The following sections have been prepared to ensure that the state of the art and science related to CVD includes novel concepts, therapeutic strategies, and emerging areas of pathophysiological and practical importance to the care of dialysis patients.
The reader will notice that the format of this section is different, reflecting its different perspective: namely, the relative lack of evidence on which to base plausible guideline statements. The evidence that does exist, and is cited in this section, is either completely in nondialysis populations, or is purely associative information, with no intervention in any population yet tested. Thus, it would be a problem to include guideline statements or recommendations.
Nonetheless, this section describes the current status of knowledge with respect to risk factors and biomarkers, and represents an overview of key areas for future clinical trials. The reader is encouraged to review this section, and examine his or her current understanding and practice within the context of these highlights.
The literature review has been conducted using the same systematic strategy as for the previous guidelines in this document. The reviews presented here have been thoughtfully constructed so that clinicians can adopt different practices based on them. However, for reasons cited above, the ability to truly recommend or suggest changes in practice would be premature at this time.
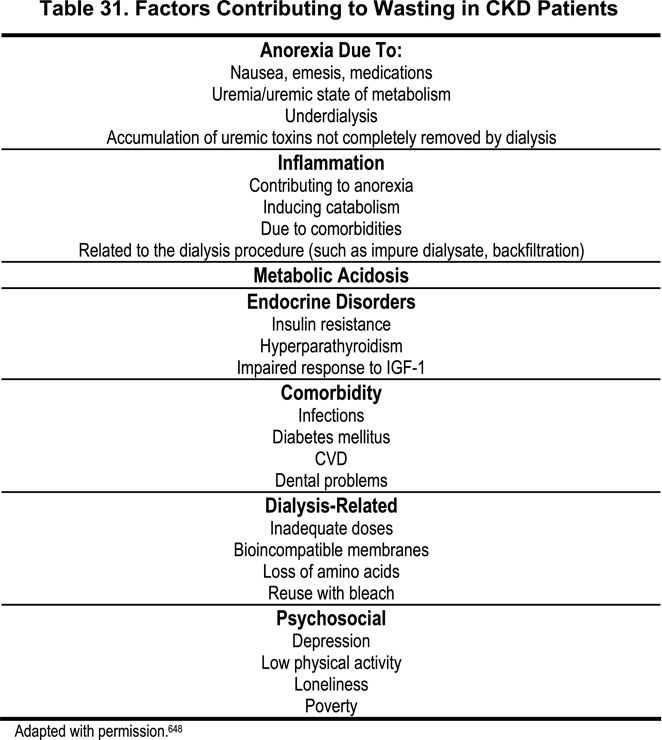
Protein-energy malnutrition (PEM) and wasting are common among CKD patients,635–637 and are associated with higher rates of morbidity and mortality.169,441,635,638,639 Although various factors associated with the dialysis procedure, per se (such as dialyzer membrane bio-incompatibility, and nutrient losses), may contribute to PEM, recent studies have shown that malnutrition is also common before the start of dialysis.434,638 Various factors contributing to malnutrition in CKD patients are presented in Table 31. The decline in nutritional status during the course of progressive kidney failure may be caused by disturbances in protein and energy metabolism, hormonal derangement, as well as by spontaneous reductions in dietary energy and protein intake.640 However, as it has been demonstrated that patients treated with HD for a long time become malnourished despite adequate dialysis dose and protein intake,641 several co-morbid conditions may also contribute to PEM among dialysis patients. In particular, chronic inflammation, CVD, diabetes mellitus, and other superimposed illnesses may produce anorexia and malnutrition. It was recently reported that diminished appetite (anorexia) was associated with higher concentrations of proinflammatory cytokines.642 Evidence suggests that the presence of PEM is associated with inflammation in CKD patients.421,434,643,644 Moreover, both PEM at baseline and worsening of PEM over time are associated with a greater risk for cardiovascular death in dialysis patients328,645 and strong associations between the presence of malnutrition and CVD have been documented both in predialysis434 and dialysis643 populations. On the other hand, a recent study646 documented no association between BMI and hospitalized acute coronary syndromes in a large group of incident Medicare dialysis patients. The exact mechanism(s) by which PEM may increase the risk of CVD are not known. However, as PEM and low BMI recently have been associated with both increased oxidative stress475,647 and impaired endothelium-dependent vasodilation with reduced bioavailability of nitric oxide,647 these may be mechanisms that contribute to the high prevalence of CVD in malnourished CKD patients. As nutritional status is so strongly associated with outcome, it is important to define which nutritional indicators to use in the clinical setting. However, the optimal protocol to diagnose and monitor the response to nutrition intervention has not yet been defined. Therefore, the current approach is to integrate parameters that have been shown to have nutritional relevance; i.e., clinical assessment, food intake, biochemical assessment, body weight, body composition, and psychosocial evaluation.
Validity of serum albumin as a nutritional marker
Over the past few years, the process of nutrition assessment and management of the CKD patients has been presented with new challenges regarding validity and reliability. This is largely due to the fact that parameters previously relied upon for visceral stores assessment, predominantly serum albumin (and, to a lesser extent, prealbumin), are independently altered by systemic inflammation. Several studies have demonstrated that a low serum albumin concentration is strongly associated with both mortality181,362,441,479,649 and cardiac disease479 in CKD patients maintained on either PD or HD. Moreover, among 1,411 HD patients enrolled in the HEMO study, patients in the low albumin group had significantly greater prevalence of CHD.650 However, in studies in which the effect of inflammation (measured by CRP levels) is also accounted for in multiple-regression analysis, low serum albumin levels tend to lose predictive power,322,422,445suggesting that inflammation may be a more powerful predictor of poor outcome. Indeed, in two recent studies of 7,719441 and 25,661442 HD patients, respectively, the risk of mortality was directly associated with the neutrophil count. The interactions between inflammation and nutritional status may be complex, as inflammation and dietary protein intake exert competing effects on serum albumin levels.651 In fact, inflammation may cause the same changes in serum protein levels and body composition as PEM, even with adequate calorie and protein intake. Recent studies have shown that inflammatory cytokines, such as TNF-α and IL-6, are associated with protein synthesis and catabolism in the body, and downregulate albumin synthesis.652 The poor correlation documented between serum albumin and other nutritional parameters445,653 implies that non-nutritional factors actually may be more important in determining serum albumin levels than dietary intake and nutritional status per se in CKD patients. Indeed, a number of factors other than protein intake and nutritional status may affect the serum albumin concentration in CKD patients (Table 32). Beside inflammation, age and co-morbidities, such as CVD and diabetes, have been shown to be strongly associated with serum albumin levels in CKD patients.445,654,655 Moreover, external albumin losses, such as albuminuria and losses in dialysate, may significantly contribute to hypoalbuminemia in CKD.655 Finally, over-hydration, which is a common feature in dialysis patients, may also contribute to low serum albumin levels.
Among a number of other available biochemical nutritional indicators, prealbumin and serum creatinine may have unique validity, when researchers reach a more detailed mechanistic understanding of their functions. Prealbumin is curiously misnamed, as it is not structurally related to albumin in any way, but is in fact the thyroxin-binding protein, transthyretin. Transthyretin levels are more sensitive to nutritional status than serum albumin levels. Both are suppressed when hepatic protein synthesis switches to the production of acute-phase proteins, but transthyretin levels change more rapidly. Therefore, transthyretin represents a good index of liver anabolic protein synthesis. However, the clinical picture is complicated, because transthyretin is reabsorbed and/or metabolized by the proximal tubule.656 Therefore, serum levels of transthyretin rise as kidney function declines.442 Nonetheless, transthyretin levels correlate strongly with serum albumin and have been shown to provide prognostic value independent of albumin in HD patients.657 Because serum creatinine concentration reflects muscle mass, somatic protein stores, and dietary protein intake, and also predicts outcome in CKD,181 it may be another useful marker of nutritional status in CKD. However, creatinine levels are also affected by inflammation and other factors such as age, sex, race, residual kidney function, variation in creatinine metabolism, and dialysis dose.441,651
Other potentially useful nutrition markers
Clearly, other nutritional indices are needed to assess nutritional status in CKD. Ideally, a nutritional marker should not only predict outcome, but it should also be an inexpensive, reproducible, and easily performed test that is not affected by such factors as inflammation, gender, age, and systemic diseases. Unfortunately, no such ideal nutritional marker is available at present. Thus, the use of a broad panel of putative indicators may best facilitate the epidemiological and clinical assessment of nutritional status (Table 33). The assessment of dietary intake has been commonly used to assess nutritional status. In particular, the normalized protein catabolic rate (nPCR) has been widely used as a measure of dietary protein intake, assuming a state of protein balance. Indeed, nPCR is much simpler to determine than dietary protein intake from diet diaries or interviews.658 However, a recent study observed no relationship between mortality and either baseline or 6-month follow-up measurements of nPCR in 7,719 U.S. adult HD patients,441 raising doubt about the clinical usefulness of this nutritional parameter.
Several methods have been used to monitor lean body mass in CKD, e.g., anthropometrics, creatinine kinetics, multifrequency bioimpedance (BIA) and DEXA. Of these, DEXA seems to be the most reliable, especially if serial measurements are made.659 However, to the best of our knowledge, no studies have yet evaluated whether lean body mass (by DEXA) predicts outcomes and/or is associated with CVD. By using DEXA, a reliable estimation of the amount of body fat mass can also be done. However, as DEXA is not widely available, other nutritional indicators are needed.660 Although measures such as BIA and handgrip muscle strength (HGS) are practical and convenient, they, too, suffer from limitations.661–663
Subjective global assessment (SGA), on the other hand, is widely available and seems to be a reliable predictor of poor outcome in both sexes (Table 34).445 It is a combined subjective and objective test of the patient’s medical history and physical examination, including recent weight loss, dietary intake, gastrointestinal symptoms and visual assessment of subcutaneous fat.664,665 In addition, several large prospective studies have demonstrated that SGA is a reliable predictor of poor outcome in dialysis patients, suggesting that it provides a meaningful assessment of nutritional status.441,635 Although SGA has several advantages, such as its low cost, rapid performance, and strong predictive value for mortality, it should be appreciated that visceral proteins are not assessed and that the sensitivity, precision and reproducibility over time of SGA have not been well studied. In a recent study, it was found that whereas SGA may not be a reliable predictor of degree of protein malnutrition (as assessed by total body nitrogen), it may differentiate severely malnourished patients from those with normal nutrition.666
Studies are needed to identify the incidence of hypoalbuminemia due to visceral protein store depletion vs. hypoalbuminemia due to chronic inflammation. Effective nutrition and medical management interventions need to be identified that are specific for malnutrition vs. inflammation vs. metabolic challenges. Studies are also required to examine how long-term nutritional intervention affects cardiovascular risk and specific risk factors for accelerated atherosclerosis, such as oxidative stress and endothelial dysfunction, in CKD patients.
Protein-energy malnutrition and wasting are strong predictors of mortality among CKD patients. Although several biochemical and anthropometric measurements correlate with nutritional status, there is not a single measurement that provides complete and unambiguous assessment. While serum albumin is a robust and well-documented indicator of mortality risk in CKD patients, its value as a nutritional marker has been questioned because levels are affected by a number of non-nutritional factors. As SGA is a simple and inexpensive indicator that predicts outcome, this test could be useful in identifying malnourished CKD patients at high risk. The utility of the SGA for nutrition assessment and management of this patient population requires further verification. At present, the use of a broad panel of nutritional indicators, such as BMI, SGA, handgrip strength (or other measure of muscle mass), waist circumference, serum albumin, and serum creatinine may be the best approach to provide useful information about the nutritional status in any given clinical situation.