The following sections have been prepared to ensure that the state of the art and science related to CVD includes novel concepts, therapeutic strategies, and emerging areas of pathophysiological and practical importance to the care of dialysis patients.
The reader will notice that the format of this section is different, reflecting its different perspective: namely, the relative lack of evidence on which to base plausible guideline statements. The evidence that does exist, and is cited in this section, is either completely in nondialysis populations, or is purely associative information, with no intervention in any population yet tested. Thus, it would be a problem to include guideline statements or recommendations.
Nonetheless, this section describes the current status of knowledge with respect to risk factors and biomarkers, and represents an overview of key areas for future clinical trials. The reader is encouraged to review this section, and examine his or her current understanding and practice within the context of these highlights.
The literature review has been conducted using the same systematic strategy as for the previous guidelines in this document. The reviews presented here have been thoughtfully constructed so that clinicians can adopt different practices based on them. However, for reasons cited above, the ability to truly recommend or suggest changes in practice would be premature at this time.
Fatty acid biochemistry
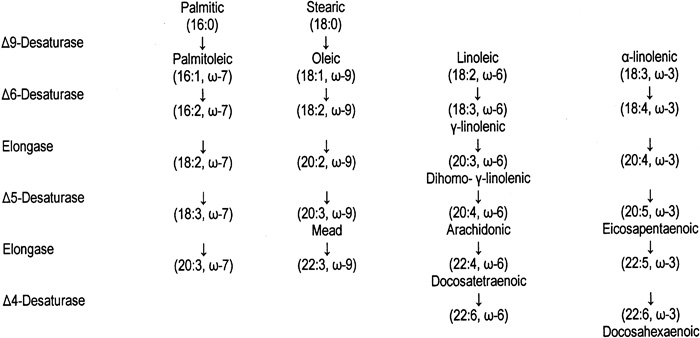
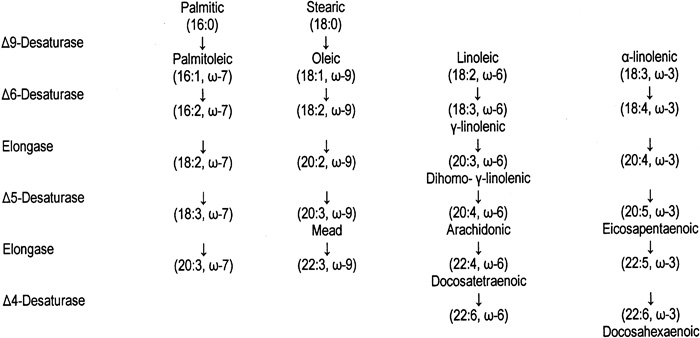
There are four families of polyunsaturated fatty acids in mammalian tissue: ω-3, ω-6, ω-7 and ω-9 (Fig 6). The fatty acids that are considered to be essential to human health belong to the first two families: 18:3, ω-3; 18:2, ω-6; and arachidonic acid (20:4, ω-6).505 The main dietary sources of ω-3 fatty acids are cold-water fish, canola oil, soybeans, walnuts, flaxseeds, and their products. Omega-6 fatty acids are found predominantly in all other vegetable oils and foods prepared with them, while ω-9 fatty acids are predominantly found in olives and olive oil.
Figure 6 - Desaturation and Elongation of the Major Families of Polyunsaturated Fatty Acids. Reproduced with permission.8
Inter-relationship between ω-3 fatty acid biochemistry and CVD
The beneficial effects of ω-3 fatty acids on CVD risk appear to be related to their impact on several risk factors identified to have a role in the development of CVD. These include: systemic inflammation, thrombotic tendency, lipid levels, endothelial function, reduction of proinflammatory responses, cardiac rhythm, and—to a lesser extent—hypertension.506–509 Mechanisms thought to be responsible for the beneficial effects of ω-3 fatty acids on CVD risk and treatment are listed in Table 25. The results from these studies have been analyzed and summarized for review elsewhere (1, 6, 7, 11, 12).506–508,510,511
The effect of ω-3 fatty acids on some of these risk factors has been demonstrated by partial substitution of ω-3 fatty acids for arachidonic acid in the sn-2 position of cell membrane phospholipids. The replacement of the ω-3 fatty acid eicosapentaenoic acid (20:5, ω-3) for the 20:4, ω-6 arachidonic fatty acid alters the proinflammatory thromboxane-prostanoid balance by attenuating the rate of dienoic eicosanoid production, results in a decrease in triglyceride levels, and confers antithrombotic and anti-inflammatory properties.505,509,512 Omega-3 fatty acids have been reported to decrease platelet activation, and improve vascular tone513 and endothelium-mediated vasodilation.511,514 Recent studies indicate that ω-3 fatty acids also impact the metabolism of adhesion molecules and cytokines (see Table 25).515,516
Hypotheses regarding the role of ω-3 fatty acids on decreasing sudden death and arrhythmias relate to inhibition of the fast, voltage-dependent sodium current and the L-type calcium channels, inhibition of thromboxane production, and beneficial effects on factors that affect heart-rate variability.517,518
Diet and risk reduction
The role of diet in risk reduction of CVD in the general population has been debated for over 100 years. Early animal studies demonstrated that diets high in cholesterol and saturated fat resulted in atherosclerosis. Human studies in the 1950s showed that diets high in cholesterol and saturated fatty acids increased serum cholesterol levels. Epidemiological data indicated that elevated serum cholesterol levels predicted the risk of CHD.507,509 As a result of these studies, initial dietary recommendations focused on lowering dietary cholesterol intake to 300 mg or less, decreasing saturated fatty acids to <10% of fat calories and total fat to <30% of total caloric intake.519 The application of these guidelines to the diet were accomplished by cutting back on animal fat intake, replacing butter with margarine, and using corn and other vegetable oils in food preparation and salads rather then partially hydrogenated fats and lard.
Advancing research over the years has now identified that CVD has many metabolic components, of which several are modifiable by dietary fatty acids. In addition to affecting serum lipid levels (Table 26),269 dietary fatty acids—specifically those of the ω-3 class—attenuate proinflammatory mediators and mechanisms that have been identified to have a role in the development of CVD.506,508,520
As a result of the growing abundance of literature including epidemiological and randomized clinical trials evaluating omega-3 fatty acids, the American Heart Association (AHA) and the Institute of Medicine (IOM) have recently included a recommendation for inclusion of ω-3 fatty acids in the diets of Americans for the purpose of prevention and treatment of cardiovascular disease.506,508 Prudent application of these new guidelines should be considered for the potential of prevention and treatment of CVD for the kidney patient on renal replacement therapy until data specific for this patient population become available.
While there is an abundance of literature on ω-3 fatty acids and kidney disease,521–530 no randomized clinical trials have been completed that evaluate the effectiveness of ω-3 fatty acids on CVD risk factors and surrogate markers in dialysis patients.
One recent study reports the effect of fish intake in dialysis patients.531 In a cohort of 216 incident dialysis patients, those who reported fish consumption were 50% less likely to die compared to those who did not report fish intake during the study interval (p=0.02). Multivariate analysis indicated that younger age, black race, and high mental health scores at baseline were also associated with a lower mortality risk. Omega-3 fatty acid substitution was not objectively documented in this study. Despite this limitation, the results suggest a beneficial effect of ω-3 fatty acids via fish consumption and further studies are warranted.
Fatty acid guidelines for general health maintenance
The IOM recently published Acceptable Macronutrient Distribution Ranges (AMDRs) that have been established for protein, carbohydrate, fat, ω-6 and ω-3 fatty acids.506 The AMDRs are based on the results of epidemiological studies and a literature review that evaluated associations between diet intake and risk of chronic disease. The AMDR for fat is 20%-35% of calories, 5–10% of calories for linoleic acid (ω-6 polyunsaturated fatty acids, PUFAs) and 0.6%-1.2% of energy for alpha-linolenic acid (ω-3 PUFAs). Up to 10% of the AMDR for ω-3 fatty acids can be consumed as eicosapentaenoic acid (EPA) and/or docosahexenoic acid (DHA); 0.06%-0.12% of energy. It is important to avoid excessive intake of ω-3 fatty acids as there have been reports of adverse effects on immune function and a potentially increased risk of excessive bleeding and hemorrhagic stroke.506 An intake of <3 g/day is unlikely to cause clinically significant bleeding.508
The IOM also has introduced a new reference value, Adequate Intake (AI), for the general population. It is defined as the recommended average daily intake level based on observed or experimentally determined approximations or estimates of nutrient intake by a group (or groups) of apparently healthy people that are assumed to be adequate. This value is used when the Recommended Dietary Allowance (RDA) cannot be determined.506
The AI for alpha-linolenic acid is 1.6 g and 1.1 g for men and women, respectively. Up to 10% can be consumed as EPA and/or DHA. This amount of ω-3 fatty acid can be obtained by eating at least two servings of fatty fish per week or by taking supplements. For linoleic acid, the AI is 17 g/day for adult men and 12 g/day for adult women. Table 27 identifies amounts of ω-3 fatty acids provided by selected food sources and supplements.
Overall approach
The AHA Guidelines for CVD prevention include encouraging the intake of fruits, vegetables, grains, low-fat or nonfat dairy products, fish, legumes, poultry, and lean meats. Food choices should be modified to reduce saturated fats (<10% of calories), cholesterol (<300 mg/dL) and trans-fatty acids by substituting grains and unsaturated fatty acids from fish, vegetables, legumes, and nuts. Salt intake should be limited to <6 g/day. Alcohol intake should also be limited (≤2 drinks per day in men and women) among those who drink.508
Response to therapy
Routine review of dietary intake and laboratory values should be sufficient to monitor tolerance to the inclusion of foods enriched in ω-3 fatty acid at least twice per week.
For patients with documented CHD, initial bimonthly check of bleeding times would be prudent, followed by monthly check with routine laboratory values once stable. Lipid levels, including triglycerides, should be monitored.
Patients taking 2–4 g of EPA+DHA supplements should maintain bimonthly checks of bleeding times with triglyceride monitoring as part of routine monthly laboratory values.
Follow-up
For those patients taking therapeutic doses of ω-3 fatty acids for hypertriglyceridemia, supplementation can be modified to a lower dose of 1 g/day upon normalization of the lipid profile and/or inclusion of foods enriched in ω-3 fatty acids 1–2 times per week.
There are more questions than answers regarding essential fatty acid metabolism, oxidative stress, CVD, and diet in the dialysis patient. The lack of evidence in the dialysis population makes extrapolation of guidelines for the general population to the dialysis patient questionable. However, the abundance of evidence suggesting a beneficial effect of ω-3 fatty acids, fresh fruits and vegetables, the ongoing data that saturated and trans-fatty acids are not heart-healthy, and the continued high prevalence of CVD morbidity and mortality in this patient population justifies prudent application of healthy eating guidelines until hard data for this patient population become available.
Incorporation of fruits, vegetables, grains, and nonfat dairy products can be problematic for many dialysis patients due to the need to restrict dietary potassium intake to (on average) 2 g/day. In addition, foods enriched in alpha-linolenic acid (flaxseed, walnuts, soy) are high in potassium, and contribute dietary protein and phosphorus (Table 28). Therefore, these foods are unlikely to be a reliable source of ω-3 fatty acids for the dialysis patient. Alternatively, the oils of these foods (walnut and flaxseeds) as well as canola oil can be safely incorporated into the diet for dialysis patients.
Studies are required to identify the essential fatty acid status of CKD patients, both progressive and for those on renal replacement therapy. Studies should also evaluate the interrelationships among ω-3 fatty acid supplementation, oxidative stress, CVD and dialysis therapy. Clinical trials are needed to evaluate the role of dietary fatty acid modification on CVD risk and outcomes in CKD patients on renal replacement therapy. Further clinical trials should evaluate current nutrition recommendations for the general population modified to the diet recommendations for CKD patients.
Based on the available evidence, it is beneficial for well-nourished, stable dialysis patients, who have no evidence of CVD, early CVD, or established CVD, to include food sources of ω-3 fatty acids in their diet at least twice weekly.