NKF KDOQI GUIDELINES
KDOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification
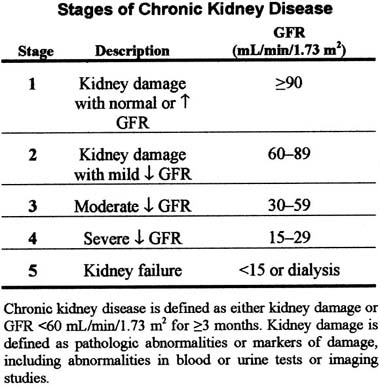
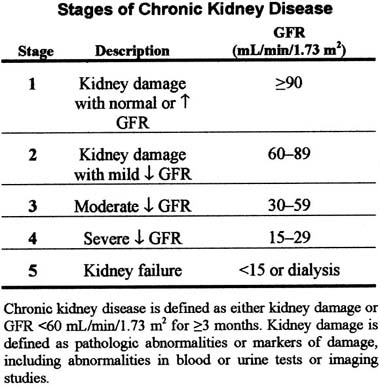
Guideline 1. Definition and Stages of Chronic Kidney Disease (p. S46)
Adverse outcomes of chronic kidney disease can often be prevented or delayed through early detection and treatment. Earlier stages of chronic kidney disease can be detected through routine laboratory measurements.
- The presence of chronic kidney disease should be established, based on presence of kidney damage and level of kidney function (glomerular filtration rate [GFR]), irrespective of diagnosis.
- Among patients with chronic kidney disease, the stage of disease should be assigned based on the level of kidney function, irrespective of diagnosis, according to the KDOQI CKD classification:
Guideline 2.
Evaluation and Treatment (p. S65)
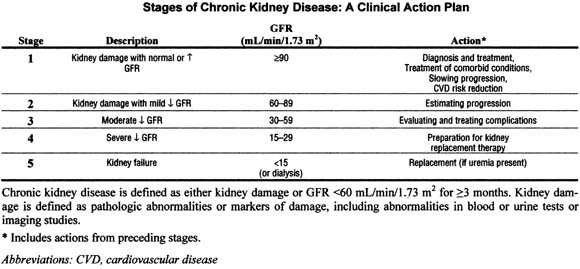
The evaluation and treatment of patients with chronic kidney disease requires understanding of separate but related concepts of diagnosis, comorbid conditions, severity of disease, complications of disease, and risks for loss of kidney function and cardiovascular disease.
Patients with chronic kidney disease should be evaluated to determine:
- Diagnosis (type of kidney disease);
- Comorbid conditions;
- Severity, assessed by level of kidney function;
- Complications, related to level of kidney function;
- Risk for loss of kidney function;
- Risk for cardiovascular disease.
Treatment of chronic kidney disease should include:
- Specific therapy, based on diagnosis;
- Evaluation and management of comorbid conditions;
- Slowing the loss of kidney function;
- Prevention and treatment of cardiovascular disease;
- Prevention and treatment of complications of decreased kidney function;
- Preparation for kidney failure and kidney replacement therapy;
- Replacement of kidney function by dialysis and transplantation, if signs and symptoms of uremia are present.
A clinical action plan should be developed for each patient, based on the stage of disease as defined by the KDOQI CKD classification (see table below).
Review of medications should be performed at all visits for the following:
- Dosage adjustment based on level of kidney function;
- Detection of potentially adverse effects on kidney function or complications of chronic kidney disease;
- Detection of drug interactions; and
- Therapeutic drug monitoring, if possible.
Self-management behaviors should be incorporated into the treatment plan at all stages of chronic kidney disease.
Patients with chronic kidney disease should be referred to a specialist for consultation and co-management if the clinical action plan cannot be prepared, the prescribed evaluation of the patient cannot be carried out, or the recommended treatment cannot be carried out. In general, patients with GFR <30 mL/min/ 1.73 m2 2 should be referred to a nephrologist.
Guideline 3.
Individuals at Increased Risk of Chronic Kidney Disease (p. S72)
Some individuals without kidney damage and with normal or elevated GFR are at increased risk for development of chronic kidney disease.
- All individuals should be assessed, as part of routine health encounters, to determine whether they are at increased risk of developing chronic kidney disease, based on clinical and sociodemographic factors.
- Individuals at increased risk of developing chronic kidney disease should undergo testing for markers of kidney damage and to estimate the level of GFR.
- Individuals found to have chronic kidney disease should be evaluated and treated as specified in Guideline 2.
- Individuals at increased risk, but found not to have chronic kidney disease, should be advised to follow a program of risk factor reduction, if appropriate, and undergo repeat periodic evaluation.
EVALUATION OF LABORATORY MEASUREMENTS FOR CLINICAL ASSESSMENT OF KIDNEY DISEASE (PART 5, p. S76)
The definition and staging of chronic kidney disease depends on the assessment of GFR, proteinuria, and other markers of kidney disease. The goals of Part 5 are to evaluate the accuracy of prediction equations to estimate the level of GFR from serum creatinine, the accuracy of ratios of protein-to-creatinine concentration in untimed (╦spotË) urine samples to assess protein excretion rate, and the utility of markers of kidney damage other than proteinuria. As described in Appendix 1, Table 151, the Work Group evaluated studies according to accepted methods for evaluation of diagnostic tests. To provide a more comprehensive review, the Work Group attempted to integrate the systematic review of specific questions with existing guidelines and recommendations.
Guideline 4.
Estimation of GFR (p. S76)
Estimates of GFR are the best overall indices of the level of kidney function.
- The level of GFR should be estimated from prediction equations that take into account the serum creatinine concentration and some or all of the following variables: age, gender, race and body size. The following equations provide useful estimates of GFR:
- In adults, the MDRD Study and Cockcroft- Gault equations;
- In children, the Schwartz and Counahan- Barratt equations.
- The serum creatinine concentration alone should not be used to assess the level of kidney function.
- Clinical laboratories should report an estimate of GFR using a prediction equation, in addition to reporting the serum creatinine measurement.
- Autoanalyzer manufacturers and clinical laboratories should calibrate serum creatinine assays using an international standard.
- Measurement of creatinine clearance using timed (for example, 24-hour) urine collections does not improve the estimate of GFR over that provided by prediction equations. A 24-hour urine sample provides useful information for:
- Estimation of GFR in individuals with exceptional dietary intake (vegetarian diet, creatine supplements) or muscle mass (amputation, malnutrition, muscle wasting);
- Assessment of diet and nutritional status;
- Need to start dialysis.
Guideline 5.
Assessment of Proteinuria (p. S93)
Normal individuals usually excrete very small amounts of protein in the urine. Persistently increased protein excretion is usually a marker of kidney damage. The excretion of specific types of protein, such as albumin or low molecular weight globulins, depends on the type of kidney disease that is present. Increased excretion of albumin is a sensitive marker for chronic kidney disease due to diabetes, glomerular disease, and hypertension. Increased excretion of low molecular weight globulins is a sensitive marker for some types of tubulointerstitial disease. In this guideline, the term ╦proteinuriaË refers to increased urinary excretion of albumin, other specific proteins, or total protein; ╦albuminuriaË refers specifically to increased urinary excretion of albumin. ╦MicroalbuminuriaË refers to albumin excretion above the normal range but below the level of detection by tests for total protein. Guidelines for detection and monitoring of proteinuria in adults and children differ because of differences in the prevalence and type of chronic kidney disease.
Guidelines for Adults and Children:
- Under most circumstances, untimed (ËspotÓ) urine samples should be used to detect and monitor proteinuria in children and adults.
- It is usually not necessary to obtain a timed urine collection (overnight or 24- hour) for these evaluations in either children or adults.
- First morning specimens are preferred, but random specimens are acceptable if first morning specimens are not available.
- In most cases, screening with urine dipsticks is acceptable for detecting proteinuria:
- Standard urine dipsticks are acceptable for detecting increased total urine protein.
- Albumin-specific dipsticks are acceptable for detecting albuminuria.
- Patients with a positive dipstick test (11 or greater) should undergo confirmation of proteinuria by a quantitative measurement (protein-to-creatinine ratio or albumin-to-creatinine ratio) within 3 months.
- Patients with two or more positive quantitative tests temporally spaced by 1 to 2 weeks should be diagnosed as having persistent proteinuria and undergo further evaluation and management for chronic kidney disease as stated in Guideline 2.
- Monitoring proteinuria in patients with chronic kidney disease should be performed using quantitative measurements.
Specific Guidelines for Adults:
- When screening adults at increased risk for chronic kidney disease, albumin should be measured in a spot urine sample using either:
- Albumin-specific dipstick;
- Albumin-to-creatinine ratio.
- When monitoring proteinuria in adults with chronic kidney disease, the protein to-creatinine ratio in spot urine samples should be measured using:
- Albumin-to-creatinine ratio;
- Total protein-to-creatinine ratio is acceptable if albumin-to-creatinine ratio is high (>500 to 1,000 mg/g).
Specific Guidelines for Children Without Diabetes:
- When screening children for chronic kidney disease, total urine protein should be measured in a spot urine sample using either:
- Standard urine dipstick;
- Total protein-to-creatinine ratio.
- Orthostatic proteinuria must be excluded by repeat measurement on a first morning specimen if the initial finding of proteinuria was obtained on a random specimen.
- When monitoring proteinuria in children with chronic kidney disease, the total protein- to-creatinine ratio should be measured in spot urine specimens.
Specific Guidelines for Children With Diabetes:
- Screening and monitoring of post-pubertal children with diabetes of 5 or more years of duration should follow the guidelines for adults.
- Screening and monitoring other children with diabetes should follow the guidelines for children without diabetes.
Guideline 6.
Markers of Chronic Kidney Disease Other Than Proteinuria (p. S103)
Markers of kidney damage in addition to proteinuria include abnormalities in the urine sediment and abnormalities on imaging studies. Constellations of markers define clinical presentations for some types of chronic kidney disease. New markers are needed to detect kidney damage that occurs prior to a reduction in GFR in other types of chronic kidney diseases.
- Urine sediment examination or dipstick for red blood cells and white blood cells should be performed in patients with chronic kidney disease and in individuals at increased risk of developing chronic kidney disease.
- Imaging studies of the kidneys should be performed in patients with chronic kidney disease and in selected individuals at increased risk of developing chronic kidney disease.
- Although several novel urinary markers (such as tubular or low-molecular weight proteins and specific mononuclear cells) show promise of future utility, they should not be used for clinical decision-making at present.
ASSOCIATION OF LEVEL OF GFR WITH COMPLICATIONS IN ADULTS (PART 6, p. S111)
Many of the complications of chronic kidney disease can be prevented or delayed by early detection and treatment. The goal of Part 6 is to review the association of the level of GFR with complications of chronic kidney disease to determine the stage of chronic kidney disease when complications appear. As described in Appendix 1, Table 152, the Work Group searched for crosssectional studies that related manifestations of complications and the level of kidney function. Data from NHANES III were also analyzed, as described in Appendix 2.
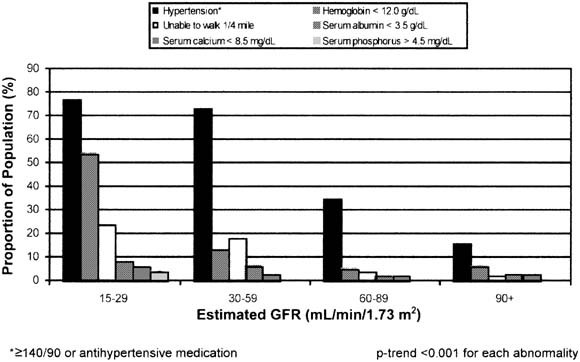
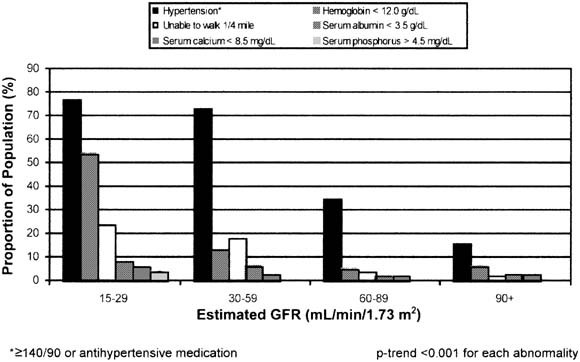
Estimated prevalence of selected complications, by category of estimated GFR, among participants age  20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR
20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR  90 mL/min/1.73 m2.
90 mL/min/1.73 m2.
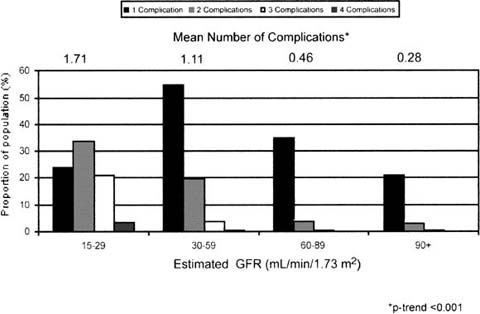
Estimated distribution of the number of complications shown in figure by category of estimated GFR among participants age  20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR of
20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR of  90 mL/min/1.73 m2.
90 mL/min/1.73 m2.
Because of different manifestations of complications of chronic kidney disease in children, especially in growth and development, the Work Group limited the scope of the review of evidence to adults. A separate Work Group will need to address this issue in children.
The Work Group did not attempt to review the evidence on the evaluation and management of complications of chronic kidney disease. This is the subject of past and forthcoming clinical practice guidelines by the National Kidney Foundation and other groups, which are referenced in the text.
Representative findings are shown by stage of chronic kidney disease in the figures above and below, showing a higher prevalence of each complication at lower GFR, and a larger mean number of complications per person and higher prevalence of multiple complications at lower GFR. These and other findings support the classification of stages of chronic kidney disease and are discussed in detail in Guidelines 7 through.
Guideline 7.
Association of Level of GFR With Hypertension (p. S112)
High blood pressure is both a cause and a complication of chronic kidney disease. As a complication, high blood pressure may develop early during the course of chronic kidney disease and is associated with adverse outcomes—in particular, faster loss of kidney function and development of cardiovascular disease.
- Blood pressure should be closely monitored in all patients with chronic kidney disease.
- Treatment of high blood pressure in chronic kidney disease should include specification of target blood pressure levels, nonpharmacologic therapy, and specific antihypertensive agents for the prevention of progression of kidney disease (Guideline 13) and development of cardiovascular disease (Guideline 15).
Guideline 8.
Association of Level of GFR With Anemia (p. S120)
Anemia usually develops during the course of chronic kidney disease and may be associated with adverse outcomes.
- Patients with GFR <60 mL/min/1.73 m2 should be evaluated for anemia. The evaluation should include measurement of hemoglobin level.
- Anemia in chronic kidney disease should be evaluated and treated (see KDOQI Clinical Practice Guidelines for Anemia of Chronic Kidney Disease, Guidelines 1-4).
Guideline 9.
Association of Level of GFR With Nutritional Status (p. S128)
Protein energy malnutrition develops during the course of chronic kidney disease and is associated with adverse outcomes. Low protein and calorie intake is an important cause of malnutrition in chronic kidney disease.
- Patients with GFR <60 mL/min/1.73 m2 should undergo assessment of dietary protein and energy intake and nutritional status (see KDOQI Clinical Practice Guidelines for Nutrition in Chronic Renal Failure, Guidelines 23 and 26).
- Patients with decreased dietary intake or malnutrition should undergo dietary modification, counseling and education, or specialized nutrition therapy (see KDOQI Clinical Practice Guidelines for Nutrition in Chronic Renal Failure, Guidelines 24 and 25).
Guideline 10.
Bone Disease and Disorders of Calcium and Phosphorus Metabolism (p. S143)
Bone disease and disorders of calcium and phosphorus metabolism develop during the course of chronic kidney disease and are associated with adverse outcomes.
- Patients with GFR <60 mL/min/1.73 m2 should be evaluated for bone disease and disorders of calcium and phosphorus metabolism.
- Patients with bone disease and disorders of bone metabolism should be evaluated and treated (see forthcoming KDOQI Clinical Practice Guidelines on Bone Metabolism and Disease in Chronic Kidney Disease).
Guideline 11.
Neuropathy (p. S156)
Neuropathy develops during the course of chronic kidney disease and may become symptomatic.
- Patients with chronic kidney disease should be periodically assessed for central and peripheral neurologic involvement by eliciting symptoms and signs during routine office visits or exams.
- Specialized laboratory testing for neuropathy in patients with chronic kidney disease is indicated only in the presence of symptoms.
Guideline 12.
Association of Level of GFR With Indices of Functioning andWell-Being (p. S161)
Impairments in domains of functioning and well-being develop during the course of chronic kidney disease and are associated with adverse outcomes. Impaired functioning and well-being may be related to sociodemographic factors, conditions causing chronic kidney disease, complications of kidney disease, or possibly directly due to reduced GFR.
- Patients with GFR <60 mL/min/1.73 m2 should undergo regular assessment for impairment of functioning and wellbeing:
- To establish a baseline and monitor changes in functioning and well-being over time;
- To assess the effect of interventions on functioning and well-being.
STRATIFICATION OF RISK FOR PROGRESSION OF KIDNEY DISEASE AND DEVELOPMENT OF CARDIOVASCULAR DISEASE (PART 7, p. S170)
The major outcomes of chronic kidney disease are loss of kidney function, leading to complications and kidney failure, and development of cardiovascular disease. The goals of Part 7 are to define risk factors for progression of chronic kidney disease and to determine whether chronic kidney disease is a risk factor for cardiovascular disease. Because of the well-known association of cardiovascular disease and diabetes, the Work Group considered patients with chronic kidney disease due to diabetes separately from patients with chronic kidney disease due to other causes. As described in Appendix 1, Table 153, the Work Group searched primarily for longitudinal studies that related risk factors to loss of kidney function (Guideline 13) and that related proteinuria and decreased GFR to cardiovascular disease (Guidelines 14 and 15). It was beyond the scope of the Work Group to undertake a systematic review of studies of treatment. However, existing guidelines and recommendations were reviewed, as were selected studies, to provide further evidence of efficacy of treatment.
Guideline 13.
Factors Associated With Loss of Kidney Function in Chronic Kidney Disease (p. S170)
The level of kidney function tends to decline progressively over time in most patients with chronic kidney diseases.
- The rate of GFR decline should be assessed in patients with chronic kidney disease to:
- Predict the interval until the onset of kidney failure;
- Assess the effect of interventions to slow the GFR decline.
- Among patients with chronic kidney disease, the rate of GFR decline should be estimated by:
- Computing the GFR decline from past and ongoing measurements of serum creatinine;
- Ascertaining risk factors for faster versus slower GFR decline, including type (diagnosis) of kidney disease and nonmodifiable and modifiable factors.
- Interventions to slow the progression of kidney disease should be considered in all patients with chronic kidney disease.
- Interventions that have been proven to be effective include:
- Strict glucose control in diabetes;
- Strict blood pressure control;
- Angiotensin-converting enzyme inhibition or angiotensin-2 receptor blockade.
- Interventions that have been studied, but the results of which are inconclusive, include:
- Dietary protein restriction;
- Lipid-lowering therapy;
- Partial correction of anemia.
- Attempts should be made to prevent and correct acute decline in GFR. Frequent causes of acute decline in GFR include:
- Volume depletion;
- Intravenous radiographic contrast;
- Selected antimicrobial agents (for example, aminoglycosides and amphotericin B);
- Nonsteroidal anti-inflammatory agents; including cyclo-oxygenase type 2 inhibitors;
- Angiotensin-converting enzyme inhibition and angiotensin-2 receptor blockers;
- Cyclosporine and tacrolimus;
- Obstruction of the urinary tract.
- Measurements of serum creatinine for estimation of GFR should be obtained at least yearly in patients with chronic kidney disease and more often in patients with:
- GFR <60 mL/min/1.73 m2;
- Fast GFR decline in the past (>4 mL/ min/1.73 m2 per year);
- Risk factors for faster progression;
- Ongoing treatment to slow progression;
- Exposure to risk factors for acute GFR decline.
Guideline 14.
Association of Chronic Kidney Disease With Diabetic Complications (p. S198)
The risk of cardiovascular disease, retinopathy, and other diabetic complications is higher in patients with diabetic kidney disease than in diabetic patients without kidney disease.
- Prevention, detection, evaluation, and treatment of diabetic complications in patients with chronic kidney disease should follow published guidelines and position statements.
- Guidelines regarding angiotensin-converting enzyme inhibitors or angiotensinreceptor blockers and strict blood pressure control are particularly important since these agents may prevent or delay some of the adverse outcomes of both kidney and cardiovascular disease.
Application of published guidelines to diabetic patients with chronic kidney disease should take into account their “higher risk” status for diabetic complications.
Guideline 15.
Association of Chronic Kidney Disease With Cardiovascular Disease (p. S204)
Patients with chronic kidney disease, irrespective of diagnosis, are at increased risk of cardiovascular disease (CVD), including coronary heart disease, cerebrovascular disease, peripheral vascular disease, and heart failure. Both “traditional” and “chronic kidney disease related (nontraditional)” CVD risk factors may contribute to this increased risk.
- All patients with chronic kidney disease should be considered in the “highest risk” group for cardiovascular disease, irrespective of levels of traditional CVD risk factors.
- All patients with chronic kidney disease should undergo assessment of CVD risk factors, including:
- Measurement of “traditional” CVD risk factors in all patients;
- Individual decision-making regarding measurement of selected “CKD-related” CVD risk factors in some patients.
- Recommendations for CVD risk factor reduction should take into account the “highest-risk” status of patients with chronic kidney disease.
![]() 20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR
20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR ![]() 90 mL/min/1.73 m2.
90 mL/min/1.73 m2.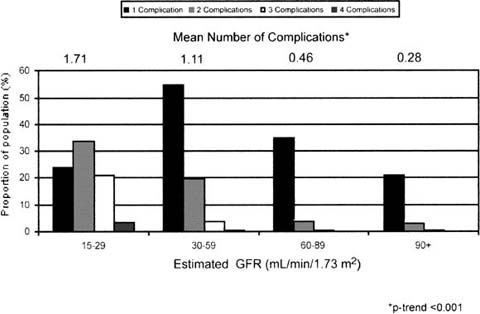
![]() 20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR of
20 years in NHANES III, 1988 through 1994. These estimates are not adjusted for age, the mean of which is 33 years higher at an estimated GFR of 15 to 29 mL/min/1.73 m2 than that at an estimated GFR of ![]() 90 mL/min/1.73 m2.
90 mL/min/1.73 m2.