Fluid and electrolyte requirements of individual children vary according to their primary kidney disease, degree of residual kidney function, and method of kidney replacement therapy. Supplementation or restriction of fluid, sodium, and potassium intake is individualized and influenced by the volume of urine output and the ability to concentrate urine, hydration status, and the presence or absence of hypertension or hyperkalemia. Dietary and other therapeutic lifestyle modifications are recommended as part of a comprehensive strategy to lower blood pressure and reduce CVD risk in those with CKD.444
8.1 Supplemental free water and sodium supplements should be considered for children with CKD stages 2 to 5 and 5D and polyuria to avoid chronic intravascular depletion and to promote optimal growth. (B)
8.2 Sodium supplements should be considered for all infants with CKD stage 5D on peritoneal dialysis (PD) therapy. (B)
8.3 Restriction of sodium intake should be considered for children with CKD stages 2 to 5 and 5D who have hypertension (systolic and/or diastolic blood pressure ≥ 95th percentile) or prehypertension (systolic and/or diastolic blood pressure ≥ 90th percentile and < 95th percentile). (B)
8.4 Fluid intake should be restricted in children with CKD stages 3 to 5 and 5D who are oligoanuric to prevent the complications of fluid overload. (A)
8.5 Potassium intake should be limited for children with CKD stages 2 to 5 and 5D who have or are at risk of hyperkalemia. (A)
8.1: Supplemental free water and sodium supplements should be considered for children with CKD stages 2 to 5 and 5D and polyuria to avoid chronic intravascular depletion and to promote optimal growth. (B)
The primary cause of CKD needs to be considered when initiating dietary modification of fluids and sodium. Although restriction of sodium and/or fluids is appropriate in children with CKD associated with sodium and water retention, the most common causes of CKD in children are associated with excessive loss of sodium and chloride. Infants and children with obstructive uropathy or renal dysplasia have polyuria, polydypsia, and difficulty conserving sodium chloride. These children develop a salt-wasting state and require salt supplementation.119 In addition to its effect on extracellular volume, sodium depletion also adversely affects growth and nitrogen retention.445 Sodium intake supports normal expansion of the ECF volume needed for muscle development and mineralization of bone.446 Therefore, infants and children with polyuric salt-wasting forms of CKD who do not have their sodium and water losses corrected may experience vomiting, constipation, and significant growth retardation associated with chronic intravascular volume depletion and a negative sodium balance.111 It is important to note that normal serum sodium levels do not rule out sodium depletion and the need for supplementation.
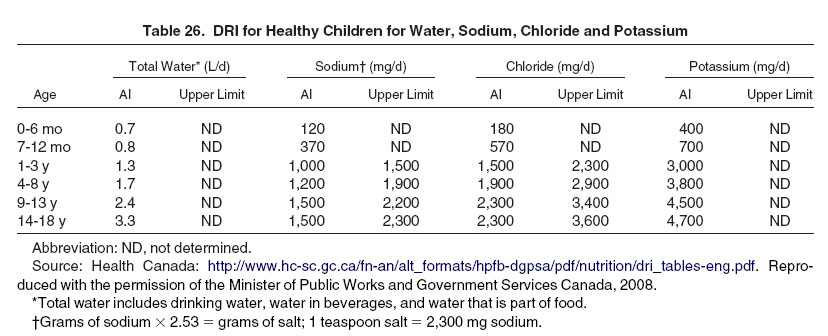
Individualized therapy can be accomplished by first prescribing at least the age-related DRI of sodium and chloride (Table 26).119 In 2 small cohort studies, infants with polyuric salt-wasting CKD stages 3 to 5 who were given nutritional support with generous fluids and sodium supplements achieved better growth compared with published data for nonsupplemented infants with CKD. The dosage of sodium supplements used by the 2 studies varied between 2 to 4 mmol of sodium (Na)/100 mL formula added to 180 to 240 mL/kg/d of formula111 and 1 to 5 mmol Na/kg body weight/d120 and was adjusted according to blood biochemistry test results. The average dose used in the first study was Na, 3.2 ± 1.04 mmol/kg.111 Nasogastric or gastrostomy tube feedings were used111 or suggested for critical periods.120
Sodium given as alkali therapy should be considered as part of the daily sodium allowance.119
Home preparation of sodium chloride supplements using table salt generally is not recommended due to potential errors in formulation that could result in hypo- or hypernatremia.447
8.2: Sodium supplements should be considered for all infants with CKD stage 5D on PD therapy. (B)
Infants on PD therapy are predisposed to substantial sodium losses, even when anuric. High ultrafiltration requirements per kilogram of body weight result in removal of significant amounts of sodium chloride. These losses cannot be replaced through the low sodium content of breast milk (160 mg/L or 7 mmol/L) or standard commercial infant formulas (160 to 185 mg/L or 7 to 8 mmol/L).449 Consequences of hyponatremia include cerebral edema and blindness; therefore, neutral sodium balance must be maintained. Therapy should be individualized based on clinical symptoms, including hypotension, hyponatremia, and/or abnormal serum chloride levels. Sodium balance measurements, determined from dietary and medication intake and dialysate effluent losses, should be considered every 6 months concurrent with the measurement of dialysis adequacy. More frequent measurement is indicated after significant changes to the dialysis prescription or clinical status.
8.3: Restriction of sodium intake should be considered for children with CKD stages 2 to 5 and 5D who have hypertension (systolic and/or diastolic blood pressure ≥ 95th percentile) or prehypertension (systolic and/or diastolic blood pressure ≥ 90th percentile and < 95th percentile). (B)
When kidney function is impaired, ECF volume increases, edema occurs, and blood pressure increases. Hypertension is already common in the early stages of CKD, with 48% to 63% of children affected.444,450 More than 50% of children on dialysis therapy have uncontrolled hypertension,450,451 and an additional 20% have controlled hypertension.63,451-454 Children with severe hypertension are at increased risk of hypertensive encephalopathy, seizures, cerebrovascular events, and congestive heart failure.455 Less severe hypertension can contribute to progression of CKD. Therefore, dietary modification is encouraged for children and adolescents who have blood pressures in the prehypertensive range, as well as those with hypertension.455
A systematic review of pediatric clinical trials demonstrated that modest dietary sodium restriction reduces blood pressure in hypertensive children without CKD.456 In dialysis patients, many observational and interventional studies of patients with CKD have shown that restricting sodium intake is an essential tool for volume and blood pressure control.457-459 Aside from preventing acute complications of hypertension, optimal control of blood pressure reduces further kidney damage and modifies progression of disease.
The K/DOQI Clinical Guidelines for Hypertension,444 CVD,220 and Dialysis Adequacy63 are all in agreement that dietary sodium restriction is an important component of a comprehensive strategy for volume and blood pressure control in adults and children with CKD. The earliest recommendation from the Hypertension Guidelines was to limit daily sodium intake to less than 2,400 mg (<104 mmol).444 The more recent Cardiovascular and Adequacy Guidelines have lowered the recommendation to less than 2,000 mg (<87 mmol) of sodium per day.450,459 The most recent 2005 Dietary Guidelines for Americans older than 2 years460 recommend that individuals with hypertension, blacks, and middle-aged and older adults aim to consume no more than 1,500 mg (65 mmol) of sodium per day. To provide more size-appropriate guidelines for infants and young children, based on a standard 60- to 70-kg adult, 1,500 to 2,400 mg/d of sodium would be the equivalent of sodium, 1 to 2 mmol/kg/d. This degree of restriction is reasonably consistent with the age-appropriate DRI for healthy children (Table 26).
The average daily intake of sodium in healthy children is far above recommended levels. In a national community health survey, 77% of children aged 1 to 3 years exceeded the recommended upper limit for sodium (1,500 mg/d), with a mean intake of 1,918 mg/d.461 In children 4 to 8 years old, daily intake averaged 2,700 mg and 93% had consumed more than the recommended upper limit. For most of these children, adding salt at the table did not contribute to their high sodium intakes because 69% of those aged 1 to 3 years and 52% of those aged 4 to 8 years "never" added salt to their food. Salt intakes of adolescents exceeded recommended upper limits by 27% to 79%; the intake of males was significantly higher than that of females.
Sodium occurring naturally in food accounts for only about 10% of total intake, whereas salt added at the table or while cooking provides another 5% to 10% of total intake.462 The majority (75%) of sodium in the diet comes from salt added by manufacturers during processing 462 to enhance flavor, control the growth of bacteria, provide certain functional characteristics, or act as a preservative. By weight, salt is composed of 40% sodium and 60% chloride. One teaspoon of salt contains about 2,300 mg of sodium.
Reduction of sodium intake can be achieved by replacing processed and canned foods with fresh foods; reading food labels to identify less salty foods; reducing salt added to foods at the table; in cooking, substituting fresh herbs and spices to flavor foods; and eating fast foods less often. The nutrition facts panel on food labels lists sodium content as actual amount (mg) and percent of the recommended daily value (% DV). Foods containing less than 140 mg or 5% DV are considered low in sodium,460 and foods that have no more than 170 to 280 mg of sodium or 6% to 10% of the DV for sodium should be chosen. Salt substitutes, also referred to as light salts, typically replace all or some of the sodium with another mineral. Salt substitutes replacing Na chloride (NaCl) with potassium chloride (KCl) are contraindicated in children with hyperkalemia.
Certain medications (eg, antacids, laxatives, and nonsteroidal anti-inflammatory drugs) can be a significant source of sodium. Kayexalate® (sodium polystyrene sulfonate) contains 100 mg (4.3 mmol) of sodium per 100 g of powder. Where available, non–sodium-containing potassium binders (eg, calcium polystyrene sulfonate) should be used for children with severe hypertension and hyperkalemia.
Restriction of salt and fluid intake requires considerable patient motivation, which is often a problem in the adolescent population. The K/DOQI Hypertension Guidelines recommend dietary education by a dietitian every 3 months.444 Patients used to a high-sodium intake may lose their appetite and become malnourished if sodium restriction is instituted too abruptly and too strictly.63 In these patients, sodium restriction should be introduced gradually to provide time for taste adjustment. By cutting back gradually, most patients find that they do not miss the salt.
8.4: Fluid intake should be restricted in children with CKD stages 3 to 5 and 5D who are oligoanuric to prevent the complications of fluid overload. (A)
Children with oliguria or anuria need to limit their fluid intake to avoid associated complications of altered fluid status, including hypertension. Fluid restriction for oligoanuric children on HD therapy is also indicated, and an interdialytic increase above their "dry" weight (≤5% of their dry weight) is expected and desirable. Severe restriction of food (and fluid) intake by children for the purpose of avoiding extra HD sessions fosters malnutrition and should be discouraged.
Daily fluid restriction = insensible fluid losses (Table 27) + urine output + amount to replace additional losses (eg, vomiting, diarrhea, enterostomy output) − amount to be deficited.
To restrict fluid intake, children should be advised to reduce their intake of beverages, as well as foods that are liquid or semiliquid at room temperature (eg, ice, soup, Jell-O, ice cream, yogurt, pudding, and gravy). This can be achieved by drinking only when thirsty, taking small amounts throughout the day using small cups or glasses, quenching thirst by sucking on crushed ice, eating cold fruit, chewing gum, gargling or using breath sprays/sheets, and avoiding high-sodium or very sweet foods. About 80% of an individual's total water intake comes from drinking water and beverages and the other 20% is derived from food.448 Many fruits and vegetables contain lots of water and can inconspicuously add to a child's fluid intake. These foods are not restricted routinely. The free water content of infant formulas (~90% by volume) and enteral feedings (70% to 85%) should be considered when formulating feeding regimens for fluid-restricted children (see Appendix 3, Table 36).
Attempts at fluid restriction may be futile if sodium is not restricted at the same time.63 Reducing fluid intake alone is not practical most of the time because the increased ECF osmolality brought about by the excessive sodium ingestion will stimulate thirst, followed by further fluid ingestion and isotonic fluid gain.63,463,464
8.5: Potassium intake should be limited for children with CKD stages 2 to 5 and 5D who have or are at risk of hyperkalemia. (A)
Ninety-eight percent of the body's potassium is contained in cells, whereas only 2% is in the extracellular compartment. Potassium moves rapidly between the intra- and extracellular compartments to maintain normal serum levels. Because of the uneven distribution between compartments, small shifts can result in major changes in serum potassium concentrations. Maintaining a normal serum potassium concentration depends on these shifts, as well as excretion of potassium from the body. Intestinal excretion accounts for approximately 10% of potassium excretion, whereas the remainder is excreted in urine. Renal potassium excretion typically is maintained until GFR decreases to less than 10 to 15 mL/min/1.73 m2. The risk of hyperkalemia is also increased by urinary obstruction, rhabdomyolysis, hemolysis (eg, blood transfusions and tumor lysis), acidosis, or treatment with potassium-sparing diuretics, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers.
Extracellular potassium influences muscle activity, especially the heart. Both hypokalemia and hyperkalemia cause alterations in all muscle function (skeletal, myocardial, and smooth muscle contractility) and cardiac arrhythmias. Hyperkalemia is common in patients with CKD stage 5 and, when severe, can rapidly lead to death from cardiac arrest or paralysis of muscles that control ventilation. Therefore, control of serum potassium is a critically important part of dietary management in patients with CKD.
When the kidney loses its ability to filter potassium (K), counseling children and caretakers to limit dietary potassium is critical to prevent and manage hyperkalemia. There are no data for the degree of dietary potassium restriction required for children with hyperkalemia. Suggested dietary management of hyperkalemia in adults limits intake to less than 2,000 to 3,000 mg (<50 to 75 mmol/d) of K daily.444,465,466 Based on a 70-kg standard adult, this is the equivalent of less than 30 to 40 mg/kg/d (<0.8 to 1 mmol/kg/d). For infants and young children, 40 to 120 mg (1 to 3 mmol/kg/d) of K may be a reasonable place to start. Breast milk (mature) has the lowest potassium content (546 mg/L; 14 mmol/L) compared with standard commercial cow's milk-based infant formulas (700 to 740 mg/L; 18 to 19 mmol/L). Volumes of infant formula of 165 mL/kg or greater will exceed 120 mg (3 mmol) K/kg and may aggravate hyperkalemia. Children can lower potassium intake by restricting intake of such high-potassium foods as bananas, oranges, potatoes and potato chips, tomato products, legumes and lentils, yogurt, and chocolate.460 The nutrition facts panel on food labels is not required to list potassium, but may provide potassium content as actual amount (mg) and % DV. Foods containing less than 100 mg or less than 3% DV are considered low in potassium. Foods containing 200 to 250 mg or greater than 6% DV are considered high in potassium.467 If potassium is not listed, it does not mean that the food does not contain potassium. Presoaking root vegetables, including potatoes, effectively lowers potassium content by 50% to 75%.468,469
Salt substitutes, also referred to as light salts, typically replace all or some of the sodium with another mineral, such as potassium or magnesium. Salt substitutes that contain potassium may cause hyperkalemia with life-threatening consequences in individuals with hyperkalemia or a tendency toward it.470 Potassium-containing salt substitutes are inappropriate for people who need to limit both salt and potassium.
When hyperkalemia persists, despite strict adherence to dietary potassium restriction, nondietary causes of hyperkalemia—such as spurious values, hemolysis, metabolic acidosis, other exogenous potassium sources, constipation, inadequate dialysis, medications (angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, nonsteroidal anti-inflammatory agents, and potassium-sparing diuretics), and tissue destruction due to catabolism, infection, surgery, or chemotherapy—should be investigated further.471,472
Moderate to severe hyperkalemia may require treatment with a potassium binder. When oral, enteral, or rectal administration of potassium-binding resins is ineffective, undesirable, or not feasible, infant formula, enteral feedings, or other fluids can be pretreated to safely and effectively reduce their potassium content. Depending on the dosage of potassium binder used, this process lowers the potassium content of the feeding by 12% to 78%.473-477 This process also may be indicated when there are concerns about obstruction of an enteral feeding tube. In addition to reducing potassium content, other reported changes associated with binder use include an increase or reduction in other nutrients, such as sodium and calcium.
Children on PD or frequent HD therapy (ie, >5 sessions/wk) rarely need dietary potassium restriction and may actually develop hypokalemia. Normokalemia may be achieved through counseling and frequent reinforcement of a high-potassium diet,478 KCl supplements, or addition of potassium to the dialysate.
This guideline is in agreement with the following CARI CKD Guidelines479:
This guideline did not agree with the following suggestion in the CARI CKD Guidelines:
No clinical guidelines were found for the degree of potassium restriction for children with or at risk of hyperkalemia. The CARI Guidelines for adults recommend a reduced potassium diet that limits intake to approximately 50 to 65 mmol (2,000 to 2,500 mg) of potassium daily.480 The European Best Practice Guidelines on Nutrition for adults recommend a daily potassium intake of 50 to 70 mmol (1,950 to 2,730 mg) potassium daily or 1 mmol/kg ideal body weight for hyperkalemic predialysis patients.309
There are no studies examining the effects of various levels of fluid, sodium, or potassium restriction on outcomes in children with CKD.