The assessment and treatment of both risk factors and end organs are essential in the management of cardiovascular diseases. The first section will deal with the end organs and will focus on cardiac, cerebrovascular and peripheral vascular diseases. Cardiac diseases have justifiably received the most attention because they are by far the most common cause of cardiovascular deaths in dialysis patients. Cerebrovascular diseases and peripheral vascular diseases, however, also lead to substantial morbidity and mortality and have often been overlooked by practitioners and clinical researchers.
The workgroup has faced dilemma in the scope and depth of the coverage of end organ diseases. There has been only one small randomized trial that demonstrated beneficial effects of specific cardioprotective drugs (namely, carvedilol) published in dialysis patients. Therefore, most guidelines described in this section are referred from published guidelines in the general population. Nonetheless, there are unusual features in the dialysis patients that the practitioners need to be aware of. For example, the pathophysiology and rate of progression of cardiac valvular calcification appear to be different from those in the general population. Surveillance and treatment strategies should take these caveats into consideration. On the other hand, the implant of tissue valves is proscribed in the existing ACC/AHA guidelines. More recent and stronger evidence, however, suggest that tissue valves are associated with equivalent outcomes in dialysis patients. These similarities, not only differences, between dialysis patients and the general population also need to be emphasized.
The section on end organ diseases is written for not only the nephrologists, but also the general practitioners, cardiologists, vascular surgeons and other practitioners.
Guideline 7: Dysrhythmia
Patients on maintenance dialysis are at increased risk for dysrhythmias, cardiac arrest, and SCD. The risk of SCD or cardiac arrest increases with age and dialysis duration.
7.1 Evaluation of dialysis patients:
7.1a All dialysis patients, regardless of age, should undergo a routine 12-lead ECG at the initiation of dialysis. (C)
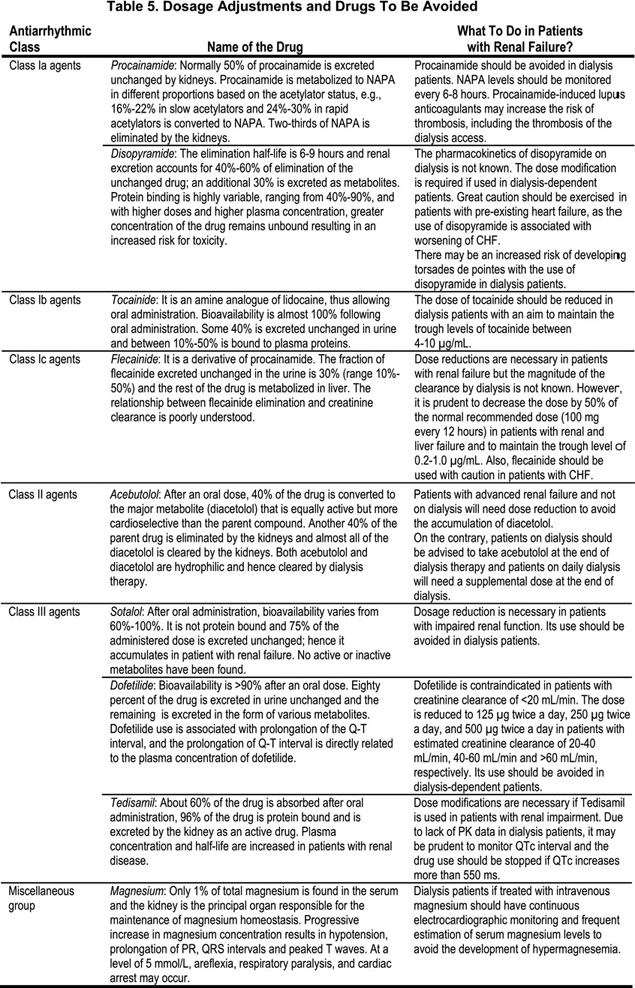
7.1b Patients with dysrhythmias should be treated in the same manner as the general population with regard to antiarrhythmic agents (including beta-blockers) and pacing devices (including internal defibrillators). Refer to Table 5 for dosage adjustments and drugs to be avoided. (C)
Risk factors
Patients on maintenance dialysis therapy are at increased risk for dysrhythmias, cardiac arrest, and SCD. Dialysis patients with underlying structural or functional CVD are at much higher risk for these dysrhythmias and cardiac arrest because of increased dysrhythmogenicity due to dynamic changes in electrolytes, volume status, blood pressure and the use of multiple medications. Even nondiabetic dialysis patients have a markedly increased cardiac event rate and decreased event-free survival as compared to the general population.93(Moderately Strong)
Ischemic heart disease is present in many patients even at the time of initiation of dialysis. CKD Stage 5 patients with either symptomatic or asymptomatic coronary artery disease are at increased risk for dysrhythmias and SCD.94–97 This risk is potentiated with concomitant presence of anemia98 and left ventricular hypertrophy99 or increased left ventricular mass index, often present in CKD patients at the initiation of dialysis therapy.100,101(Weak)
The prevalence of baseline ECG abnormalities and the development of new dysrhythmias and silent myocardial ischemia is related to the concomitant presence of CAD, and is also directly proportional to the duration of dialysis.102–105 Potentially life-threatening ventricular dysrhythmias and silent myocardial ischemia were noted in 29% and 36%, respectively, on Holter monitor performed 24 hours before, during HD, and continued for 20 hours after dialysis in a small cohort of 38 HD patients.105 Furthermore, atrial dysrhythmias were noted in 10% of patients in a cohort of 106 maintenance HD patients106 and 76% of patients demonstrated varying degrees of ventricular dysrhythmias in a cohort of 127 maintenance dialysis patients.102 The risk of new onset dysrhythmias was shown to increase in patients on peritoneal dialysis (PD), with ventricular dysrhythmias increasing from 30% to 43% and supraventricular dysrhythmias (SVA) increasing from 40% to 57%, respectively, during a mean follow-up period of 20 ±4 months.107(Moderately Strong)
Risk factors for increased arrhythmogenicity include compromised myocardium (due to either underlying CAD, decreased coronary reserve blood flow, or the consequences of uremia on myocardial function and structure), increased QTc interval or dispersion, electrolyte abnormalities, intradialytic hypotension, concomitant presence of LVH (present in almost 80% patients on dialysis), and autonomic dysfunction (with or without diabetes).108–110(Moderately Strong)
Dialysis patients have frequent electrolyte abnormalities such as fluctuating levels of potassium, ionized calcium, magnesium, and other divalent ions.111 Due to the intermittent nature of the dialysis procedure, patients on HD have wide fluctuations in volume status, and potassium and bicarbonate levels, in between dialysis treatments.97,112 These fluctuations are partly driven by the level of potassium and calcium in the dialysate fluid used during the prior session of treatment, and wide variability in eating habits due to varying adherence to dietary modifications necessary to control the calcium-phosphate product.112–115 All these factors culminate in an dysrhythmogenic diathesis. (Weak)
Atrial fibrillation (A.fib) is perhaps the most commonly diagnosed dysrhythmia in the general population, and also in the dialysis population.106 A historical cohort study of the USRDS DMMS Wave 2 revealed that A.fib was more common in dialysis patients than in the general population, although the study did not showwhether A.fib was related or unrelated to valvular disease.116(Weak)
Treatment
There is strong evidence for the use of different interventions either for primary or secondary prevention of arrhythmias and cardiac arrest in the high-risk general population (patients with CAD,117–120 CHF121,122 and near-fatal cardiac events123–126). Since dialysis patients are at increased risk for CV events, it is reasonable to assume that these interventions will be effective, despite the lack of evidence in the dialysis population. Pending further research, there is presently no reason to withhold these interventions in dialysis patients. (Moderately Strong)
The use of beta-blockers in nondialysis patients is recommended for the primary prevention of SCD,127 and improves outcomes in patients with CHF.128,129 Similarly, the USRDS Wave 3 and 4 study showed decreased risk of death in patients who were on beta-blockers.130,131 A small study demonstrated that dialysis patients may not tolerate sotalol due to an increased risk of torsade de pointes.132,133(Weak)
The use of novel agents such as Ximelagatran, direct thrombin inhibitor, fixed-dose therapy without coagulation monitoring as an alternative to coumadin therapy for the prevention of strokes in patients with nonvalvular A.fib, has been demonstrated to be effective in the general population.134–136 However, the use of Ximelagatran in dialysis patients has not been studied. (Weak)
The use of internal defibrillators may be precluded due to: