The assessment and treatment of both risk factors and end organs are essential in the management of cardiovascular diseases. The first section will deal with the end organs and will focus on cardiac, cerebrovascular and peripheral vascular diseases. Cardiac diseases have justifiably received the most attention because they are by far the most common cause of cardiovascular deaths in dialysis patients. Cerebrovascular diseases and peripheral vascular diseases, however, also lead to substantial morbidity and mortality and have often been overlooked by practitioners and clinical researchers.
The workgroup has faced dilemma in the scope and depth of the coverage of end organ diseases. There has been only one small randomized trial that demonstrated beneficial effects of specific cardioprotective drugs (namely, carvedilol) published in dialysis patients. Therefore, most guidelines described in this section are referred from published guidelines in the general population. Nonetheless, there are unusual features in the dialysis patients that the practitioners need to be aware of. For example, the pathophysiology and rate of progression of cardiac valvular calcification appear to be different from those in the general population. Surveillance and treatment strategies should take these caveats into consideration. On the other hand, the implant of tissue valves is proscribed in the existing ACC/AHA guidelines. More recent and stronger evidence, however, suggest that tissue valves are associated with equivalent outcomes in dialysis patients. These similarities, not only differences, between dialysis patients and the general population also need to be emphasized.
The section on end organ diseases is written for not only the nephrologists, but also the general practitioners, cardiologists, vascular surgeons and other practitioners.
Guideline 10: Peripheral Vascular Disease
Both diabetic and nondiabetic dialysis patients are at risk for peripheral vascular disease (PVD),144,145 with approximately 15% of incident patients having a clinical diagnosis of PVD.
10.1 Diagnosis of PVD:
10.1a At the time of dialysis initiation, all patients should be evaluated for the presence of PVD. (C)
10.1b Evaluation should include physical examination including assessment of arterial pulse and skin integrity. (C)
10.1c Further specialized studies, such as duplex studies or invasive testing, should be undertaken if abnormalities are detected upon physical examination and interventions are considered. (C)
10.2 Approach to therapy of PVD: (C)
10.2a Patients with PVD should be treated in the same manner as the general population in regard to smoking cessation, lipid-lowering therapy, glycemic control, blood pressure control, and the use of ACE inhibitors and antiplatelet agents. In addition, supervised exercise regimens and medications to increase vasodilation should be considered in patients with claudication and without critical leg ischemia. Established national guidelines, similar to those for stroke, are not available for PVD in the general population.
Screening for PVD (Weak)
Ankle brachial index (ABI) (ankle systolic blood pressure divided by brachial systolic blood pressure) is a simple method of screening for PVD. However, ABI might be falsely elevated in dialysis patients because of vascular calcification.146 Toe brachial index (TBI) is not affected by vascular calcification.146 Even though ABI and TBI are simple, inexpensive, noninvasive methods, further studies are warranted to determine whether screening for asymptomatic PVD with these tests improve limb survival.
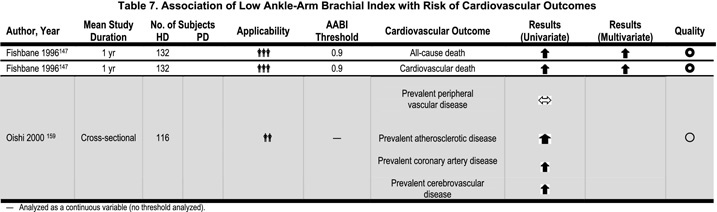
Checking arterial pulses and assessing skin integrity should be part of a physical examination, particularly in diabetic dialysis patients. As PVD is a strong predictor of cardiovascular mortality in the general and dialysis population,147,148 early diagnosis of PVD and aggressive medical therapy (smoking cessation, lipid-lowering therapy, glycemic control, blood pressure control, and the use of ACE inhibitors and antiplatelet agents) might improve cardiovascular survival in dialysis patients (Table 7).
Therapy of PVD (Weak)
There are no randomized, controlled trials for PVD in dialysis patients that establish the efficacy of any pharmacological agents or other interventions. In the absence of evidence to the contrary, it might be reasonable to extend the therapy of PVD in the general population to the dialysis population. The therapy of PVD depends upon the presence of claudication and critical leg ischemia in the general population.149
When compared to the general population, outcomes after revascularization for PVD in dialysis patients are inferior.150,151 The problems with revascularization in PVD in dialysis patients include: high perioperative and 1-year mortality; decreased wound healing; loss of limb despite patent graft; and prolonged hospital stay and poor rehabilitation.152–156 Therefore, some authors have argued for the liberal use of primary amputation in dialysis patients.157
However, careful patient selection for revascularization in dialysis patients might result in acceptable outcomes. A study of 44 HD patients who underwent revascularization reported a 2-year survival rate of 48%, perioperative mortality of 9%, primary graft patency at 1 year and 2 years of 71% and 63%, respectively and limb salvage at 1 year and 2 years of 70% and 52%, respectively.158 In this study, an aggressive approach to limb salvage was favored when patients were found to be ambulatory or able to use the affected extremity for purposes of weight bearing or transfer. Attempted limb salvage was not advocated for patients who were chronically bedridden, or those with uncontrolled infection or tissue necrosis precluding a reasonable expectation of limb salvage.
Therefore, symptomatic PVD in dialysis patients should not automatically result in amputation in all patients. Revascularization (surgical or angioplasty with stent) might be the preferred method of treatment of symptomatic PVD in selected dialysis patients. Extensive tissue necrosis in nonweight-bearing limbs and preoperative infection might be indications for primary amputation.