11.1 To prevent aluminum toxicity, the regular administration of aluminum should be avoided and the dialysate concentration of aluminum should be maintained at <10 µg/L. (EVIDENCE)
11.1a CKD patients ingesting aluminum should not receive citrate salts simultaneously. (EVIDENCE)
11.2 To assess aluminum exposure and the risk of aluminum toxicity, serum aluminum levels should be measured at least yearly and every 3 months in those receiving aluminum-containing medications. (OPINION)
11.2a Baseline levels of serum aluminum should be <20 µg/L. (OPINION)
11.3 A deferoxamine (DFO) test should be performed if there are elevated serum aluminum levels (60 to 200 µg/L); clinical signs and symptoms of aluminum toxicity (Table 31), or prior to parathyroid surgery if the patient has had aluminum exposure. (EVIDENCE) (Algorithms 6 and 7)
11.3a The test is done by infusing 5 mg/kg of DFO during the last hour of the dialysis session with a serum aluminum measured before DFO infusion and 2 days later, before the next dialysis session. (OPINION)
11.3b The test is considered positive if the increment of serum aluminum is ≥50 µg/L. (OPINION)
11.3c A DFO test should not be performed if the serum levels of aluminum are >200 µg/L to avoid DFO-induced neurotoxicity. (OPINION)
11.4 The presence of aluminum bone disease can be predicted by a rise in serum aluminum of ≥50 µg/L following DFO challenge combined with plasma levels of intact PTH of <150 pg/mL (16.5 pmol/L). (OPINION) However, the gold standard for the diagnosis of aluminum bone disease is a bone biopsy showing increased aluminum staining of the bone surface (>15% to 25%) using aluminum stain and often adynamic bone or osteomalacia. (EVIDENCE)
Aluminum is widely present in nature, but most aluminum salts are quite insoluble. Moreover, only a tiny fraction of ingested aluminum is absorbed; this small amount is normally excreted by the kidney so that the body burden of aluminum does not increase. When there is a markedly reduced or absent kidney function, there is little or no ability to excrete aluminum and it can accumulate slowly. When aluminum is present in dialysate, it enters the body directly across the dialysis membrane, and the type of syndrome that develops depends on the rapidity and magnitude of aluminum accumulation. The various syndromes of aluminum toxicity were first identified in dialysis patients, but they can occur in both Stage 4 CKD patients and Stage 5 CKD patients not yet treated with dialysis. Because of their devastating nature and the difficulties in their management, it is essential that the clinical features of aluminum toxicity are known along with the biochemical methods for their recognition. These problems have become substantially less common with the reduced use of aluminum gels as phosphate binders and proper purification of dialysate; however, aluminum toxicity still occurs. It is necessary to consider the means for proper monitoring and the appropriate diagnostic procedures needed to identify the various syndromes of aluminum toxicity.
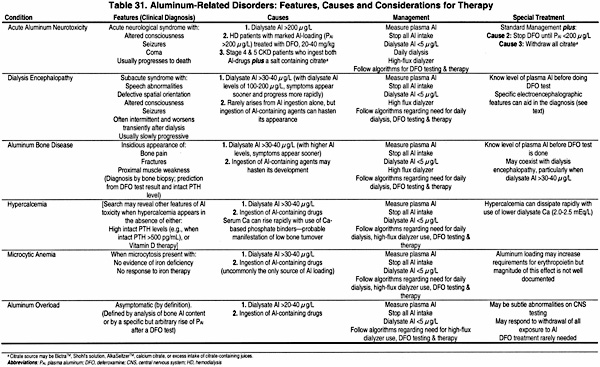
Aluminum toxicity occurs in dialysis patients or CKD patients with GFR <30 mL/min/1.73 m2 (Stages 4 and 5 CKD) because aluminum that is absorbed from the gut or enters the body from dialysate or another parenteral route390 is not excreted or is inadequately excreted by the diseased kidneys.391,392 When aluminum accumulates in dialysis patients, it is only slowly removed by dialysis because 90% of aluminum is bound to plasma proteins (primarily transferrin393,394). The aluminum entering the body accumulates in various tissues, including bone, brain, parathyroid glands, and other organs.395,396 Such accumulation of aluminum can produce toxicity with several distinct syndromes, depending on the rate and magnitude of aluminum loading. The first to be described was dialysis encephalopathy (or dialysis dementia).397,398 Aluminum was then recognized as the cause of both "fracturing dialysis osteomalacia" (aluminum-related bone disease)398-400 and a microcytic anemia developing without iron deficiency.401-403 A fulminant variant of dialysis encephalopathy, termed "acute aluminum neurotoxicity," occurs with the sudden, marked elevation of serum aluminum levels and is commonly fatal.404,405 These disorders are briefly described below. The development and availability of a method to measure trace quantities of aluminum accurately in biological fluids and tissues406 permits detection of these disorders, and this methodology provides a means to identify patients with increased body burden of aluminum (Table 31 and Algorithm 7).
Algorithm 6. Evaluation of aluminum neurotoxicity.
Algorithm 7. Evaluation of aluminum-related disorders: considerations for DFO test and subsequent DFO treatment.
Acute aluminum neurotoxicity.
Acute aluminum neurotoxicity is diagnosed based on clinical features and the elevation of plasma aluminum levels to 400 to 1,000 µg/L. It arises from aluminum contamination of dialysate, often to levels of 150 to 1,000 µg/L. As a rule, patients may become ill simultaneously in the same dialysis center. They develop agitation, confusion, myoclonic jerks, and major motor seizures; these symptoms are often followed by coma and death.404,405 The syndrome can also develop in patients with Stages 3 to 4 CKD (GFR <30 mL/min/1.73 m2) when they are given aluminum gels (to control hyperphosphatemia) plus sodium citrate (Bicitra™ or Shohl’s solution) for the correction of metabolic acidosis.407,408 Various citrate salts, including citric acid, sodium citrate, or calcium citrate, markedly enhance intestinal absorption of aluminum.171,409,410 Acute aluminum neurotoxicity can also appear in patients with large aluminum body load soon after the start of treatment with DFO in doses of 20 to 40 mg/kg.411,412 When acute aluminum neurotoxicity develops due to (1) very high dialysate aluminum levels or (2) the ingestion of both aluminum gels and citrate salts, most symptomatic patients have died.404,405,407,408 When the syndrome appeared in aluminum-loaded patients given DFO, some patients died; however, others survived when DFO treatment was stopped for several weeks and restarted later using a lower dose411,412
Dialysis encephalopathy.
Dialysis encephalopathy is an insidious disorder with symptoms generally appearing after patients have undergone dialysis for 12 to 24 months or even longer.397,398 Initial symptoms include subtle personality changes and a progressive speech disorder, characterized by stuttering, stammering and hesitant speech, or even total inability to talk.413 Motor disturbances include twitching, myoclonic jerks, and motor apraxia. Auditory and visual hallucinations, spatial disorientation, and paranoid behavior are common. These features can fluctuate widely and are characteristically worse shortly after dialysis. With time, the symptoms become persistent and worsen, seizures appear, and most untreated patients have died within 6 to 12 months after the onset of symptoms.397 The only distinctive laboratory findings were substantial elevations of plasma aluminum, usually 150 to 350 µg/L. The electroencephalographic (EEG) findings differ from the generalized slowing noted with other causes of metabolic encephalopathy. The diagnosis of these neurological disorders rests on clinical suspicion, the finding of elevated plasma aluminum levels, and the EEG features. New cases of this syndrome disappeared after the initiation of water purification.
Aluminum-related bone disease.
Aluminum-related bone disease was first described in certain specific geographic areas of the United Kingdom and the United States399,414; there was a suspicion of aluminum toxicity because many patients developed clinical features of dialysis encephalopathy.399,414 Epidemiological studies showed that this disorder—which presented with bone pain, a characteristic "waddling" gait, proximal muscle weakness and fractures401—was associated with dialysate aluminum levels above 100 µg/L.400 The disorder was limited to certain geographical regions, and aluminum-contaminated dialysate was considered the only source of aluminum loading. Later, sporadic cases appeared in dialysis centers where elevated dialysate aluminum levels were never found,415,416 and it was shown that small quantities of aluminum are absorbed from ingested aluminum gels.417 Such sporadic cases of aluminum bone disease have become less common since the use of aluminum gels were stopped or their dosage reduced substantially.14,418
Patients with aluminum-related bone disease often exhibit hypercalcemia,419,420 and PTH levels which are variably elevated, particularly with older C-terminal or mid-region PTH assays.420,421 Some of these patients had radiographic features of subperiosteal erosions and, when parathyroidectomy was done, the clinical features worsened. Bone biopsies revealed typical aluminum-related bone disease, and the term pseudohyperparathyroidism was applied to such patients.421 Other observations have documented the appearance or worsening of skeletal symptoms when patients with aluminum-related bone disease or aluminum loading had their PTH levels reduced by either parathyroid surgery422 or by treatment with an active vitamin D sterol.312,423
Indirect methods to identify aluminum-related bone disease were sought. Plasma aluminum levels were elevated in afflicted patients, with values usually above 100 µg/L; however, similar levels were found in many patients lacking bone biopsy evidence of aluminum-related bone disease.14,424 The DFO-infusion test, using DFO in doses of 20 to 40 mg/kg, was introduced to identify those with aluminum bone disease.425,426 The results indicate that the rise in aluminum correlated better with the total bone aluminum content than with surface staining of aluminum427,428; and that the presence of bone surface staining for aluminum of >15% to 25% showed a close association with clinical symptoms and with bone biopsy features of reduced bone formation and even osteomalacia, the histological features of aluminum bone disease.319,429,430
Population studies suggested that the combination of the increment of plasma aluminum after DFO combined with intact PTH levels below 150 pg/mL (16.5 pmol/L) provided better sensitivity and specificity to predict aluminum bone disease than the DFO test alone.426,431 Also, it was found that the sensitivity of the DFO test was reduced substantially in patients with no known exposure to aluminum for 6 months or longer.431 Most information indicates that plasma aluminum levels only reflect recent aluminum intake.432
Problems arose with use of the DFO test. Isolated reports documented permanent visual loss from ophthalmological damage after one DFO test with a dose of 40 mg/kg.433,434 Furthermore, as noted below under Treatment of Aluminum Toxicity, the use of DFO, 20 to 40 mg/kg, was associated with fulminant and fatal mucormycosis in an unacceptable number of dialysis patients.435 As a consequence, there has been reluctance to use a DFO test using 40 mg/kg, and smaller doses have been evaluated.436-438
Prevention of aluminum toxicity is preferable to use of toxic methods for treatment, particularly with the mortality of the neurological disorders and high morbidity of the bone disease. Periodic monitoring of plasma aluminum levels and assessment of aluminum in dialysate are essential for its prevention.
The evidence for the devastating neurological and skeletal disorders produced by contamination of dialysate with aluminum is compelling. However, these reports are not prospective, randomized trials. Obviously, such trials can never be done.
The evidence that aluminum is absorbed from aluminum hydroxide and other aluminum-containing compounds is indirect; however, the methodology for measuring true aluminum absorption using a stable isotope and mass spectroscopy is very expensive, has limited availability, and is likely to be done in very small numbers of patients. The close relationship between the cumulative aluminum intake and the skeletal accumulation of aluminum, along with the reduced prevalence of aluminum bone disease as the use of aluminum gels has decreased, provides only indirect—but convincing—evidence to recommend that aluminum gels not be used as phosphate binders, except for a very short periods of time.
The substantial reduction in prevalence of aluminum bone disease, and the apparent disappearance of this problem in dialysis units where aluminum gels are not used as phosphate binders, makes this a problem that may be disappearing.
Prospective comparison of aluminum gels and calcium-based phosphate binders was done in a small numbers of patients and was limited to 1 year of therapy.442 Also, the studies that showed the close correlation between the quantity of aluminum ingested and that present in bone at postmortem445 or on biopsy447 were not prospective studies.
Awareness of the various manifestations of aluminum toxicity by all health-care providers will allow early recognition of aluminum loading and aluminum toxicity in CKD patients. This will permit the earlier diagnosis and treatment of the syndromes of aluminum toxicity, thereby leading to reduced morbidity and disability. Use of the recommended low dose for the DFO test will minimize any risk of side-effects from the test. Such better safety should lead clinicians to use the DFO test with more confidence in clinical conditions when it may be useful or necessary. Through proper monitoring of plasma aluminum levels and the interpretation of these values, there will be earlier recognition of aluminum loading, with a greater ability to prevent the occurrence of aluminum toxicity.
Longitudinal studies with the measurement of serum aluminum at 6-monthly intervals from the very outset of dialysis, combined with a subsequent DFO test and bone biopsy in randomly selected patients and others chosen because serum aluminum levels rise >40 µg/L, could provide information on the “peak” aluminum levels at which there may be a risk of aluminum loading or the development of aluminum bone disease.
Limited long-term trials with very low doses of aluminum gels, which remain the most "potent" of phosphate binders, would be useful. Such doses, however, almost certainly would need to be combined with another type of phosphate-binding agent.
Large, prospective, long-term trials with the use of "low doses" of aluminum gels as phosphate binders would be useful. Those who remain convinced that low doses of aluminum are safe (and there remain some with this viewpoint) should seem compelled to design such trials to prove the point. Whether low doses of aluminum gels might be effective and safe when they are given in combination with continued "minidoses" of DFO treatment438 would be useful to consider for a prospective trial, particularly with the growing concern about potential risks of calcium-based phosphate binders.