The assessment and treatment of both risk factors and end organs are essential in the management of cardiovascular diseases. The first section will deal with the end organs and will focus on cardiac, cerebrovascular and peripheral vascular diseases. Cardiac diseases have justifiably received the most attention because they are by far the most common cause of cardiovascular deaths in dialysis patients. Cerebrovascular diseases and peripheral vascular diseases, however, also lead to substantial morbidity and mortality and have often been overlooked by practitioners and clinical researchers.
The workgroup has faced dilemma in the scope and depth of the coverage of end organ diseases. There has been only one small randomized trial that demonstrated beneficial effects of specific cardioprotective drugs (namely, carvedilol) published in dialysis patients. Therefore, most guidelines described in this section are referred from published guidelines in the general population. Nonetheless, there are unusual features in the dialysis patients that the practitioners need to be aware of. For example, the pathophysiology and rate of progression of cardiac valvular calcification appear to be different from those in the general population. Surveillance and treatment strategies should take these caveats into consideration. On the other hand, the implant of tissue valves is proscribed in the existing ACC/AHA guidelines. More recent and stronger evidence, however, suggest that tissue valves are associated with equivalent outcomes in dialysis patients. These similarities, not only differences, between dialysis patients and the general population also need to be emphasized.
The section on end organ diseases is written for not only the nephrologists, but also the general practitioners, cardiologists, vascular surgeons and other practitioners.
Guideline 3: Acute Coronary Syndromes
The diagnosis of acute coronary syndromes (ACS) in dialysis patients and in the general population is usually based on the triad of symptoms, ECG findings, and cardiac biomarkers. The outcomes of patients on dialysis with ACS are often poor, which may be related to the lack of a consistent and standard approach to the treatment of ACS.
3.1 All dialysis patients presenting with ACS should be treated as in the nondialysis population, with the exception of specific attention to drugs that have altered clearances in kidney failure (e.g., low molecular weight heparin). These therapies include percutaneous coronary intervention (PCI), CABG, antiplatelet agents, beta-blockers, thrombolytic therapy, and lipid-lowering agents. (C)
3.1a Dialysis patients with ST-segment elevation MI should receive acute reperfusion therapy (as do patients in the nondialysis population). With the potential for increased hemorrhagic risk associated with thrombolytic therapy, emergent PCI is the preferred treatment if it is available. (C)
3.2 The timing of dialysis in the first 48 hours after ACS should take into account individual risk factors. (C)
There are no data regarding the safety or risk associated with HD in the first 48 hours after ACS. Collaboration between nephrology teams and cardiology teams caring for these patients should take into consideration volume status, electrolyte disturbances, and bleeding potential. Dialysis prescriptions should be adjusted to maximize benefits while reducing the risk of hypotension during this vulnerable period.
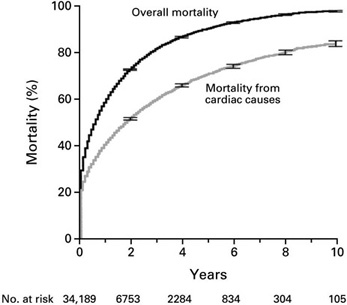
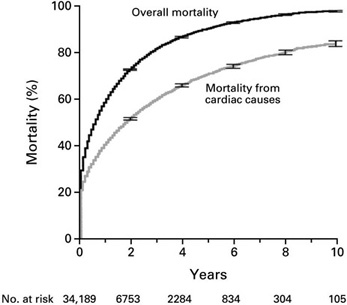
The mortality after acute MI (Fig 1) in dialysis patients has been reported to be approximately 75% in 2 years, in part due to inadequate post-MI treatment.7 Prophylactic care that is considered to be standard in the general population may improve upon this very poor outcome in dialysis patients. Therefore, the use of aspirin, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and thrombolytic therapy are recommended although controlled trials in dialysis patients are lacking. These therapies have been found to be protective in retrospective observational studies in various stages of CKD.8,59–61 Abciximab and tirofiban (glycoprotein platelet [GP] IIb/IIIa inhibitors) should also be considered as adjunctive therapy in ACS in dialysis patients. The use of adjunctive antithrombotic and antiplatelet agents during PCI presents special problems in dialysis patients, because of the increased risk of hemorrhage. Bivalirudin is a direct thrombin inhibitor specifically studied in dialysis patients with dosing recommendations and should be preferentially considered. When a GPIIb/IIIa antagonist is used, abciximab and tirofiban should be considered preferred agents, since no dosing changes are required for abciximab, and dialysis-specific dosing recommendations are available for tirofiban. Abciximab is typically used for PCI, as the clearance of the drug is not altered in dialysis patients. There are CKD—but not dialysis—patient studies dealing with this issue. One study reported safety of abciximab for Cr >2.0 mg/dL,62 while another showed no increase in bleeding for renal failure versus no renal failure for abciximab in PCI.63 However, increased bleeding with abciximab in renal failure has been reported.64 Increased bleeding but reduced in-hospital mortality in CKD patients with ACS treated with IIb/IIIa antagonists has also been shown.65(Weak)
Figure 1 - Estimated Mortality of Dialysis Patients after Acute MI. Reproduced with permission.