CLINICAL PRACTICE guidelines (CPGs) are “systematically developed statements based on current professional knowledge to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances.” As such, guidelines define best clinical practices based on available evidence. Their translation into clinical practice for use in specific clinical circumstances is what makes guidelines relevant.
Passive dissemination of guidelines has proven to be of limited clinical utility. Nonadherence to best clinical practices, as articulated in CPGs, has been routinely observed. The translation of CPGs into clinical practice requires the development of a multi-component long-term implementation plan. A central component of such a plan is the linkage of selected guidelines to continuous quality improvement (CQI) programs to improve outcomes within a given local health care delivery system.
CQI efforts require measurement tools, both to quantify the current process of care and to monitor the success of changing practice patterns on clinical outcomes. Clinical performance measures (CPMs) are such tools. The rationale for CPMs, the essential steps in their development, and the attributes of well-designed CPMs have been described.653,654
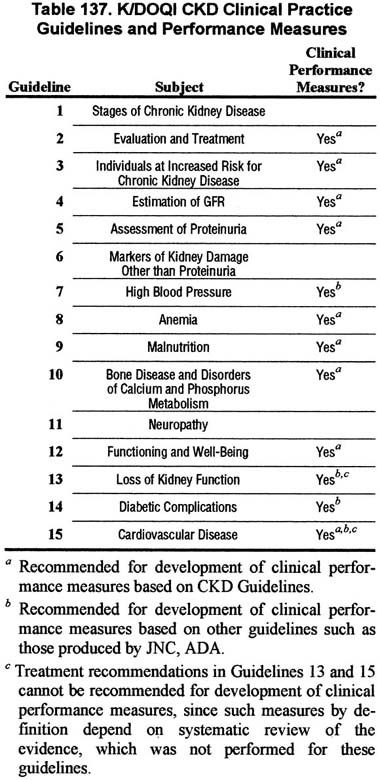
The first step in the development of CPMs is the prioritization of CPGs, in collaboration with the Work Group that developed the guidelines. Following are guideline statements recommended by the CKD Work Group for potential use in CQI and CPM and examples of CPM that could be developed from them (Table 137).
A special subcommittee of the Advisory Board, chaired by Alan S. Kliger, MD, is assessing feasibility and exploring opportunities for developing these recommendations for future use as CPMs.
Guideline 2
Preparation for kidney replacement therapy (dialysis and transplantation), as well as vascular access care, should be initiated when the estimated GFR declines to <30 mL/min/1.73 m2.
Guideline 3
Individuals at increased risk for chronic kidney disease should be tested at the time of a health evaluations to determine if they have chronic kidney disease. These include individuals with:
Measurements should include:
Guideline 4
Estimated GFR should be the parameter used to evaluate the level of kidney function.
Guideline 5
The ratio of protein or albumin to creatinine in spot urine samples should be monitored in all patients with chronic kidney disease.
Guideline 7
Blood pressure should be monitored in all patients with chronic kidney disease.
High blood pressure should be evaluated and treated according to established guidelines, such as JNC-VI and ADA.
Guidelines 8-12
Patients with GFR <60 mL/min/1.73 m2 should be evaluated and treated for complications of decreased GFR. This includes measurement of:
Guideline 13
Estimated GFR should be monitored yearly in patients with chronic kidney disease, and more frequently in patients with:
Guideline 14
Individuals with diabetic kidney disease are at higher risk of diabetic complications, including retinopathy, cardiovascular disease, and neuropathy.
They should be evaluated and managed according to established guidelines.
Guideline 15
Individuals with chronic kidney disease are at increased risk of cardiovascular disease.
They should be considered in the “highest risk group” for evaluation and management according to established guidelines.