The following sections have been prepared to ensure that the state of the art and science related to CVD includes novel concepts, therapeutic strategies, and emerging areas of pathophysiological and practical importance to the care of dialysis patients.
The reader will notice that the format of this section is different, reflecting its different perspective: namely, the relative lack of evidence on which to base plausible guideline statements. The evidence that does exist, and is cited in this section, is either completely in nondialysis populations, or is purely associative information, with no intervention in any population yet tested. Thus, it would be a problem to include guideline statements or recommendations.
Nonetheless, this section describes the current status of knowledge with respect to risk factors and biomarkers, and represents an overview of key areas for future clinical trials. The reader is encouraged to review this section, and examine his or her current understanding and practice within the context of these highlights.
The literature review has been conducted using the same systematic strategy as for the previous guidelines in this document. The reviews presented here have been thoughtfully constructed so that clinicians can adopt different practices based on them. However, for reasons cited above, the ability to truly recommend or suggest changes in practice would be premature at this time.
Patients arrive at CKD Stage 5 with significant cardiovascular risk factors and, once on dialysis, they die at a more rapid rate than would be predicted by their Framingham risk factors alone. Recently, much interest has focused on the role of nontraditional risk factors for atherosclerosis, such as an excessive inflammatory response. Although the concept that inflammation plays a central role in the pathophysiology of atherosclerosis has gained a lot of recent interest, we do not know yet whether inflammation reflects vascular injury or is instead a cause of vascular injury. However, recent data suggest that inflammatory biomarkers, such as interleukin-6 (IL-6) and the archetypal acute phase reactant C-reactive protein (CRP), are not only markers but also mediators of atherothrombotic disease in man. In the general population, high-sensitive C-reactive protein (hs-CRP) appears to be the best inflammatory biomarker employed to detect enhanced absolute risk of CVD. Moreover, there is evidence supporting the use of CRP in primary prevention of CVD; in fact, CRP may be a stronger predictor of cardiovascular events than the LDL-cholesterol level. It has been speculated that a persistent inflammatory response may mediate malnutrition (i.e., wasting) and progressive atherosclerotic CVD by a number of pathogenic mechanisms.
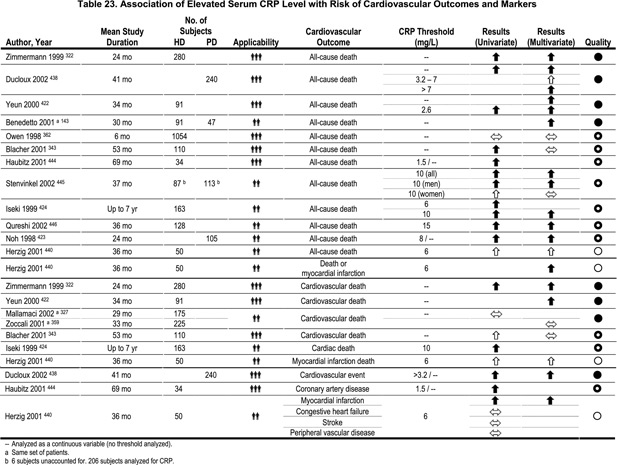
Whereas chronic inflammation is a common phenomenon in European420 and North American421,422 CKD patients, the prevalence of inflammation seems to be lower in Asian CKD patients (Table 23).423,424 This suggests that genetic factors and/or cultural habits (such as food intake) may affect the inflammatory response in dialysis patients. Recent studies suggest that a reduction of kidney function per se may be associated with an inflammatory response, both in mild CKD425 and advanced kidney failure.426,427 Factors common in dialysis patients, such as clotted access grafts,428 failed kidney grafts429 atherosclerosis,430 and persistent infections431,432 may contribute to an acute-phase response, thus elevating inflammatory biomarkers such as CRP and IL-6.
A recent evaluation of a historical cohort of 393,451 U.S. dialysis patients demonstrated that septicemia was associated with increased cardiovascular death risk.433 Although the association between CVD and inflammation is well documented in CKD patients,434,435 we do not know if the acute-phase response merely reflects established atherosclerosis or if acute-phase reactants are actually involved in the initiation and progression of atherosclerosis. However, an increasing body of evidence suggests that CRP may be directly involved in atherothrombogenesis that extends beyond its previously accepted role as an inflammatory marker. Thus, CRP and other biomarkers of inflammation, such as IL-6, TNF-α, and fibrinogen, may contribute to atherogenesis.436 The circulating calcification inhibitor, fetuin-A, has recently attracted interest as its level decreases during chronic inflammation, and patients with low serum fetuin-A levels showed a significantly poorer survival rate compared to those with normal or high-normal values.437 Several studies have shown that elevated CRP predicts all-cause and cardiovascular mortality in both HD322,422,424 and PD423,438,439 patients. Moreover, in PD patients, elevated CRP was independently shown to predict nonfatal myocardial infarction440 and increased incidence of CVD.438 Also, recent data from the MDRD study (n=801) showed that, after adjusting for traditional CVD risk factors, the odds of CVD were 1.73 times greater in patients with high CRP levels.421 Further support for linking inflammation to poor outcomes is evident from two recent large studies of 7,719441 and 25,661442 HD patients, respectively, showing a direct association between neutrophil counts and mortality.
In the current evaluation (Table 23), we have defined inflammation as elevated CRP (usually defined as a serum level >5–10 mg/L). In some studies, other inflammatory markers such as IL-6, have been used to assess the presence of inflammation. Most studies with high applicability did show that elevated CRP predicted all-cause mortality in dialysis patients.322,359,422,438,439 Notably, in the only study in which no significant relationship was observed between the odds risk of death and CRP,362 the observation period was only 6 months. Most studies with high applicability322,422,439 also showed that elevated CRP predicted cardiovascular mortality in CKD. The majority of papers with a lower level of applicability also show that elevated CRP predicts all-cause mortality and/or are associated with cardiovascular disease. Taken together, the presence of inflammation predicts both all-cause and cardiovascular mortality in CKD patients.
There is no consensus in the literature with regard to the optimal “cut-off” point of CRP used to define the presence of inflammation in CKD patients. Moreover, most studies have used only a single determination of CRP (or IL-6), which may be problematic since inflammatory biomarkers vary with time in dialysis patients.443 Difficulties and differences in the definition of cardiovascular mortality may also limit the applicability of the present studies. Also, there are no controlled studies in which the effects of various anti-inflammatory treatment strategies have been evaluated in this patient population. Finally, the cost-effectiveness of CRP screening in dialysis patients has not been evaluated.
Future research should aim at finding the optimal “cut-off” point at which elevated CRP predicts outcome in CKD. Studies are needed to investigate the possible interactions between the presence of inflammation and both traditional risk factors (such as dyslipidemia) and nontraditional risk factors (such as oxidative stress, vascular calcification, advanced glycation end-products and endothelial dysfunction) for atherosclerosis. Research is also required to investigate the impact of age, gender, physical activity, diet, race and genetic factors on the prevalence of inflammation in CKD. Nonpharmacological and pharmacological interventions for patients with signs of inflammation should be developed and evaluated for efficacy in reducing inflammation and improving clinical outcomes in this patient group. The independent role of potential proatherogenic inflammatory biomarkers such as CRP, fetuin-A, and IL-6, in the processes of atherogenesis and progression, need to be tested in the uremic milieu.
Based on the studies reviewed, CRP predicts outcomes and improves risk prediction. Therefore, it would be beneficial to assess CRP levels in dialysis patients on a regular basis, and to seek sources of infection or inflammation. A highly sensitive method for measuring CRP is recommended. Various causes of inflammation may be identified in dialysis patients. Overt and occult infectious processes (such as clotted arteriovenous grafts) require appropriate treatment. Factors associated with dialysis treatments that may provoke an inflammatory response include impure dialysate (due to endotoxin or bacterial contamination), back-filtration, and bioincompatible dialysis membranes.