Traditional risk factors—such as diabetes, hypertension, dyslipidemia—and those specific to dialysis patients (anemia and mineral metabolism abnormalities) require regular assessment and treatment as per current recommendations. The relative importance and weight of each of these risk factors in the dialysis population is not known and, in the absence of controlled trials in this population, current recommendations from existing organizations should be followed, with special consideration given to potential risks.
Furthermore, lifestyle issues such as smoking, physical activity, depression, and anxiety are the cornerstones of therapy as in the general population. The treatment options are often similar, but the impact of these factors is potentially more profound in dialysis patients. These factors are all discussed in this section. Special attention will be paid to the difference between the usual recommendations and those for dialysis patients.
Guideline 11: Diabetes
11.1 All dialysis patients who have diabetes should follow the American Diabetes Association guidelines.49,160(C)
Glycemic control (Weak)
The rationale for this ADA recommendation is based on substantial evidence from the Diabetes Control and Complications Trial (DCCT),161,162 and the U.K. Prospective Diabetes Study (UKPDS)163,164 that the careful control of blood glucose has a significant effect on decreasing the complications of diabetes. Combined with substantial observational evidence of the link between prolonged hyperglycemia and complications, the recommendation has strong evidence-based support. However, these relationships have not been validated specifically in dialysis patients. Tight control has potential problems for patients on dialysis, and there is some evidence that hemoglobin A1C may not be as predictive of glycemic control in patients on dialysis.
The ADA recommendation indicates that extremely tight control may increase the incidence of hypoglycemic events, and may produce weight gain. Hypoglycemia may be worsened by nausea and the inability to eat, as well as by longer duration of drugs and increased half-life of insulin. Therefore, care should be taken to prevent hypoglycemic episodes in patients on dialysis who experience significant nausea or gastrointestinal complaints. In addition, if excellent glycemic control gradually increases a patient’s solid weight, it should be reflected in the adjustment of dry weight for the purpose of postdialysis weight targets.
There is evidence that hemoglobin A1C is not as representative of glycemic control in patients on HD165 or PD.166,167 Through decreased metabolism, anemia, and shorter life of red cells, the hemoglobin A1C may under-represent glycemic control, and a level >7% in a dialysis patient may represent glycemic control similar to a nondialysis patient with a hemoglobin A1C <7%. The precise target of hemoglobin A1C that is associated with the best outcome in dialysis patients has not been clearly established. Clinicians are cautioned that insulin doses and oral hypoglycemic doses may change substantially during the transition from earlier stages of CKD to dialysis. The decrease in insulin catabolism associated with the further loss of kidney function may reduce insulin requirements. On the other hand, the glucose contained in the dialysate (especially peritoneal dialysate) may increase the requirement of hypoglycemic agents.
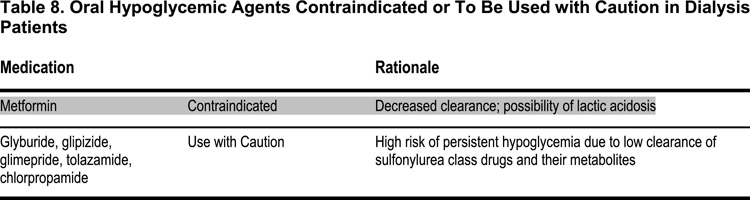
The use of newer insulin regimens and insulin preparations (with properties that are closer to normal physiology) should be encouraged, possibly in consultation with a specialist in diabetes management. There are some oral hypoglycemic agents that either should be used with caution, or not used at all, in dialysis patients (see Table 8).
Nutritional therapies and care (Weak)
The rationale for metabolic and nutritional management in diabetes comes primarily from a review by the ADA of the existing evidence, which supports nutritional interventions in the control of diabetes and its complications.160,168 In contrast, although health and dietary habits for diabetics are generally consistent with those for dialysis patients, there are special dietary considerations for patients on dialysis. The level of dietary protein recommended for dialysis patients exceeds the ADA recommendation for patients with diabetic nephropathy not requiring dialysis, because the prevention of malnutrition is a primary concern for dialysis patients. In patients not requiring dialysis, the slowing of progression of CKD is a major concern in which protein restriction probably has a role. High-protein diet may also cause more electrolyte imbalance and retention of nitrogenous waste products in nondialysis patients. On the other hand, dietary phosphorus restriction is often necessary to decrease hyperphosphatemia in dialysis patients. For more detailed recommendations, see the KDOQI Guidelines on Nutrition,169 and the sections on nutrition and calcium-phosphorus product in this document.
Exercise (Weak)
Patients who are on dialysis may have to modify their exercise routines to match their dialysis schedule, since postural hypotension, dizziness, and washout sensations are not uncommon, and exercise immediately after dialysis may be poorly tolerated.
Hypertension control (Weak)
The rationale for these recommendations derives from extensive reviews of the link between hypertension and cardiovascular morbidity and mortality for the general population and the statement of the Seventh Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure.170 The optimal blood pressure for dialysis patients, however, has not been firmly established (see Guideline 12 in this document). Although the JNC VII recommendation for blood pressure control in patients with CKD is <130/80 mm Hg, blood pressure control in patients on HD is complicated by the volume and electrolyte shifts surrounding dialysis procedure that acutely changes blood pressure. Diabetic patients on dialysis may be more prone to postural hypotension and labile blood pressure than nondiabetic dialysis patients. A higher supine blood pressure may be necessary in order to prevent symptomatic postural hypotension. Individual judgment and patient evaluation is required to match goals with symptoms.
Antihypertensive therapy (Weak)
The use of diuretics in patients on HD cannot be recommended for blood pressure control, unless there is substantial residual kidney function that responds to diuretics.171,172 The choice of initial pharmacological therapy for hypertension in dialysis patients is otherwise similar to those not on dialysis; however, the kidney-protective effect of ACE inhibitors and ARBs are less of a concern. Limited data suggest that ARBs may protect residual kidney function for patients on chronic PD. There is weak evidence that some beta-blockers may hinder peritoneal transport in patients on PD,173,174 but this evidence is not sufficient to warrant withholding the use of beta-blockers in dialysis patients when they are clearly indicated.
Finally, as detailed in Table 9, there are some antihypertensive agents that should not be used, or should be used only with care, in dialysis patients.
Cardiac disease screening (Weak)
The NKF KDOQI Guidelines support the need for cardiac screening in patients on dialysis, especially since the combination of diabetes and advanced kidney disease substantially increases the likelihood of coronary disease. The techniques for screening and their caveats in dialysis patients are described in Guideline 2 in this document.