The assessment and treatment of both risk factors and end organs are essential in the management of cardiovascular diseases. The first section will deal with the end organs and will focus on cardiac, cerebrovascular and peripheral vascular diseases. Cardiac diseases have justifiably received the most attention because they are by far the most common cause of cardiovascular deaths in dialysis patients. Cerebrovascular diseases and peripheral vascular diseases, however, also lead to substantial morbidity and mortality and have often been overlooked by practitioners and clinical researchers.
The workgroup has faced dilemma in the scope and depth of the coverage of end organ diseases. There has been only one small randomized trial that demonstrated beneficial effects of specific cardioprotective drugs (namely, carvedilol) published in dialysis patients. Therefore, most guidelines described in this section are referred from published guidelines in the general population. Nonetheless, there are unusual features in the dialysis patients that the practitioners need to be aware of. For example, the pathophysiology and rate of progression of cardiac valvular calcification appear to be different from those in the general population. Surveillance and treatment strategies should take these caveats into consideration. On the other hand, the implant of tissue valves is proscribed in the existing ACC/AHA guidelines. More recent and stronger evidence, however, suggest that tissue valves are associated with equivalent outcomes in dialysis patients. These similarities, not only differences, between dialysis patients and the general population also need to be emphasized.
The section on end organ diseases is written for not only the nephrologists, but also the general practitioners, cardiologists, vascular surgeons and other practitioners.
Guideline 5: Valvular Heart Disease
The presence of valvular heart disease (VHD) impacts long-term outcomes, as in the general population. In addition, VHD in dialysis patients may impair the ability to adequately deliver dialysis, which, in turn, may limit ultrafiltration and toxin removal, resulting in exacerbation of CVD.
5.1 Evaluation of VHD in dialysis patients:
5.1a Patients should be evaluated for the presence of VHD and for follow-up of VHD in the same manner as the general population except for frequency of follow-up for aortic stenosis. (C)
5.1b Special considerations for echocardiographic evaluation in dialysis patients:
5.1bi Dry weight optimization should be achieved prior to testing, to enhance the interpretation of results. (B)
5.1bii The interpretation of repeat echocardiographic evaluations should be done with consideration of the relationship between the echo exam and either the HD treatment or the presence or absence of PD fluid in the peritoneal cavity. (B)
5.2 Management of VHD in dialysis patients:
5.2a Published recommendations for the management of VHD in the general population should be followed. (C)
5.2b Both mechanical and tissue valves can be used for replacement, with similar outcomes, in dialysis patients. (B)
5.2c Asymptomatic dialysis patients on the transplant waitlist with moderate or more severe aortic stenosis (aortic valve area ≤1.0 cm2) should have annual Doppler echocardiograms (as aortic stenosis progresses faster in dialysis patients than general population). The same frequency of follow-up is appropriate in other dialysis patients who would be suitable candidates for aortic valve replacement based on overall clinical status. (C)
5.2d Newly or increasingly symptomatic (e.g., displaying dyspnea, angina, fatigue, and unstable intradialytic hemodynamics) patients with VHD should be (re)-evaluated for VHD severity by echocardiography (and referred to a cardiologist for further evaluation if the patient is deemed suitable for intervention on clinical grounds). (C)
5.3 Children with VHD should be evaluated by echocardiography. Management of valvular disease should follow recommendation provided by the ACC/AHA Guidelines for the Management of Patients With Valvular Heart Disease VI.45(C)
Medical treatment
Cardiac calcification, including that of heart valves, occurs at a faster rate in dialysis patients compared to the general population. The rate of progression of aortic stenosis is faster in dialysis patients.76,77 A rate of aortic stenosis progression of 0.23 cm2/year versus 0.05–0.1 cm2/year has been reported in the general population.77 This is presumably a complication of the metabolic milieu of uremia, which includes hyperparathyroidism and high calcium-phosphate product (see the KDOQI Bone Metabolism and Disease Guidelines).78–80 It is uncertain whether pharmacological agents can alter the rate of progression of this process, although sevelamer has been shown to retard coronary arterial and aortic calcification specifically in the dialysis population, based on clinical data utilizing EBCT.81 In addition, statins have been suggested to inhibit calcification and bone formation in cardiac valves, currently the subject of a proposed clinical trial in the general population. (Weak)
Cardiac filling pressures are greatly affected by intravascular volume. The maintenance of dry weight is a critical part of the management of valvular heart disease.
Operative treatment (Weak)
Balloon valvuloplasty is not recommended for aortic stenosis in the general population because of poor long-term results due to re-stenosis, and it is also not recommended for dialysis patients. Severe mitral calcification (and mitral insufficiency) is quite common in dialysis patients, making mitral valvuloplasty inappropriate for many dialysis patients. Percutaneous balloon valvuloplasty of the mitral valve in dialysis patients should be performed only in centers with experienced operators.
The risk of in-hospital and long-term mortality associated with aortic and/or mitral valve replacement is considerably higher in the dialysis population compared to the general population. In the U.S., the in-hospital mortality of dialysis patients with valvular replacement surgery is almost 20% and the two-year mortality is approximately 60%.67
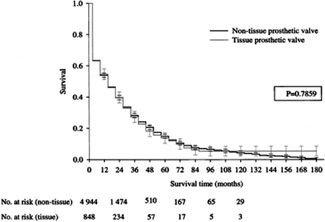
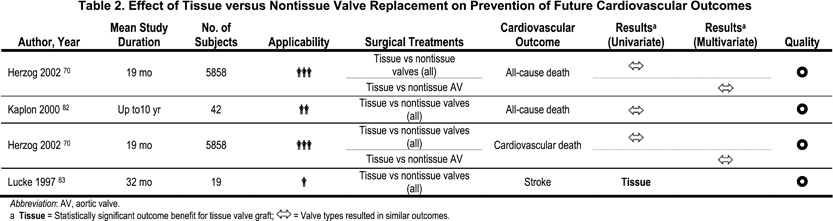
The selection of the type of prosthetic heart valve is the only practice guideline related to valvular heart disease that is at significant variance from the current ACC/AHA guidelines. The current ACC/AHA practice guidelines proscribe the use of bioprosthetic (i.e., tissue) heart valves for HD patients (Class III: “conditions for which there is evidence and/or general agreement that the procedure/treatment is not useful and in some cases may be harmful”). This proscription is based only on four cases collected over two decades ago, which led to the perception that bioprosthetic valves were associated with accelerated calcification and failure in HD patients. The more recent epidemiological data on 5,825 dialysis patients (4,545 were HD only, and there was no difference in the HD subset) undergoing cardiac valvular surgery from the USRDS found that approximately 900 patients had bioprosthetic valves. Similar findings are reported in smaller series on the noninferiority of bioprosthetic valves in dialysis patients (Table 2). There was no difference in two-year mortality (60%) in patients who received bioprosthetic valves (relative risk = 1.00) and those who received mechanical valves (Fig 3). Therefore, both tissue (bioprosthetic) and nontissue (mechanical) prosthetic heart valves are appropriate for dialysis patients. In dialysis patients with a history of life-threatening hemorrhage and no other indications for chronic anticoagulation, bioprosthetic valves may even be preferable.
Figure 3 - Estimated All-Cause Survival of Dialysis Patients after Heart Valve Replacement Surgery with Tissue and Nontissue Prosthetic Valves. Bars indicate standard errors.70 Reprinted with permission.