Patients with CKD and those on dialysis therapy are at risk of vitamin and mineral deficiencies as a result of abnormal renal metabolism, inadequate intake/poor gastrointestinal absorption, and dialysis-related losses. The provision of adequate quantities of these nutrients is essential because of their importance to growth and development in children.
6.1 The provision of dietary intake consisting of at least 100% of the DRI for thiamin (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5), pyridoxine (B6), biotin (B8), cobalamin (B12), ascorbic acid (C), retinol (A), a-tocopherol (E), vitamin K, folic acid, copper, and zinc should be considered for children with CKD stages 2 to 5 and 5D. (B)
6.2 It is suggested that supplementation of vitamins and trace elements be provided to children with CKD stages 2 to 5 if dietary intake alone does not meet 100% of the DRI or if clinical evidence of a deficiency, possibly confirmed by low blood levels of the vitamin or trace element, is present. (C)
6.3 It is suggested that children with CKD stage 5D receive a water-soluble vitamin supplement. (C)
6.1: The provision of a dietary intake consisting of at least 100% of the DRI for thiamin (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5 ), pyridoxine (B6), biotin (B8), cobalamin (B12 ), ascorbic acid (C), retinol (A), a-tocopherol (E), vitamin K, folic acid, copper, and zinc should be considered for children with CKD stages 2 to 5 and 5D. (B)
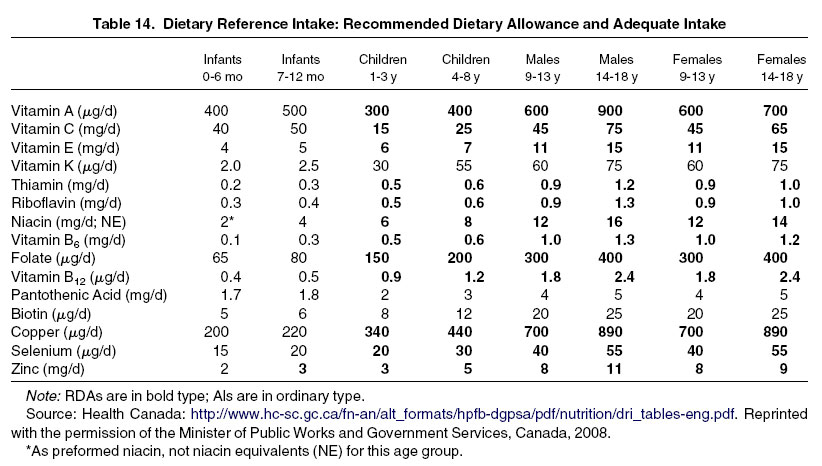
Little information exists about the vitamin and trace element needs specific to children with CKD and those on dialysis therapy. However, in view of the important role of these nutrients as cofactors in a number of metabolic reactions, and recognizing that achieving the DRI should reduce the risk of developing a condition that is associated with the nutrient in question that has a negative functional outcome,298,299 the practice has been to target 100% of the DRI as the goal for children with CKD stages 2 to 5 and on dialysis therapy (Table 14).
The B vitamins are essential for carbohydrate, protein, and fat metabolism; oxidation-reduction reactions; transamination and decarboxylation; glycolysis; and blood formation. Most thiamin in the body is present as thiamin pyrophosphate, which is a coenzyme for the oxidative decarboxylation of α-ketoacids. The metabolism of riboflavin resulting in functional flavoproteins is important because the flavoenzymes are important factors involved in oxidation-reduction reactions that are necessary for a variety of metabolic pathways, including energy production. Pantothenic acid is necessary for the synthesis of such compounds as fatty acids, cholesterol, and steroid hormones and for energy extraction during oxidation of amino acids. Pyridoxine is a coenzyme for nearly 100 enzymatic reactions and is essential for gluconeogenesis and niacin formation. Biotin has an important role in the metabolism of carbohydrates, fatty acids, and some amino acids. Finally, cobalamin has a key role in the metabolism of folic acid.
Ascorbic acid is involved in collagen synthesis through its role as a reversible reducing agent, whereas retinol is necessary for normal night vision. α-Tocopherol is the main antioxidant in biological membranes and vitamin K is a coenzyme for the posttranslational carboxylation of glutamate residues that ultimately influence the coagulation cascade. Folic acid is required for DNA synthesis, and copper functions as a cofactor in several physiologically important enzymes, such as lysyl oxidase, elastase, ceruloplasmin, and superoxide dismutase, as does zinc.
The DRIs were established by the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes of the Food and Nutrition Board, Institute of Medicine, National Academy of Sciences, as an expansion of the periodic RDA reports. Most studies examining vitamin status in children and adults with CKD occurred before the release of the DRI and hence report intake relative to the earlier RDA. The DRIs apply to the apparently healthy general population and are based on nutrient balance studies, biochemical measurement of tissue saturation or molecular function, and extrapolation from animal studies. Unfortunately, only limited data exist about the vitamin needs for infants and children, and there is no assurance that meeting the DRI will meet the needs of patients with kidney disease.
6.2: It is suggested that supplementation of vitamins and trace elements be provided to children with CKD stages 2 to 5 if dietary intake alone does not meet 100% of the DRI or if clinical evidence of a deficiency, possibly confirmed by low blood levels of the vitamin or trace element, is present. (C)
6.3: It is suggested that children with CKD stage 5D receive a water-soluble vitamin supplement. (C)
Children with CKD and those on dialysis therapy are at risk of alterations in vitamin and trace element levels or function as a result of decreased intake secondary to anorexia or dietary restrictions, increased degradation or clearance from blood, loss per dialysis, or interference with absorption, excretion, or metabolism (Tables 15 and 16).
Although limited, most data about the subject are derived from studies of adult populations. Whereas studies conducted in children receiving dialysis have documented dietary intake of most water-soluble vitamins, zinc, and copper that has been less than the RDA, the combination of dietary intake and supplemental intake has routinely met or exceeded the RDA.300-303 In large part, this is due to the rarity of a vitamin and mineral supplement specifically formulated for infants and children on dialysis therapy and the resultant need to use one of the proprietary renal supplements available.304-306 Caution should be exercised when using these supplements to not exceed the UL for the contents of the preparation when the intake of diet and supplement is combined (Tables 17 and 18). In older children and adolescents, daily vitamin supplementation is feasible without providing excessive vitamin intake. For smaller dosing in infants and toddlers, less frequent dosing (eg, every 2 to 3 days) or partial dosing (eg, half tablet) may be required if a liquid product or easily divisible tablet is not available. Children with healthy appetites for a variety of nutritious foods and children receiving the majority or all of their energy requirements from adult renal formulas generally meet 100% of the DRI for vitamins and trace elements and may not require vitamin supplementation.
Thiamin (vitamin B1)
Adult patients with CKD ingesting a low-protein diet have demonstrated borderline low thiamin levels.307 In 1 study of children receiving dialysis, the spontaneous dietary intake was below the RDA in 28 of 30 patients.301 Whereas a substantial quantity of thiamin is removed by HD, little appears to be lost by the peritoneal route in patients receiving chronic PD (CPD).308,309 In most cases, the combination of dietary intake and daily supplement to equal the DRI will prevent deficiency. Thiamin stores can be assessed indirectly by means of erythrocyte transketolase activity or directly by means of high-performance liquid chromatography (HPLC).310-312
Riboflavin (vitamin B2)A low-protein diet may contain inadequate quantities of riboflavin,312 and both Pereira et al301 and Kriley and Warady300 have documented spontaneous intake of riboflavin less than the RDA in children receiving dialysis. However, riboflavin deficiency is uncommon in patients being treated with HD or CPD and who receive a combined diet/supplement intake that meets or exceeds the DRI. Erythrocyte glutathione reductase activity is used to evaluate riboflavin status.312
Niacin (vitamin B3 )
There are limited data about the niacin status of patients with CKD, with or without the use of dialysis. The metabolic clearance of niacin is rapid, and thus it is believed that losses into dialysate are likely to be low. Prior studies have demonstrated the intake of niacin to be less than or equivalent to the RDA in patients prescribed a low-protein diet.314 Whereas Pereira et al301 found the spontaneous intake of niacin to be less than the RDA in 27 of 30 children receiving dialysis, the combined dietary and supplement intake exceeded the RDA in all cases. Thus, it is recommended that the DRI for niacin be provided per diet and/or supplement.
Pantothenic acid (vitamin B5)
There are few data available about the status of pantothenic acid in adult patients with CKD or those receiving dialysis, and no data are available for children. However, the vitamin is removed by HD, and normal, low, and high levels have been found in adult dialysis patients.315-317 Accordingly, patients on HD and CPD therapy likely should receive 100% of the DRI for this vitamin. Pantothenic acid levels are measured by means of radioimmunoassay.
Pyridoxine (vitamin B6)
Low pyridoxine intake has been documented in a number of adult surveys of dialysis patients. In children, low intake of pyridoxine in children with CKD was reported by Foreman et al.9 Stockberger et al318 found intake to be lower than 59% of the RDA in 67% of children receiving CPD, and Pereira et al301 noted intake less than the RDA in 26 of 30 pediatric dialysis patients. In a study of infants receiving CPD, Warady et al303 documented dietary pyridoxine intake of only 60% RDA. There are also a host of medicines that can interfere with pyridoxine (and folic acid) metabolism (Table 19).
Low blood levels (measured as plasma pyridoxal-5-phosphate by means of HPLC) have been documented in HD and CPD patients, and dialysis removal of the nutrient likely contributes to the deficiency. A daily pyridoxine-HCl supplement of 10 mg has been recommended for adult HD and CPD patients because this is the lowest dose that has been proved to correct pyridoxine deficiency. Lower supplemental doses, in addition to that provided by diet, likely would be sufficient in infants and young children based on the marked increase in blood level that has occurred with a 10-mg supplement in this population.300 Supplements that equate to the RDA have previously been recommended.302,319 Functional tests (eg, erythrocyte oxaloacetate transaminase) have been used to assess vitamin B6 deficiency. As noted, direct measurement of total pyridoxine by means of HPLC also can be performed.
Biotin (vitamin B8 )
The intake of biotin has been estimated to be less than the RDA in adult patients with CKD prescribed with a low-protein diet.316 In addition, intestinal absorption of biotin may be compromised in patients with CKD. The impact of HD on biotin status is poorly understood because both high and low blood levels have been reported.320,321 Although there is no information regarding the influence of CPD on biotin losses and there is no information at all from children with kidney disorders, intake equal to the DRI should be provided per diet and/or supplement. Plasma biotin is measured by using microbiological assays.
Folic acid (vitamin B9)
Litwin et al321a documented normal folic acid levels in 18 children with CKD and Pereira et al301 found the dietary intake of folic acid to be greater than the RDA in 21 of 30 pediatric dialysis patients. Low folic acid levels have been reported in adult patients receiving CPD, with an average dialysis loss of 107 μg/d in 1 study.322,323 Folic acid status (red blood cell and plasma) may be compromised by inhibitors of folic acid absorption (Table 19). Folic acid (along with vitamins B6 and B12) also has a key role in the handling of plasma homocysteine. Whereas some data have suggested that increased plasma homocysteine levels are a risk factor for CVD, other more recent studies have suggested otherwise.324,325 Studies conducted in children have all demonstrated lowering of the plasma homocysteine level (the normal plasma concentration of homocysteine is ~5 to 10 μmol/L) following the provision of folic acid.326-329 Thus, most children with CKD and those on dialysis therapy should receive the DRI, whereas adults are prescribed 1.0 mg/d.330,331 If lowering plasma homocysteine level is the clinical goal, children with increased plasma homocysteine levels pro-bably should receive 2.5 to 5.0 mg/d of folic acid.305,310-313,315,317 However, in dialysis patients, administration of folate and vitamins B6 and B12 has been reported to lower, but not normalize, plasma homocysteine levels.332,333 Red blood cell folate levels are most indicative of body stores.334 The reduced form of folic acid, tetrahydrofolate, may be measured by using a radioimmunologic technique.
Cobalamin (vitamin B12 )
Most adult and pediatric patients with CKD and dialysis patients have been reported to have normal cobalamin levels, regardless of whether they receive a supplement.300,303,309,322,323 Dietary intake also appears to meet or exceed the DRI in most, but not all, dialysis patients.300,301,303,335 Serum vitamin B12 levels can be determined by using radioassay methods.
Ascorbic acid (vitamin C)
Decreased vitamin C levels have been reported in patients with CKD, as well as those receiving HD and CPD.335-337 The low levels seen in dialysis patients are the result of low intake (eg, restricted intake of fruits) and dialysis losses.301,322,335-337 In children, Pereira et al301 found that 24 of 30 children received less than the RDA by diet alone. Warady et al303 reported a negative mass transfer of 32 mg/d in children receiving APD, an amount compensated for by oral supplementation. However, in a study of infants receiving APD, Warady et al303 reported dietary intake to be 140% of RDA, increasing to 180% of RDA with the addition of a 15-mg/d supplement. Excessive vitamin C intake (eg, 0.5 to 1 g/d in adults) can result in increased oxalate concentrations in plasma and soft tissues.338,339 Thus, recommended combined dietary and supplement intake should not greatly exceed the DRI, with caution exercised when providing supplementation. Plasma ascorbic acid levels reflect dietary intake, and leukocytes levels estimate the body pool.
Retinol (vitamin A)
Vitamin A is not removed by dialysis, and elevated serum levels are present in patients with CKD and on dialysis therapy without supplementation.300,302,303,309 Whereas retinol-binding protein (the transport protein for vitamin A) is catabolized in the renal tubules in individuals with normal kidney function, both vitamin A and retinol-binding protein accumulate when the GFR is reduced and there is impaired renal tubular activity.340,341 Kriley and Warady300 documented serum vitamin A levels in pediatric dialysis patients without supplements that were 3-fold greater than control patients. Because the risk of developing vitamin A toxicity is high when supplements with vitamin A are provided, total intake of vitamin A should be limited to the DRI, with supplementation rarely recommended and limited to those with very low dietary intake. Plasma vitamin A levels are measured by means of HPLC.
Vitamin K
There is no need for an intake of vitamin K greater than the DRI unless the patient is eating poorly and receiving long-term antibiotic therapy.309,342,343 Plasma vitamin K levels are measured by means of liquid chromatography.
a-Tocopherol (vitamin E)
Plasma vitamin E levels in patients receiving HD have been reported as low, normal, and high.344-346 No differences in levels were found comparing predialysis and postdialysis samples, and no α-tocopherol was found in dialysis effluent.347,348 Studies of CPD patients have also reported both low and high levels of α-tocopherol.335,349,350 Nevertheless, because of its ability to alleviate oxidative stress in patients at risk of CVD, patients with CKD and dialysis patients (aged < 9 years) should receive the DRI of vitamin E.351,352 Serum vitamin E levels are measured by means of HPLC.
Copper
Dietary intake less than the DRI has been noted for copper in children receiving CPD.353 Although copper excess is associated most commonly with CKD, low serum copper and ceruloplasmin levels also have been reported in children receiving HD.303 Intake should be monitored every 4 to 6 months because supplementation to the DRI may be required in patients with particularly low dietary intake. Assessment of serum copper levels may be beneficial when clinical signs of overload or deficiency are present.
Selenium
Although selenium is normally excreted by the kidney and not removed by dialysis, low serum levels occur in patients with CKD or those receiving maintenance HD.337,354 The selenium content of food is dependent on the selenium content of soil on which crops have grown or animals have grazed.309 Selenium-dependent glutathione peroxidase activity in the blood, an integral component of the antioxidant defense, has also been found to be lower in patients with CKD than in healthy subjects, and the reduction worsens with increasing severity of disease. Supplementation of selenium in patients with CKD has resulted in a minimal increase in selenium-dependent glutathione peroxidase activity in patients with CKD, but not dialysis patients. Whereas routine supplementation is not recommended, patients should receive a daily dietary intake that meets the DRI.
Zinc
Low serum zinc levels result from removal by dialysis and poor intake. Intake less than the RDA has been documented in children receiving CPD.353 Children and adults should receive the DRI for zinc, with supplementation reserved for treatment of clinical manifestations of zinc deficiency after laboratory confirmation.
The absence of studies in children with CKD and those on dialysis therapy that have assessed vitamin and trace element blood levels (1) before the institution of supplementation or after a washout period, and (2) after supplementation in a randomized manner with a control group for comparison. In addition, of the limited number of studies on the topic, most address dialysis and not predialysis patients with CKD, and all are based on single-center populations.