The assessment and treatment of both risk factors and end organs are essential in the management of cardiovascular diseases. The first section will deal with the end organs and will focus on cardiac, cerebrovascular and peripheral vascular diseases. Cardiac diseases have justifiably received the most attention because they are by far the most common cause of cardiovascular deaths in dialysis patients. Cerebrovascular diseases and peripheral vascular diseases, however, also lead to substantial morbidity and mortality and have often been overlooked by practitioners and clinical researchers.
The workgroup has faced dilemma in the scope and depth of the coverage of end organ diseases. There has been only one small randomized trial that demonstrated beneficial effects of specific cardioprotective drugs (namely, carvedilol) published in dialysis patients. Therefore, most guidelines described in this section are referred from published guidelines in the general population. Nonetheless, there are unusual features in the dialysis patients that the practitioners need to be aware of. For example, the pathophysiology and rate of progression of cardiac valvular calcification appear to be different from those in the general population. Surveillance and treatment strategies should take these caveats into consideration. On the other hand, the implant of tissue valves is proscribed in the existing ACC/AHA guidelines. More recent and stronger evidence, however, suggest that tissue valves are associated with equivalent outcomes in dialysis patients. These similarities, not only differences, between dialysis patients and the general population also need to be emphasized.
The section on end organ diseases is written for not only the nephrologists, but also the general practitioners, cardiologists, vascular surgeons and other practitioners.
Guideline 6: Cardiomyopathy (Systolic or Diastolic Dysfunction)
The prevalence of systolic or diastolic dysfunction, or overt LVH, is estimated to be at least 75% at dialysis initiation (see also Guideline 1). De novo and recurrent heart failure occurs in a substantial proportion of patients on dialysis, and impacts on morbidity and mortality, as well as the ability to deliver adequate dialysis.
6.1 Evaluation of cardiomyopathy (systolic or diastolic dysfunction) in dialysis patients:
6.1a Dialysis patients should be evaluated for the presence of cardiomyopathy (systolic or diastolic dysfunction) in the same manner as the general population, using echocardiographic testing. (C)
6.1b Patients should be re-evaluated if there is change in clinical status (e.g., symptoms of CHF, recurrent hypotension on dialysis, postcardiac events) or considered for kidney transplant. (C)
6.1c Echocardiograms should be performed in all patients at the initiation of dialysis, once patients have achieved dry weight (ideally within 1–3 months of dialysis initiation) (A), and at 3-yearly intervals thereafter. (B)
6.1d As in the general population, dialysis patients identified with significant reduction in LV systolic function (EF <40% should be evaluated for CAD (if not done previously). This evaluation may include both noninvasive testing (stress imaging) and invasive testing (coronary angiography). In patients at high risk for CAD (e.g., those with diabetic CKD), coronary angiography may be appropriate, even in patients with negative stress imaging test, due to lower diagnostic accuracy of noninvasive stress imaging test in CKD patients. (C)
6.2 The treatment of cardiomyopathy in the dialysis population is similar to that in the nondialysis population, with the important exception of potential effects of therapeutic agents (e.g., ACE inhibitors or beta-blockers) on intrahemodialytic hemodynamics. (C; B for carvedilol)
6.2a Congestive heart failure unresponsive to changes in target dry weight may also be a complication of unsuspected VHD or IHD; clinical re-evaluation should be considered in these patients. (C)
6.2b Dosing of therapeutic agents may need to be empirically individualized to hemodialysis schedules (in hypotensive patients). (C)
6.2c The consistent maintenance of euvolemia is a cornerstone of treatment of CHF in dialysis patients. (C)
6.3 Target “hemodynamic dry weight” may need to be adjusted to compensate for hemodynamic effects of therapeutic agents. (C)
6.4 Children should be evaluated for the presence of cardiomyopathy (systolic and diastolic dysfunction) using echocardiographic testing. (C)
Diagnosis (Moderately Strong)
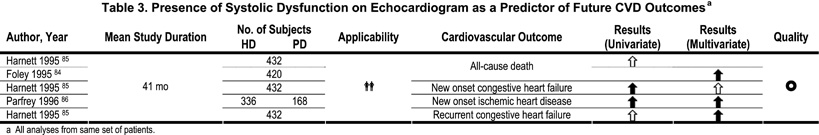
Congestive heart failure in dialysis patients is a complex condition. It often reflects the interaction of hypertensive heart disease (resulting in LVH and noncompliant vasculature), hypervolemia, anemia, IHD, and—to a lesser extent—VHD. In addition, there are abnormalities of the myocardial ultrastructure (e.g., fibrosis) that may make the dialysis patient particularly vulnerable to ischemia and, importantly, sudden cardiac death (SCD), the single largest cause of death in this population. Left ventricular hypertrophy, LV systolic dysfunction (decreased ejection fraction), and CHF are independent predictors of poor survival in dialysis patients, as in the general population. In one prospective cohort study84 abnormal LV systolic function and LV geometry were independently associated with mortality. Other studies also suggest the prognostic importance of echocardiographically-defined LV systolic dysfunction85,86 and LV mass84–88 as predictors of cardiovascular outcome (Table 3,Table 4). Left ventricular hypertrophy and systolic dysfunction cannot be accurately assessed solely by history, physical examination, or chest X-ray. Left ventricular systolic performance, however, can be accurately measured by echocardiography, gated nuclear scintigraphy, ultrafast CT, contrast ventriculography, or cardiac MRI.
Echocardiography (M-mode, 2-D, or Doppler) provides information on LV function, chamber dimension and geometry, presence of LVH, pulmonary artery systolic pressure, VHD, and volume status. No other single imaging modality provides this potential wealth of data in the screening of noncoronary heart disease.
Treatment (Moderately Strong)
The consistent maintenance of euvolemia and normal blood pressure is a goal of treatment. Good volume control is a cornerstone of antihypertensive therapy and cardiac management. Clinicians must be alerted to the changing lean body mass in these patients and adjust the target dry weight accordingly, on a periodic basis. When CHF appears to be refractory, ultrafiltration with simultaneous direct-pressure monitoring using right-heart catheterization (e.g., a pulmonary artery catheter) may be helpful to define the optimal intravascular volume. Echocardiography can provide key, noninvasive measurement of cardiac filling pressures and volume status with Doppler imaging for estimation of pulmonary artery pressure, pulmonary vein (and diastolic transmitral), qualitative assessment of pulmonary venous and left atrial pressure, and inferior vena cava (IVC) imaging for estimation of right atrial pressure. Optimal blood pressure in HD patients has not been defined clearly, and should probably incorporate predialysis and postdialysis systolic and diastolic blood pressures. Quotidian long-duration dialysis may be more effective in optimizing fluid volume in patients who have difficulty attaining presumed dry weight with conventional, thrice-weekly HD.
In the general population, large multicenter studies have validated the efficacy of certain agents for the treatment of CHF in patients with impaired LV systolic function. Agents that are known to improve cardiovascular outcome in clinical trials (e.g., beta-blockers) are preferred. Special dosing regimens may be necessary to facilitate the delivery of HD and ultrafiltration. Among all the medications used to treat CHF in the general population, only carvedilol has been shown to be effective in a randomized trial in the dialysis population. In a single, small study of dialysis patients with dilated cardiomyopathies, carvedilol was found to improve LV function and decrease hospitalization, cardiovascular deaths and total mortality.89,90 The degree of improvement was comparable to that observed in the general population. Other beta-blockers may have effects similar to carvedilol, but there are no studies to confirm or refute this hypothesis. Pending further data, carvedilol should be the preferred beta-blocker for the treatment of dialysis patients with severe dilated cardiomyopathy. (Moderately Strong)
Angiotensin-converting enzyme inhibitors have been used extensively in the general population for the treatment of CHF. In randomized placebo-controlled trials, ACE inhibitors have been shown to improve survival in patients with depressed LV function and symptomatic heart failure, and to improve survival in asymptomatic patients with depressed LV function. However, minimal data exist on the use of ACE inhibitors in dialysis patients with CHF. Nonetheless, the Work Group recommends that these agents be used in patients with CHF and impaired LV function. The dosing schedules may need to be individualized for each dialysis session in order to avoid intradialytic hypotension. One randomized prospective study, employing a 2 × 2 design on simvastatin and enalapril, found a 30% 6-month drop-out rate as a result of hypotension in the enalapril arm.91(Weak)
Digitalis glycosides (e.g., digoxin) should be considered as third-line therapy for CHF. A major indication for this class of agent is ventricular rate control in patients with atrial fibrillation. In most dialysis patients, diuretics are ineffective and not indicated for removing excess volume. There is a paucity of data on the use of spironolactone or eplerenone in dialysis patients with CHF. Serum potassium levels have been reported to increase in dialysis patients receiving spironolactone and potassium loading. Pending further safety data, this agent should be used with great caution, or not at all. (Weak)
Although echocardiography is widely available, the cost is not low, and this may deter its use. Further, the detection of cardiac abnormalities (such as LV dysfunction) may increase the necessity for other diagnostic tests, such as stress imaging or contrast angiography, for the assessment of CAD.