Traditional risk factors—such as diabetes, hypertension, dyslipidemia—and those specific to dialysis patients (anemia and mineral metabolism abnormalities) require regular assessment and treatment as per current recommendations. The relative importance and weight of each of these risk factors in the dialysis population is not known and, in the absence of controlled trials in this population, current recommendations from existing organizations should be followed, with special consideration given to potential risks.
Furthermore, lifestyle issues such as smoking, physical activity, depression, and anxiety are the cornerstones of therapy as in the general population. The treatment options are often similar, but the impact of these factors is potentially more profound in dialysis patients. These factors are all discussed in this section. Special attention will be paid to the difference between the usual recommendations and those for dialysis patients.
Guideline 14: Smoking, Physical Activity, and Psychological Factors
While there are few data specific to CVD in dialysis patients regarding smoking, physical activity, and psychological factors (depression, anxiety, and hostility), the evidence in the general population is clearly in favor of addressing each of these issues. In order to ensure that clinicians caring for dialysis patients do not overlook the importance of each of these factors, we have dedicated an entire guideline to them.
14.1 All dialysis patients should be counseled and regularly encouraged to stop smoking. (A) Referral to smoking cessation specialists is recommended. (C)
14.1a Special consideration should be given to cessation of smoking in depressed individuals with little ability to engage in physical activity. (C)
14.2 All dialysis patients should be counseled and regularly encouraged by nephrology and dialysis staff to increase their level of physical activity. (B)
14.2a Unique challenges to exercise in dialysis patients need to be identified in order to refer patients appropriately (e.g., to physical therapy or cardiac rehabilitation) and to enable the patients to follow regimens successfully. Such challenges include orthopedic/musculoskeletal limitations, cardiovascular concerns, and motivational issues. (C)
14.3 Measurement of physical functioning:
14.3a Evaluation of physical functioning and re-evaluation of the physical activity program should be done at least every 6 months. (C)
14.3b Physical functioning can be measured using physical performance testing or questionnaires (e.g., SF-36). (C)
14.3c Potential barriers to participation in physical activity should be assessed in every patient. (C)
14.4 Physical activity recommendations:
14.4a Many dialysis patients are severely deconditioned and therefore may need a referral for physical therapy to increase strength and endurance to the point where they are able to adopt the recommended levels of physical activity.
14.4ai Patients who qualify for cardiac rehabilitation should be referred to a specialist. (C)
14.4aii The goal for activity should be for cardiovascular exercise at a moderate intensity for 30 minutes most, if not all, days per week. Patients who are not currently physically active should start at very low levels and durations, and gradually progress to this recommended level. (C)
14.4b Follow-up:
14.4bi Physical functioning assessment and encouragement for participation in physical activity should be part of the routine patient care plan. Regular review should include assessment of changes in activity and physical functioning. (C)
14.5 Depression, anxiety, and hostility should be identified and treated in dialysis patients. (B)
14.5a Every dialysis patient should be seen by the dialysis social worker at initiation of dialysis, and at least biannually thereafter, to assess the patient’s psychological state, with specific focus on the presence of depression, anxiety, and hostility. (C)
14.5b Dialysis patients should be treated for depression, anxiety, and hostility if they are experiencing these psychological states. (C)
Definitions
Physical activity
Bodily movement that is produced by the contraction of skeletal muscle and that substantially increases energy expenditure.
Regular physical activity
Accumulation of at least 30 minutes of moderate-intensity physical activity on most—and preferably all—days of the week. Moderate intensity is at levels appropriate to the capacity, needs, and interest of the individual.
Physical functioning
Ability of the individual to participate in required activities of living.
Physical capacity
Measured ability to perform specific tasks, such as performance testing and exercise testing.
Major Depression is typically characterized by having a depressed mood and a significant loss of interest in all activities that persists for a minimum of 2 weeks and is accompanied by a minimum of four of the following symptoms: appetite or sleep disturbances; psychomotor retardation or agitation; fatigue; feeling guilty or worthless; problems with concentration; or suicidal ideation.270 Because many of the somatic symptoms associated with depression are also symptoms of uremia, the cognitive symptoms may be better used when assessing depression in dialysis patients.
Anxiety has both physiological and psychological symptoms. The psychological aspects, which may be more relevant when assessing those with pre-existing medical problems, include: feelings of powerlessness; a sense of impending danger; exhaustive alertness; self-absorption that interferes with ability to effectively problem-solve; and extreme doubts about a threatening occurrence and one’s ability to deal with it; and worries that are difficult to control and may interfere with functioning. The concerns may be with or without cause, are pervasive, and last longer than would be expected.271
Hostility involves negative behavior and feelings, often directed at interpersonal relationships. It includes such characteristics as anger, cynicism, and lack of trust.270
Smoking (Moderately Strong)
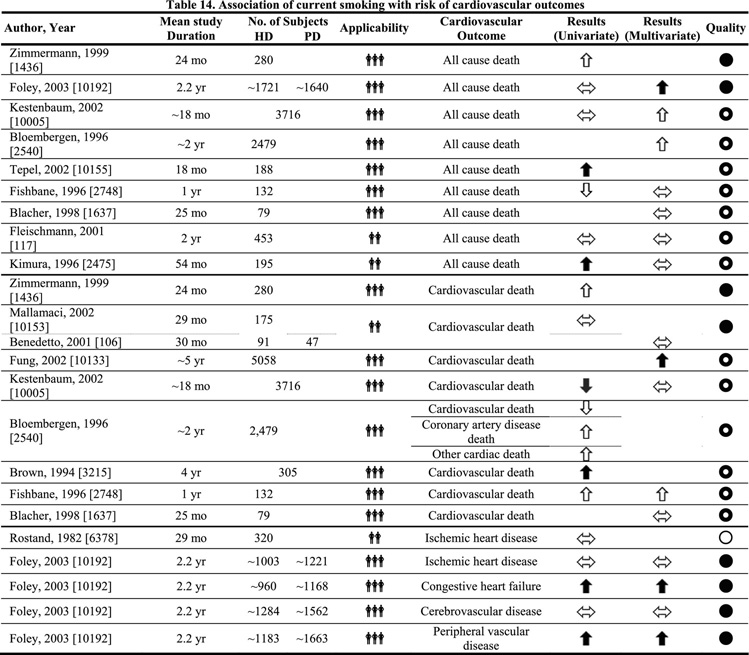
Cigarette smoking is universally recognized as an independent risk factor for CVD. Smoking, therefore, should also be discouraged in patients with CKD. However, this recommendation is even more compelling, considering the relationship between smoking and poor outcomes in dialysis and transplant patients (Table 14). The frequency and duration of contact with dialysis health-care providers should facilitate concerted and serious efforts directed towards assisting patients to discontinue smoking.
Physical activity (Weak)
Dialysis patients have extremely low levels of physical functioning and exercise capacity, and are often physically inactive. Physical inactivity is known to be a risk factor for CVD and overall mortality272 as well as increasing risk for developing several chronic conditions, including diabetes273,274 and hypertension.275 In the general population, regular physical activity: reduces high blood pressure in persons with hypertension; reduces depression and anxiety; helps to control weight; helps to maintain healthy bones, muscles, and joints; helps older adults become stronger and better able to move about without falling; and promotes psychological well-being. This evidence is clearly documented in the U.S. Surgeon General’s Report on Physical Activity and Health.276 Several other national guidelines recommend regular physical activity as part of treatment for cardiovascular-related risk factors, specifically, the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure277 and the National Cholesterol Education Project Adult Treatment Guidelines III.278 In fact, in both of these documents, lifestyle change (which includes regular physical activity) is the first recommendation.
Data in dialysis patients indicate that self-reported physical functioning is highly predictive of outcomes such as hospitalizations and death, even when corrected for case mix and comorbidity.279 Likewise, a recent study has shown that objective laboratory measures of physical fitness are independently predictive of mortality, with patients with low maximal oxygen uptake (<17 mL/kg/min) showing significantly higher mortality.280 It is not known whether improving exercise capacity and/or increasing physical activity will result in reduction in hospitalizations or death in dialysis patients.
Although no randomized clinical trials have been performed to assess the effects of physical activity on cardiovascular risk in patients with renal failure, the preponderance of evidence and existing guidelines for physical activity for other populations at high risk for CVD suggest similar implementation of physical activity for patients with renal failure. The well-documented literature on low levels of physical functioning in this population, and evidence that it can be improved with exercise training, warrants attention to this lifestyle issue.281–297
Psychological factors (Moderately Strong)
The purpose of this guideline is to identify those individuals at increased risk for developing or worsening CVD due to their psychological state. There is a strong association between depression, anxiety, and hostility, and CVD in the general population. No research was identified that addressed the association of psychological state per se with CVD in dialysis patients. However, since there is a high prevalence of depression and anxiety, as well as documented hostility, in this population, it is reasonable to recommend assessment and treatment of these conditions that are known elsewhere to be highly associated with CVD.
Depression
In the 1980s, two meta-analyses of the research literature evaluating psychological functioning and CVD found conflicting results. One strongly suggested that depression relates to CAD, including its development, while the other found that depression did not predict the occurrence of CAD.298,299 Another study of 498 men found that depression was only slightly associated with incidence of CHD.300 However, recent evidence from 13 rigorously designed research studies linking patients exhibiting depressive symptoms or experiencing major depression with higher cardiovascular morbidity and mortality suggests depression may be an independent risk factor in CVD progression.270,301 A meta-analysis of 11 epidemiological studies found that the relative risk for developing CHD was 1.64 in depressed individuals.300 Multiple studies that followed patients with coronary heart disease for up to 2 years found that depression predicted the occurrence of angina pectoris, MI, and angioplasty and/or coronary artery bypass surgery.302 Depression also resulted in more than a fourfold increased independent risk of mortality, giving it the same prognostic value as a prior history of MI.302
Rates of depression of 30%–50% have been reported in dialysis patients who use self-reported measures of depressive symptoms, although lower rates have been reported when DSM III-R criteria are used to assess for major depression.303 HD patients’ mean depression score has been documented to be significantly higher than that of normal subjects.304 In one study of 128 dialysis patients, 25.7% exhibited symptoms of depression and 26.6% scored within the range of clinical depression. Approximately 50% of participants scored within the range that indicated a potentially clinically significant depression.305 A more recent study found that approximately 25% of the 1,000 HD patients studied were depressed.279 Forty-three percent of 9,382 hemodialysis patients scored within the depressed range of the Center for Epidemiological Studies Depression Screening Index.306 Multiple studies have demonstrated that depression is associated with decreased overall survival in dialysis patients. It has not been established whether depression is an independent risk factor or if depression affects other variables, such as adherence, that may impact survival.303
Anxiety
Most early studies suggested that anxiety was, at the most, only slightly related to CVD.298,299 An exception was a 5-year prospective study of 10,000 adult men which found that not only was anxiety an independent contributor to the development of angina pectoris, but the likelihood of developing angina increased as the level of anxiety rose.307 Later evidence from three research studies, one involving 34,000 healthy subjects, further documented a significant association between anxiety and the development of cardiac events and SCDs.270 Others have shown that social anxiety both significantly predicts CHD development as well as increases its incidence.300 Multiple studies have established that those who experienced both depression and anxiety had a compounded cardiac risk.270 Other research has documented the relationship between anxiety and cardiac events, including MI302,308,309 and SCD.310Approximately 45% of 128 dialysis patients in one study exhibited clinical anxiety.305 As with depression, the mean anxiety score of HD patients has been found to be significantly higher than that of normal subjects.304
Hostility
Research evaluating the relationship of hostility with CVD has shown mixed results in the general population. Three prospective, controlled studies representing 1,250 subjects in the general population, which used the Cook-Medley Hostility Inventory as a measure of hostility, demonstrated that the presence of hostility predicted CAD events and overall mortality.298 Further support for hostility being an independent risk factor for CAD comes from a meta-analysis of 45 research studies.311 Data from the Western Collaborative Group Study showed that potential for hostility was a significant predictor for developing CHD.299 Additional studies revealed that hostility was independently related to coronary atherosclerosis and significantly predicted the development of CHD.299 It was found that patients with documented hostility had a 1.9 risk ratio for experiencing MI, angina, and cardiac death after controlling for other traditional risk factors.302
The intensity of anger, which is a component of hostility, has also been associated with CVD. In a prospective study of 1,305 individuals, those who experienced a higher level of anger were found to have a 3.2 times higher risk of having a fatal or nonfatal coronary event compared to those who reported the lowest level of anger.310 Another study documented that the relative risk of experiencing another MI was 2.3 within 2 hours of an anger episode in 1,623 post-MI patients.302
The Kellner Symptom Questionnaire, which was administered to female subjects, showed that not only were dialysis patients more depressed, they were also more hostile than the healthy control group.312 A study of dialysis patients and their partners documented that those on dialysis experienced a variety of psychological reactions, including anger.313
Physiological factors associated with depression, anxiety, and hostility. (Weak)
Depression, anxiety, and hostility may be associated with CVD through several mechanisms. For example, these factors may lead to nonadherence with the dialysis or diet regimen, which may impair cardiovascular functioning. In addition, a patient who is experiencing any of these psychological states may be more prone to engage in high-risk behaviors, such as smoking, that could have a negative impact on cardiovascular health.
Additionally, there are pathophysiological effects when a person experiences depression, anxiety, or hostility. Depression has been associated with impaired platelet functioning, hypercortisolemia, heightened plasma and urinary catecholamines, increased heart rate, altered vagal control, and a reduction in the variability of the heart rate. Each of these may have a negative impact on the prognosis of CHD.301 Patients experiencing depression have exhibited sympathoadrenal hyperactivity, and it has been suggested that this may contribute to the development of CVD due to the cathecholamines’ effects on cardiac functioning and platelets.301 Depression has also been associated with the inflammatory response, and consequent CAD progression.302 Other physiological changes associated with depression that negatively impact cardiovascular function are hypercoagulability, systemic and localized inflammation, and cardiac rhythm alterations.314
Some patients with anxiety have exhibited decreased heart rate variability, which may result in pathological alterations in cardiac autonomous tone. This could involve either increased sympathetic stimulation or impaired vagal control, both of which have been linked to mortality.270 Sympathetic-adrenal medullary and adrenal cortical activity are higher when anxiety is present, and this may also be a contributor to CVD.307 Anxiety may also result in coronary vasospasm that can cause atherosclerotic plaques to rupture.302
People who exhibit hostility and are exposed to certain stimuli, such as mental tasks, have been shown to have higher blood pressure and heart rates than those who are not hostile,270,298 as well as other physiological changes that are linked to CVD.270,302
Assessment and suggested treatment of depression, anxiety, and hostility. (Weak)
Although there are no studies specifically addressing the relationship between psychological factors and CVD in dialysis patients, the prevalence of these factors, as discussed earlier, makes treatment an important issue. There is documented evidence that psychological and social interventions, in addition to standard cardiac rehabilitation, can significantly reduce mortality and morbidity and have positive influences on cholesterol, blood pressure, and heart rate.302
Adequate dialysis and anemia control are important contributors to overall well-being and quality of life for dialysis patients. These factors, combined with an assessment of the patient’s physical health and potential side effects of medication, should first be evaluated as possible contributors to depression and anxiety.
Typically, referral to a psychologist may be necessary for psychometric testing, although quality-of-life assessments, which include depression, have become routine in many dialysis facilities. Several instruments measure levels of depression, anxiety, and hostility (Table 15). The Beck Depression Inventory (BDI), which is used frequently, is a well-validated instrument.303 The BDI Fast Screen is a self-report instrument that was developed specifically to measure depression in patients who have medical illness.315 The Cognitive Depression Index, a subset of the BDI, controls for the possible impact of somatic symptoms, which may artificially inflate depression rates when assessing the dialysis population.303 The SF-36 has also been established as a good screening tool for depression with center HD patients.279 The World Health Organization Quality of Life-100 (WHOQOL-100) and its abbreviated version, WHOQOL-BREF, were developed for use throughout the world in a variety of cultures. These instruments contain a psychological domain that assesses depression and anxiety.316 The State-Trait Anxiety Inventory (STAI) has been commonly used and is considered to be one of the best standardized tests to measure anxiety.317 Similarly, the State-Trait Anger Expression Scale (STAXI) has also been used extensively. It has predictive validity and vast normative data, and distinguishes between the suppression and the expression of anger.318 Another measure of hostility is the Cook-Medley Hostility Inventory, which is taken from the Minnesota Multiphasic Personality Inventory (MMPI). This instrument has been found to predict CAD events, CHD mortality and overall mortality.298,319
Social support has been shown to lower depression in the general population.303 Poor social support has also been associated with an increased incidence of CAD.270 Group counseling that focused specifically on modifying Type A personality traits, such as hostility, was found not only to reduce Type A characteristics, but also to significantly reduce cardiac deaths in a controlled study of over 800 post-MI participants. Group instruction that included stress reduction techniques was also found to lower hostility, as well as cardiac deaths.270
The use of cognitive-behavioral therapy was found to lower anxiety and reduce depression in the general population,311 and has also effectively reduced hypertension and the morbidity and mortality from CVD that is associated with hypertension.318 Relaxation techniques were also equal to or more effective than other psychological interventions in lowering physiological arousal in persons with CVD. Biofeedback, one form of relaxation, lowered hypertension in 60% of study participants with CVD.318 Other techniques, such as controlled breathing, have been found to be significantly associated with reduction in MIs, as well as all-cause mortality.270 Chronic HD patients who were taught simple progressive relaxation exercises had significantly lowered anxiety levels, while a control group remained unchanged.317 Multiple studies with the general population have documented that anger is also treatable using a variety of different interventions.311,318
Patient education has been documented to impact psychological state. Patients who participated in an educational program about CKD (which included information on its treatments and potential impact on quality of life) prior to beginning dialysis were found to have significantly lower levels of anxiety and improved moods compared to a control group. This difference remained for the first six months after initiating dialysis.320 As discussed earlier in this guideline, physical activity can also significantly impact the dialysis patient’s well-being.
If patients exhibit depressive or anxiety symptoms that do not respond to other treatments, psychotropic medication should be considered. Selective serotonin reuptake inhibitors or atypical antidepressants, such as nefazodone or buproprion, may be considered for use in CVD patients who are depressed. These antidepressant medications may have fewer potential negative cardiovascular effects than many other antidepressants.301 Studies have documented that pharmacological intervention has had positive effects on the psychological functioning of patients with CKD.321
Smoking
Physical activity
Psychological factors
Psychological factors
Smoking
Physical activity
Psychological factors