GUIDELINE 12. ASSOCIATION OF LEVEL OF GFR WITH INDICES OF FUNCTIONING AND WELL-BEING
Impairments in domains of functioning and well-being develop during the course of chronic kidney disease and are associated with adverse outcomes. Impaired functioning and well-being may be related to sociodemographic factors, conditions causing chronic kidney disease, complications of kidney disease, or possibly directly due to reduced GFR.
- Patients with GFR <60 mL/min/1.73 m2 should undergo regular assessment for impairment of functioning and well-being:
- To establish a baseline and monitor changes in functioning and well-being over time
- To assess the effect of interventions on functioning and well-being.
When there is no cure for a chronic illness, an essential healthcare goal must be to maximize quality of life. The purpose of this guideline is to identify stages and complications of kidney disease that place adult patients at greater risk for reduced quality of life. This guideline is not intended to cover all the quality of life concerns that apply to children and adolescents, nor is it intended to recommend interventions to improve quality of life in any age group. For the purpose of this guideline, concepts that embody pertinent components of quality of life will be referred to as "functioning and well-being." Recent studies show that the functioning and well-being of individuals with chronic kidney disease is related to such factors as: late referral and inadequate pre-dialysis care80; symptoms; effects of illness on physical, psychological, and social functioning; and satisfaction with health and care.452 Complications of chronic kidney disease, such as anemia, malnutrition, bone disease, neuropathy, and comorbid conditions, such as diabetes and cardiovascular disease, can negatively affect functioning and well-being. To improve functioning and well-being, patients must be referred sooner and complications and comorbid conditions must be managed appropriately.
This guideline describes the association between the level of kidney function and domains of functioning and well-being in patients with chronic kidney disease. One must analyze the full continuum of stages of chronic kidney disease to understand the risks for compromised functioning and well-being. Armed with this knowledge, clinicians can more quickly identify stages of chronic kidney disease at which deficits are likely to occur and develop strategies to treat higher risk patients and ameliorate or eliminate deficits before they become severe or irreversible.
Definitions
Health status outcomes experts recommend defining "quality of life" to include variables that health professionals can identify, quantify, and modify: (1) health status (signs and symptoms, lab values, death); (2) functional status (physical, mental, social, and role functioning), and (3) well-being (energy/fatigue, pain, health perceptions, and satisfaction).453,454 Self-report is preferable to staff report since outcomes are dependent on the lived experience and expectations of the individual patient.
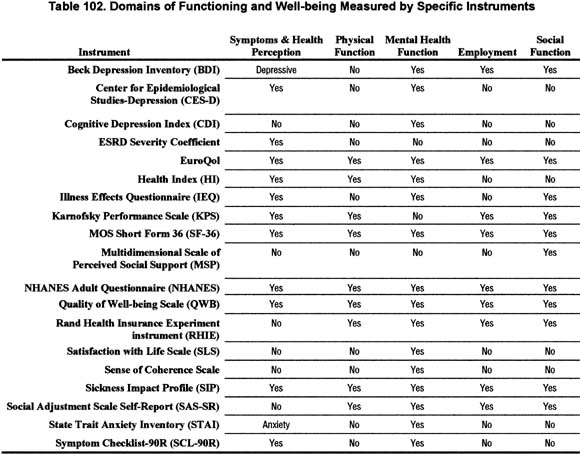
Difficulties in measuring this poorly understood concept have led researchers in the articles reviewed to study several variables using different methods and instruments (Table 102). Use of different instruments has impeded comparing findings, interpreting results, and drawing conclusions.
Strength of Evidence
Indices of functioning and well-being are impaired in chronic kidney disease (R). Dialysis patients report significantly more bodily pain, lower vitality, poorer general health, greater physical, mental, and social dysfunction, and greater limitations in their ability to work and participate in activities due to their health and emotions than the US reference norm. At least 25% are depressed.455 Dialysis patients' exercise capacity is significantly worse than that of healthy controls.456 Kidney failure negatively affects sense of control and health outlook in those on dialysis.457 About 39% of those who worked full or part-time 6 months before dialysis do not continue working when they start dialysis.4 Elderly people on dialysis engage in few previously enjoyed activities outside their homes and many leave home only for dialysis because of weakness.458
Impairment in indices of functioning and well-being are associated with worse outcomes in chronic kidney disease (R). Impaired functioning and well-being in dialysis patients is linked to increased risk of death and hospitalization while improvement in scores has been associated with better outcomes. Patients with SF-36 Physical Component Summary (PCS) scores <34.6 had a 2.03 relative risk of dying and a 1.67 relative risk of being hospitalized. Each 5-point improvement in PCS scores was associated with 10% longer survival and 6% fewer hospital days. On the SF-36, a Mental Health scale score ![]() 52 and a Mental Component Summary (MCS) score
52 and a Mental Component Summary (MCS) score ![]() 42 indicate depression. Each 5-point improvement in the MCS score is associated with 2% fewer hospital days.455
42 indicate depression. Each 5-point improvement in the MCS score is associated with 2% fewer hospital days.455
Impairment in functioning and well-being are associated with sociodemographic characteristics (R). Low income and low education were associated with greater impairments in functioning and well-being in patients with chronic kidney disease.459
Impairment in functioning and well-being may be due to conditions that cause chronic kidney disease (such as diabetes or hypertension) or complications of decreased GFR (such as anemia, malnutrition, bone disease, or neuropathy) (R). Hypertension, diabetes with angina, prior cardiac infarction,460 osteoporosis, bone fractures,461 and malnutrition462 have been shown to impair functioning and well-being in those with no known kidney disease. Among veterans with diabetes, neuropathy and kidney disease have been associated with the greatest decrease in functioning and well-being.463
Anemia has been linked to poor functioning and well-being in patients with severely decreased GFR and dialysis patients, and improving anemia with erythropoietin has been linked to improvement in functioning and well-being.284,464-468
Indices of functioning and well-being are related to the level of GFR; below a GFR of approximately 60 mL/min/1.73 m2, there is a higher prevalence of impairments in indices of functioning and well-being (S, C). Data from cross-sectional studies and baseline data from longitudinal studies were reviewed to assess the relationship between level of kidney function and level of functioning and well-being. Populations studied include those with decreased kidney function, including those with functioning transplants, and dialysis patients when compared with healthy subjects or kidney transplant recipients. While much of the data on functioning and well-being related to outcomes have been obtained in dialysis patients, there is convincing evidence that abnormalities in functioning and well-being begin earlier in chronic kidney disease and may well be related to declining GFR.
Symptoms (Table 103 and Fig 44).
Figure 44 |
|
Kidney function (GFR) and odds of having symptoms affecting quality of life and well-being in the MDRD Study, controlled for age, gender, race, kidney diagnosis, education, income, and smoking status. Reprinted with permission.469 |
|
Reduced kidney function is associated with increasing symptoms such as tiring easily, weakness, low energy, cramps, bruising, bad tasting mouth, hiccoughs, and poor odor perception. This is true in patients with native kidney disease and those with kidney transplants. Diabetic dialysis and transplant patients are more likely to report poor health than dialysis or transplant patients who do not have diabetes.
Physical Functioning (Table 104 and Figs 45 and 46).
Figure 45 |
|
Adjusted prevalence of physical inability to walk by GFR category (NHANES III). Predicted prevalence of physical inability to walk one-quarter mile among adult participants age 20 years and older in NHANES III, 1988 to 1994. Values are adjusted to age 60 years using a polynomial regression. 95% confidence intervals are shown at selected levels of estimated GFR. |
|
Figure 46 |
|
Adjusted prevalence of physical inability to lift by GFR category (NHANES III). Predicted prevalence of physical inability to lift 10 pounds among adult participants age 20 years and older in NHANES III, 1988 to 1994. Values are adjusted to age 60 years using a polynomial regression. 95% confidence intervals are shown at selected levels of estimated GFR. |
|
Decreased GFR in NHANES III subjects is associated with impaired walking and lifting ability. In transplant recipients, reduced kidney function is also associated with poorer physical function scores. In one study of patients with decreased GFR, impairment in physical function was not significantly related to the level of kidney function, but physical impairment was 8 times worse than in the general population. Dialysis patients report greater physical dysfunction than transplant recipients and diabetic dialysis and transplant patients are more likely to report physical dysfunction than those patients who do not have diabetes.
Depression (Table 105).
Reduced kidney function is associated with poorer psychosocial functioning, higher anxiety, higher distress, decreased sense of well-being, higher depression, and negative health perception. Depressed patients are more likely to report poor life satisfaction, irrespective of kidney function. Dialysis patients report significantly lower "happiness with personal life" and lower psychosocial functioning than transplant recipients. In elderly Mexican Americans, kidney disease has been found to be predictive of depressive symptoms.
Employment and Usual Activities (Table 106).
Reduced kidney function is associated with lower employment. In those with chronic kidney disease and GFR <50, the presence of physical dysfunction is significantly related to unemployment, but the association to kidney function is not significant since physical dysfunction is not uniformly present. Full-time employment is higher for those with decreased GFR (mean serum creatinine 5.4 mg/dL, 69%) compared with those with kidney failure (mean serum creatinine 13.7 mg/dL, 12%). More dialysis patients report their health limits work and other activities than those with functioning transplants. Dialysis and transplant patients with diabetes are more likely to report difficulty working than dialysis and transplant patients without diabetes.
Social Functioning (Table 107).
Reduced kidney function is associated with reduced social activity, social functioning, and social interaction. Dialysis patients report fewer neighborhood acquaintances, social contacts, and worse social well-being than healthy individuals while transplant recipients report higher social function and social interaction than those on dialysis. Diabetics on dialysis or with transplants are more likely to report problems with social interaction than nondiabetic patients. Level of perceived social support in chronic kidney disease is not associated with the level of kidney function.
Most study samples were not randomly selected. Medication usage was not reported even if medications (eg, anti-depressants) could affect outcomes. Seven of 12 studies did not provide full information on patient demographics. Three studies reported differences between groups of very unequal sizes and one reported percentages but did not report whether observed differences were statistically significant.
Historically, there has been no "gold standard" definition for quality of life or functioning and well-being. Researchers have studied multiple variables using standardized and non-standardized instruments. Thus, results are not comparable to one another.`479 With lack of instrument comparability, findings appear to be conflicting. Many studies have examined the relationships between functioning and well-being and treatment modalities after the onset of kidney failure. Few studies of persons with decreased GFR have examined the relationship between level of GFR and functioning and well-being. Three of the studies of individuals with decreased GFR had such severely restrictive inclusion criteria for level of kidney function that functioning and well-being deficits were already present. Of the 12 studies reported, 3 reported no measure of kidney function and 2 reported only serum creatinine, a less reliable measure of kidney function than GFR or creatinine clearance. Most of the studies reported only mean values for kidney function. Only the MDRD Study and NHANES III examined functioning and well-being at a wide range of levels of kidney function. Precise statements about how early deficits in domains of functioning and well-being occur as kidney function deteriorates require this essential data. Finally, since anemia has been shown to limit functioning and well-being, inadequate anemia management in studies conducted prior to the widespread use of erythropoietin could have affected outcomes. Therefore, recent functioning and well-being outcomes may not be comparable to outcomes reported in studies prior to 1989 even if the same instruments were used.
The conferees at the Institute of Medicine (IOM) Workshop "Assessing Health and Quality of Life Outcomes in Dialysis" recommended that ESRD providers:
Data reported in the reviewed studies suggest that decreased kidney function affects patients' functioning and well-being through several dimensions. Deficits in functioning are reported by patients even at early stages of chronic kidney disease, and persist even after transplantation. The implications of these findings are:
These recommendations are based on the opinions expressed by the authors of most of the studies reviewed for this guideline, as well as those of recognized experts in functioning and health status outcomes measurement who attended the IOM Workshop.
Researchers may use any of a wide array of instruments to measure functioning and well-being throughout the course of chronic kidney disease. However, clinicians want to know what instrument to use, when to use it, and who should administer, score, and analyze the data. In general, it is practical for clinicians to use only a few instruments and to gain experience with them. Based on the literature reviewed for this guideline, it appears that any clinician treating patients with decreased GFR can administer the Dartmouth COOP Charts, DUKE Health Profiles, Kidney Disease Quality of Life, or SF-36 that have been used with dialysis and transplant patients (Table 108).
In the clinical setting ease of use is essential. These surveys are recommended because each has an instructional manual and patients can complete them independently or with limited assistance. To assess specific limitations in functioning and well-being, clinicians can supplement these general instruments with more specific instruments including performance-based tests of physical functioning.
Research in dialysis patients has shown that functioning and well-being pre-treatment may predict post-treatment outcomes. Therefore, large-scale longitudinal studies are needed to evaluate the relationship between GFR and all domains of functional status and well-being throughout the course of progression of kidney disease. More research should be undertaken using the recommended standardized instruments and their outcomes compared. Whenever specific medications could affect outcomes, usage should be assessed. Because conditions such as anemia, bone disease, cardiovascular, disease, and diabetes can affect functioning and well-being, researchers need to study whether appropriate management of these conditions improves functioning and well-being. Finally, researchers need to examine the effectiveness of rehabilitation interventions in earlier stages of chronic kidney disease. Doing so could provide further scientific evidence for the relationship of kidney function and treatment on patients' risk of dysfunction, hospitalization, and death and increase understanding of what interventions improve functioning and well-being and reduce the burden of chronic kidney disease on the patient, his or her family, and society.