissue-to-graft incorporation, thereby preventing the possibility of a hematoma dissecting along the perigraft space. However, most patients experience significant tissue swelling as a result of the tunneling, and palpation of the graft is difficult for the cannulator and painful for the patient.
Placement of a graft that allows for early cannulation may be advantageous in the patient who needs to begin dialysis therapy, has no other access, and does not have veins suitable for a fistula. Such an access would preclude the necessity to place a catheter while a conventional graft matures. This type of graft confers no additional benefit beyond early cannulation.114,119,128
Biografts are more likely to become aneurysmal than PTFE grafts,116 and cannulation techniques should be a hybrid of the techniques for a graft regarding depth of the access and the texture of an autogenous vein. Rotation of cannulation sites should be observed in these grafts; however, constant cannulation (buttonhole) has not been studied.244
Dialysis Catheters and Port Catheter Systems (CPG 3.5)
A dislodged (cuff exposed) or potentially infected catheter or exit site requires further assessment and possibly an intervention before being deemed safe to access for dialysis.
The Centers for Disease Control and Prevention (CDC) has no preference between transparent dressing and gauze, except in the case in which the exit site is oozing, which requires gauze.222 Standard practice is to clean the exit site and redress at each dialysis treatment (see Table 6).
Airborne contaminants from both patients and staff are prevented best by the use of surgical masks when the catheter lumens or exit site are exposed. Wearing clean gloves and avoiding touching exposed surfaces further decreases the risk for infection. Aseptic technique includes minimizing the time that the catheter lumens or exit site are exposed.222,226 Manufacturers' directions should be adhered to for the types of disinfectants recommended for safe cleaning of the skin and device. If not contraindicated, the CDC recommends use of 2% chlorhexidine,222 shown to be superior to povidone-iodine.245,246 Careful attention to hub care can decrease the CRB rate almost 4-fold to a rate approaching 1 episode/1,000 days.247
Many of the guidelines are based on good standards of clinical practice. Those relating to the use of “aseptic” technique follow the recommendations of the CDC. It is unlikely that randomized trials will ever be done in this area.
Establishing Constant-sites in Native Fistulae by Using Standard Sharp Fistula Needles
Fig 1. Starting a buttonhole. Reproduced with permission from Medisystems Inc.
*Note: It takes approximately 6-10 cannulations using a sharp needle to create a scar tissue tunnel track. Arterial and venous sites may not develop at the same rate. Once a scar tissue tunnel track is well formed, the antistick dull bevel needles should be used. If standard sharp needles are used beyond the creation of the buttonhole sites, the scar tissue tunnel can be cut. More pressure and more needle manipulation will be required to advance the antistick needle down the tunnel track. This can lead to bleeding or oozing from the needle site during use on HD. The sharp needle can also puncture the vessel at a new site or cause an infiltration. The quick transition to the antistick needle will preserve the integrity of the buttonhole site and prevent complications.
Cannulating Mature Constant Sites in Native Fistulae Using an Antistick Dull Bevel
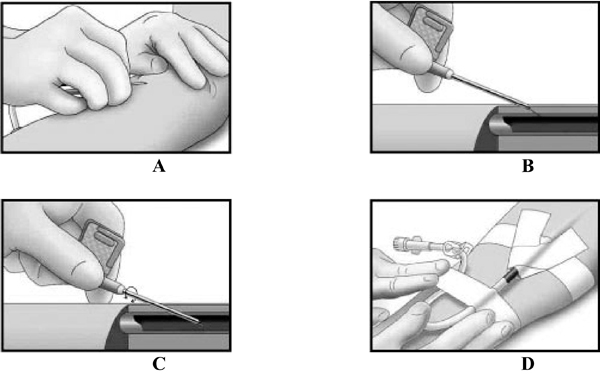
Fig 2. Cannulating a buttonhole. Reproduced with permission from Medisystems Inc.
*Note: Ensure that the same needle insertion angle and depth of penetration are used consistently for each cannulation of a constant site.