17.1 Serum levels of calcium, phosphorus, total CO2 and PTH should be monitored following kidney transplantation. (OPINION)
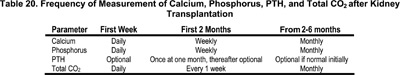
17.1.a The frequency of these measurements should be at least as often as shown in Table 20. (OPINION)
17.1.b Six months after transplantation, the frequency of measurements should follow the recommendations of Table 2, Guideline 1, depending on the stage of CKD.
17.2 The care of osteodystrophy in kidney transplant patients reaching CKD Stage 2 and below should follow the guidelines established for native CKD. (OPINION)
17.3 Kidney transplant recipients who develop persistent hypophosphatemia (below the age-appropriate lower limits) should be treated with phosphate supplementation. (OPINION)
17.4 To minimize bone mass loss and osteonecrosis, the lowest effective dose of glucocorticoids should be used. (OPINION)
Successful renal transplantation corrects many of the underlying abnormalities contributing to bone disease in children with CKD. However, hypophosphatemia, pre-existing hyperparathyroidism, and glucocorticoid therapy may impair healing of renal bone disease and lead to bone loss. In addition, progressive damage to the transplanted kidney will result in CKD and bone and mineral disorders comparable to the effects of CKD in the native kidney. Therefore, the kidney transplant recipient is at risk for multifactorial, progressive bone disease.
Hypophosphatemia
Hypophosphatemia is a frequent, early complication of renal transplantation. The primary cause is increased urinary phosphate loss and persistent hyperparathyroidism.543 A recent series in adults demonstrated that as many as 93% of patients develop moderate to severe hypophosphatemia (serum phosphate concentration 0.9-2.25 mg/dL), an average of 5 weeks following transplantation.544 In the setting of good allograft function, gradual decreases in serum PTH and improvements in allograft tubular function result in normalization of serum phosphate concentrations within months. Hypophosphatemia may persist as a late complication in patients with prolonged hyperparathyroidism.188 Numerous adult studies have demonstrated incomplete resolution of hyperparathyroidism and persistently increased bone turnover in long-term recipients with good renal function.545,546
Corticosteroid-Induced Osteopenia
The pathogenesis of corticosteroid-induced bone loss is multifactorial and has been reviewed extensively in the adult literature.547 The primary mechanism of glucocorticoid-induced osteopenia is decreased bone formation by osteoblasts due to a decreased work rate and a decreased active life span of osteoblasts. Animal data from a rat model suggest that cyclosporine may induce a high-turnover osteopenia with loss of trabecular bone,548 potentially compounding the bone toxicities of glucocorticoid therapy and hyperparathyroidism. It is well-recognized that corticosteroids result in rapid loss of trabecular bone in adults; however, the effects of corticosteroids, cyclosporin A and tacrolimus on trabecular and cortical bone mineral accretion during growth are not known.
Hypophosphatemia
Severe hypophosphatemia may result in hemolytic anemia, impaired cardiac contractility and respiratory insufficiency. Therefore, it is common practice to supplement with oral phosphate salts in patients with severe hypophosphatemia. In adults, a preliminary study assessed phosphate replacement for moderate hypophosphatemia in the early post-transplant period, and the impact on serum calcium, PTH, and acid/base metabolism. Oral supplementation with neutral sodium phosphate (Na2HPO4) effectively corrected hypophosphatemia, increased muscular ATP and phosphodiester content, and improved renal acid excretion without any adverse effect on serum PTH levels.
CKD in the Transplanted Kidney
There are no available data on the clinical sequelae of bone disease in children with progressive CKD due to allograft failure in the setting of renal transplantation. However, progressive CKD in the allograft will likely set in motion the same pathophysiological abnormalities observed with CKD in the native kidney. In addition, the combination of glucocorticoid-induced suppression of bone formation and hyperparathyroid-induced increases in bone resorption result in uncoupling of bone. This likely has particularly devastating effects on bone modeling and bone mineral accrual during growth. Glucocorticoids may impair gastrointestinal calcium absorption, resulting in negative calcium balance and exacerbating 2° HPT. Therefore, the child with progressive CKD and a kidney transplant requires ongoing assessment and treatment of serum calcium, phosphorus, PTH, serum bicarbonate and 25(OH)D concentrations, consistent with the guidelines for CKD in the native kidney.
Hypophosphatemia
We are unaware of any investigations examining the incidence of hypophosphatemia in the weeks immediately following transplantation in children. One study recently described a series of 16 children evaluated at 3, 6, and 12 months following transplantation. Serum phosphate concentrations were not decreased at these intervals.549 The median serum phosphate concentration at 3 months was 3.99 mg/dL, range 3.16-5.54 mg/dL.
Impaired Bone Mineralization Following Transplantation in Children
While there are numerous DXA studies of bone following transplantation in children, only one included bone histomorphometry.372 This study evaluated 47 children and adolescents with stable renal function an average of 3.2 years after transplantation.372 Eleven of 47 children had PTH values >65 pg/mL and four exceeded 100 pg/mL. Bone biopsies revealed that 31 transplant recipients had normal bone formation, 11 had mild hyperparathyroidism, and five had adynamic skeletal lesions. Neither the interval since transplantation, serum PTH, serum creatinine, nor the cumulative prednisone doses differed according to histological subgroups. Despite normal bone formation rates (BFRs) in many children, all three subgroups demonstrated increased eroded bone perimeter, increased osteoid area, and increased osteoid perimeter. Hyperparathyroidism improved or resolved after transplantation in all 14 subjects with high-turnover bone disease prior to transplantation; however, one patient developed an adynamic lesion following transplantation. Bone histology did not change following transplantation among those with normal bone formation prior to transplantation. Bone formation improved in two of the three children with adynamic bone disease prior to transplantation. In summary, most—but not all—skeletal lesions improve substantially in pediatric patients undergoing successful transplantation; however, concern is raised over residual hyperparathyroidism or development of adynamic bone disease in a few.
Studies of bone using DXA in children following transplantation have yielded conflicting results, largely related to the difficulties in interpreting DXA results in children with delayed growth and development.35,372,549-551 One study first described bone loss in children following renal transplantation.552 Bone mineral content (BMC) z-scores were less than -2.0 in 11 of 18 (62%) children. Children receiving daily steroid demonstrated significantly greater bone loss than children on alternate-day steroid treatment. A subsequent longitudinal study of DXA measures of whole body BMC following renal transplantation in 16 children showed that BMC decreased from the initial z-score of 0.98 to a z-score of -0.55 three months after transplant.549 A further decrease was noted at the end of month 6 (-1.34 SD) and month 12 (-1.32 SD). These studies related bone mineralization to chronologic age. Others have investigated the possible influence of height and weight retardation on the measurement of BMD in pediatric transplantation recipients.35 Only one patient had low values for vertebral BMD when the data were corrected for height or weight. The authors concluded that BMD among pediatric renal transplantation recipients is not diminished when the data are corrected for height or weight, rather than age. Another study reported similar results372: BMD z-scores for age were significantly decreased (-0.67 ± 1.2); however, BMD z-scores for height were above normal in all three histological subgroups (0.68 ± 1.0). This may be a misleading approach since shorter controls will be less mature than the patients with CKD. With the exception of a case series of fractures in children with cystinosis,553 there are no data on fractures following transplantation in children.
Corticosteroid-Induced Osteopenia
There are currently no data available addressing the impact of different corticosteroid doses or formulations on bone mineral accretion in children with a kidney transplant. None of the DXA studies reviewed above demonstrated a consistent relationship between glucocorticoid therapy and bone mass. However, glucocorticoid therapy is a major factor in the development of osteopenia in adult transplantation recipients, as reviewed in the adult guidelines. Therefore, it is recommended that clinicians use the lowest effective dose of corticosteroids necessary to preserve renal function.
Prior studies have suggested that calcium and active vitamin D therapy may lessen corticosteroid-induced bone loss in non-transplant patients.554,555 A recent randomized clinical trial in 111 adult renal transplant recipients demonstrated that low-dose (0.25 µg/day) 1-α-hydroxyvitamin D plus calcium (1,000 mg/day) partially prevented the bone loss at the lumbar spine and proximal femur during the first six months following renal transplantation.556 There are no data in children.
Bisphosphonate Therapy
The effects of bisphosphonate therapy on skeletal modeling and bone mineral accretion have not been adequately addressed in children with CKD. There are no data assessing the safety and efficacy of these drugs in children with CKD or glucocorticoid-induced osteoporosis.
As outlined above, DXA studies of bone in children following transplantation have yielded conflicting results, largely related to the difficulties in interpreting DXA results in children with delayed growth and development. Furthermore, there are no data assessing the prevalence and timing of hypophosphatemia in the immediate post-transplant interval, risk factors for hypophosphatemia in children, or the efficacy of phosphate supplementation. Finally, there are no controlled studies, either clinical trials or controlled observational studies, examining bone disease in the pediatric renal transplant recipient.
Bone disease may not regress completely in children following successful kidney transplantation. Future research is needed to address the following issues: