The assessment and treatment of both risk factors and end organs are essential in the management of cardiovascular diseases. The first section will deal with the end organs and will focus on cardiac, cerebrovascular and peripheral vascular diseases. Cardiac diseases have justifiably received the most attention because they are by far the most common cause of cardiovascular deaths in dialysis patients. Cerebrovascular diseases and peripheral vascular diseases, however, also lead to substantial morbidity and mortality and have often been overlooked by practitioners and clinical researchers.
The workgroup has faced dilemma in the scope and depth of the coverage of end organ diseases. There has been only one small randomized trial that demonstrated beneficial effects of specific cardioprotective drugs (namely, carvedilol) published in dialysis patients. Therefore, most guidelines described in this section are referred from published guidelines in the general population. Nonetheless, there are unusual features in the dialysis patients that the practitioners need to be aware of. For example, the pathophysiology and rate of progression of cardiac valvular calcification appear to be different from those in the general population. Surveillance and treatment strategies should take these caveats into consideration. On the other hand, the implant of tissue valves is proscribed in the existing ACC/AHA guidelines. More recent and stronger evidence, however, suggest that tissue valves are associated with equivalent outcomes in dialysis patients. These similarities, not only differences, between dialysis patients and the general population also need to be emphasized.
The section on end organ diseases is written for not only the nephrologists, but also the general practitioners, cardiologists, vascular surgeons and other practitioners.
Guideline 9: Cerebrovascular Disease
Stroke is the third leading cause of death in the general population in the U.S. and many other countries, with large economic and human burdens as a consequence. Patients with CKD are at increased risk for stroke relative to the general population.
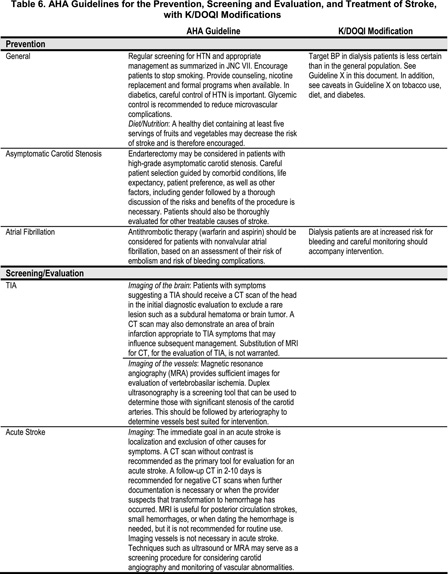
9.1 All dialysis patients should follow the AHA Guidelines for the prevention, screening and evaluation, and treatment of stroke. A summary of the AHA guidelines with any caveats related to dialysis patients is shown in Table 6.(C)
9.2 Special considerations in dialysis patients include:
9.2a Anticoagulation in nonvalvular atrial fibrillation: Dialysis patients are at increased risk for bleeding and careful monitoring should accompany intervention. (C)
9.2b Acute stroke in dialysis patients: Given that acute stroke syndromes can be due to either thrombotic or bleeding events in dialysis patients, the immediate goal of localization and cause is particularly important in dialysis patients because of increased risk of bleeding associated with anticoagulants in this population. Therefore, imaging with established methods should be undertaken. (C)
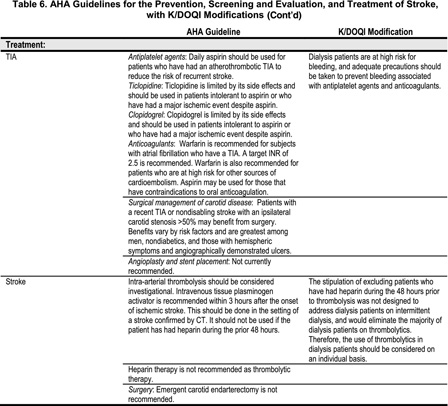
9.3 Treatment of stroke and transient ischemic attack (TIA):
9.3a Treatment of TIAs and strokes should follow the same principles used in the general population for both medical management and surgical management, with the exception of thrombolytics in HD patients. (C)
9.3ai Assessment of the risk of bleeding in patients recently receiving heparin on dialysis should be conducted when considering the use of thrombolytics. (B)
Prevention
Few studies have identified risk factors for stroke in the dialysis population. The available data suggest that high blood pressure, markers of poor nutrition, age, diabetes, and ethnicity place patients at greatest risk. Of these factors, only blood pressure and nutrition are potentially modifiable. The largest study assessing risk factors for stroke used data from the United States Renal Data System (USRDS). Several factors were found to be associated with stroke.139 African-Americans with a history of CVD had a lower risk for incident stroke than Caucasians. Lower serum albumin, subjective malnutrition and lower weight were associated with a higher risk for stroke. Higher blood pressure, older age, and diabetes were also associated with a higher risk for stroke. There was no association between incident stroke and cholesterol, calcium, phosphorus, or parathyroid hormone. Measures of malnutrition and diabetes were not associated with hemorrhagic stroke, while polycystic kidney disease, African-American race without a history of CVD, and male gender were associated with a higher risk for hemorrhagic stroke. Data from Japan identified polycystic kidney disease, higher blood pressure, higher ECG voltage, and lower KT/V as risk factors for cerebral hemorrhage.140 A small study from Japan demonstrated that hypertension was a risk factor for stroke.141 Factors not found to be associated with stroke included male gender, age, diabetes, smoking, dyslipidemia, and duration of dialysis. However, a survival analysis was not performed and statistical power was limited. The epidemiology of stroke is different in Japan and caution should be used when generalizing these data to U.S. dialysis patients.
Screening/evaluation
There are some data to suggest that dialysis patients have higher measures of subclinical vascular disease142 and that these measures predict cardiovascular events and death. Carotid ultrasound measurements of elasticity or arterial stiffness measured in the common carotid artery assessing incremental modulus of elasticity have demonstrated a positive relationship between arterial stiffness and cardiovascular mortality.92 Greater carotid intimal medial thickness has also been shown to be associated with a greater risk for cardiovascular events.143 Carotid artery incremental elastic modulus has been associated with an increased risk for cardiovascular events. Each one standard deviation increase was associated with a 1.7-fold increased risk for cardiovascular events.92 There are no studies that have assessed whether these measures predict stroke specifically, or if screening decreases events. Routine screening using carotid ultrasound is not recommended in asymptomatic patients.