The overall aim of the project was to develop clinical practice guidelines for the evaluation and management of CVD in CKD patients who require either HD or PD.
The Work Group sought to develop the guidelines using an evidence-based approach. Evidence regarding the guideline topics was derived from a systematic summary of the available scientific literature on the epidemiology of CVD among dialysis patients, the evaluation and management of cardiac, cerebrovascular, and peripheral vascular disease among dialysis patients, the evaluation and management of specific risk factors for CVD among dialysis patients, and cardiovascular risk stratification among dialysis patients.
Development of the guideline and evidence report required many concurrent steps to:
The Co-Chairs of the KDOQI Advisory Board selected the Work Group Co-Chairs and Director of the Evidence Review Team, who then assembled groups to be responsible for the development of the guidelines and the evidence report, respectively. These groups collaborated closely throughout the project.
The Work Group consisted of “domain experts,” including individuals with expertise in nephrology, epidemiology, cardiology, nutrition, social work, pediatrics, and internal medicine. In addition, the Work Group had a liaison member from the Renal Physicians Association. The first task of the Work Group members was to define the overall topic and goals, including specifying the target condition, target population, and target audience. They then further developed and refined each topic, literature search strategy, and data extraction form (described below). The Work Group members were the principal reviewers of the literature, and from these detailed reviews, they summarized the available evidence and took the primary roles of writing the guidelines and rationale statements.
The Evidence Review Team consisted of nephrologists (two senior nephrologists and a nephrology fellow) and methodologists from Tufts-New England Medical Center with expertise in systematic review of the medical literature. They were responsible for coordinating the project, including coordination of meetings, refinement of goals and topics, creation of the format of the evidence report, development of literature search strategies, initial review and assessment of literature, and coordination of all partners. The Evidence Review Team also coordinated the methodological and analytical process of the report, coordinated the meetings, and defined and standardized the methodology of performing literature searches, of data extraction and of summarizing the evidence in the report. They performed literature searches, retrieved and screened abstracts and articles, created forms to extract relevant data from articles, and tabulated results. Throughout the project, and especially at meetings, the Evidence Review Team led discussions on systematic review, literature searches, data extraction, assessment of quality and applicability of articles and the body of evidence, and summary reporting.
The goals of the Work Group targeted a diverse group range of topics, which would have been too large for a comprehensive review of the literature. Based on their expertise, members of the Work Group focused on the specific questions, and employed a selective review of evidence: a summary of reviews for established concepts (review of textbooks, reviews, guidelines and selected original articles familiar to them as domain experts); and a review of primary articles and data for new concepts.
The Work Group and Evidence Review Team developed a) draft guideline statements; b) draft rationale statements that summarized the expected pertinent evidence; and c) data extraction forms requesting the data elements to be retrieved from the primary articles. The topic refinement process began prior to literature retrieval and continued through the process of reviewing individual articles.
Data extraction forms were designed to capture information on various aspects of the primary articles. Forms for all topics included study setting and demographics, eligibility criteria, causes of kidney disease, numbers of subjects, study design, study funding source, dialysis characteristics, comorbid conditions, descriptions of relevant risk factors and cardiovascular outcomes, statistical methods, results, study quality (based on criteria appropriate for each study design, see below), study applicability (see below), and sections for comments and assessment of biases.
Training of the Work Group members to extract data from primary articles occurred at meetings, and subsequently by e-mail and during teleconferences.
The Work Group and Evidence Review Team decided in advance that a systematic process would be followed to obtain information on topics that relied on primary articles. Only full journal articles of original data were included. Editorials, letters and abstracts were not included. Selected review articles were included for background material. Though reports of formal studies were preferred, case series were also included. No systematic process was followed to obtain textbooks and review articles.
Studies for the literature review were identified through MEDLINE searches of English language literature conducted between March and October 2002. These searches were supplemented by relevant articles known to the domain experts and reviewers through December 2003.
The MEDLINE literature searches were conducted to identify clinical studies published from 1966 through the search dates. The primary search was designed to capture studies pertaining to all topics. Supplemental searches were made to maximize retrieval of studies pertaining to specific topics, including: anxiety and hostility, carnitine, diet, hormone replacement therapy, pediatrics, and peripheral vascular disease. Development of the search strategies was an iterative process that included input from all members of the Work Group. The text words or MeSH headings for all topics included “renal replacement therapy,” end-stage renal disease and related terms. The searches were limited to studies on humans and published in English, and focused on either adults or children, as relevant.
MEDLINE search results were screened by members of the Evidence Review Team. Potential papers for retrieval were identified from printed abstracts and titles, based on study population, relevance to topics, and study size. For studies of risk factors and treatments, those with fewer than 10 subjects were excluded; for epidemiology studies, those with fewer than 30 subjects were excluded. Studies of risk factors had to evaluate a cardiovascular outcome to be included. Studies of risk factor or cardiovascular treatments, including surgery, had to be comparative; thus single-cohort case series were excluded. After retrieval, each paper was read to verify relevance and appropriateness for review, based primarily on study design and ascertainment of necessary variables. Some articles were relevant for two or more topics. Domain experts made the final decision for inclusion or exclusion of articles. All articles included were extracted and are contained in the summary tables. Numerous additional articles that did not meet the specific criteria necessary to qualify for inclusion were reviewed, with or without extraction, for use as background material.
In an iterative process, the topics for which articles would be analyzed in depth and summarized were restricted to those topics that had not been sufficiently summarized previously by other KDOQI Work Groups or others and provided evidence for the specific guidelines. For most topics, given the small number of available studies, all comparative studies with at least 10 dialysis patients per arm were included. For certain topics with relatively large numbers of studies, stricter criteria were used. For studies of serum calcium, phosphorus, and PTH as predictors of CVD, only studies that reported that they were sufficiently powered for these predictors were included. Studies that evaluated tobacco use as a risk factor for CVD had to both define smoking use categories a priori and have a minimum of 100 subjects. Studies of both Lp(a) and genetic markers were required to have at least 10 subjects with CVD outcomes. For predictors with sufficient numbers of studies, only associations with CVD event outcomes were included. These included: C-reactive protein, random serum troponin levels, smoking, echocardiogram measurements, and surgical interventions for coronary artery disease. Intermediate outcomes, including vascular calcification, intima-media thickness, and ventricular arrhythmia were included for other predictors analyzed. For certain predictors, studies were also included that reported prevalent (as opposed to future) CVD. These included genetic markers and ankle-arm brachial index.
Overall, 16,691 citations were screened (9,078 from the primary search; 7,613 from supplemental searches), from which 396 articles were retrieved and reviewed. An additional 151 articles, added by Work Group members and domain experts, were reviewed. Of these, a total of 86 articles met sufficient criteria to be included in summary tables.
Two types of evidence tables were prepared. Detailed tables contain data from each field of the components of the data extraction forms. These tables were used to efficiently track and transmit data about all extracted studies. They were completed by the Evidence Review Team from extraction forms filled out by Work Group members. They were then given to the Work Group members, but are not included in the report.
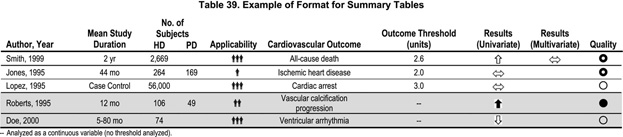
Summary tables describe the strength of evidence according to four dimensions: study size (of both HD and PD patients) and duration, study applicability, results and methodological quality. Within each table, the studies are first grouped by outcome type. Outcomes are ordered by all-cause death, CVD death, and CVD events. Studies with intermediate and prevalent outcomes are shaded at the bottom of the tables. Within each outcome, studies are ordered first by methodological quality (best to worst), then by applicability (most to least) and then by study size (largest to smallest). When relevant, outcome thresholds (e.g., of troponin I levels) or definitions of predictors (for genetic predictors) are included. Results are presented using summary symbols, as defined below. An example of an evidence table is shown in Table 39.
Study size and duration
The study (sample) size is used as a measure of the weight of the evidence. In general, large studies provide more precise estimates of prevalence and associations. In addition, large studies are more likely to be generalizable; however, large size alone does not guarantee applicability. A study that enrolled a large number of selected patients may be less generalizable than several smaller studies that included a broad spectrum of patient populations. Similarly, longer duration studies may be of better quality and more applicable, depending on other factors.
Applicability
Applicability (also known as generalizability or external validity) addresses the issue of whether the study population is sufficiently broad so that the results can be generalized to the population of interest at large. The study population is typically defined primarily by the inclusion and exclusion criteria. The target population was defined to include patients with end stage renal disease (primarily those on dialysis). A designation for applicability was assigned to each article, according to a three-level scale. In making this assessment, sociodemographic characteristics were considered, as were the stated causes of chronic kidney disease, and prior treatments. Applicability referred to either the HD population or the PD population, as appropriate.
Results
In general, the result is summarized by both the direction and strength of the association. Depending on the study type, the results may refer either to dichotomous outcomes, such as the presence of a specific genotype or a laboratory test above or below a threshold value, or to the association of continuous variables with outcomes, such as serum laboratory tests. The magnitude of the association and both the clinical and statistical significance of the associations were considered. Criteria for indicating the presence of an association varied among predictors depending on their clinical significance. Both univariate and multivariate associations are presented. Associations are generally represented according to the following symbols:
For studies of troponin I and T, sensitivity and specificity data are included when reported. For clarity, the results for studies of surgical interventions for coronary artery disease are presented as CABG, Stent, or Tissue to indicate studies for which the intervention had significantly better outcomes, or CABG for studies where there was a trend toward better outcomes with coronary artery bypass graft.
Quality
Methodological quality (or internal validity) refers to the design, conduct, and reporting of the clinical study. Because studies with a variety of types of design were evaluated, a three-level classification of study quality was devised:
Summarizing reviews and selected original articles
Work Group members had wide latitude in summarizing reviews and selected original articles for topics that were determined not to require a systemic review of the literature.
Format
This document contains 14 guidelines. The format for each guideline is outlined in Table 40. Each guideline contains one or more specific “guideline statements,” which are presented as “bullets” that represent recommendations to the target audience. Each guideline contains background information, which is generally sufficient to interpret the guideline. A discussion of the broad concepts that frame the guidelines is provided in the preceding section of this report. The rationale for each guideline contains a discussion of specific topics that support the guideline statements, together with a classification of the strength of evidence. The guideline concludes with a discussion of limitations of the evidence review and a brief discussion of implementation issues and research recommendations regarding the topic.
Strength of evidence
The overall guideline is, in general, graded according to the strength of evidence supporting the individual topics addressed by the guideline statements. Strength of evidence was assessed by assigning either “A,” “B,” or “C” (Table 41). An “A” rating indicates “it is strongly recommended that clinicians routinely follow the guideline for eligible patients. There is strong evidence that the practice improves health outcomes, and benefits substantially outweigh harms.” The “B” rating indicates “it is recommended that clinicians routinely follow the guideline for eligible patients. There is moderate evidence that the practice improves health outcomes.” A “C” rating indicates “it is recommended that clinicians consider following the guideline for eligible patients. This recommendation is based on either weak evidence, or on the opinions of the Work Group and reviewers, that the practice might improve health outcomes.”
The strength of evidence was graded using a rating system that takes into account: 1) methodological quality of the studies; 2) whether or not the study was carried out in the target population, i.e., patients with CKD on dialysis, or in other populations; and 3) whether the studies examined health outcomes directly, or examined surrogate measures for those outcomes, e.g., valve calcification instead of CVD death (Table 42). These three separate study characteristics were combined in rating the strength of a body of evidence provided by the composite of the pertinent studies.
In addition, the Work Group adopted a convention for using existing expert guidelines issued for populations other than the target population. Grades assigned by the guideline-issuing bodies for the strength of evidence were adopted. When the guideline or the evidence was not graded, this Work Group assumed that the guideline would be based on at least moderately strong evidence. The extrapolation of ungraded guideline recommendations from the general populations to the target population was considered to support grade B recommendations.
While the literature searches were intended to be comprehensive, they were not exhaustive. MEDLINE was the only database searched, and searches were limited to English language publications. Hand searches of journals were not performed, and review articles and textbook chapters were not systematically searched. However, important studies known to the domain experts that were missed by the literature search were included in the review.
Exhaustive literature searches were hampered by limitations in available time and resources that were judged appropriate for the task. The sensitive search strategies required to capture every article that may have had data on each of the questions frequently yielded upwards of 10,000 articles. Given the large number of topics, this approach was not feasible. The difficulty of finding all potentially relevant studies was compounded by the fact that in many studies, the information of interest for this report was a secondary finding for the original studies. We used our best judgment in developing search strategies to balance the yield of potentially useful articles and feasibility.