The following sections have been prepared to ensure that the state of the art and science related to CVD includes novel concepts, therapeutic strategies, and emerging areas of pathophysiological and practical importance to the care of dialysis patients.
The reader will notice that the format of this section is different, reflecting its different perspective: namely, the relative lack of evidence on which to base plausible guideline statements. The evidence that does exist, and is cited in this section, is either completely in nondialysis populations, or is purely associative information, with no intervention in any population yet tested. Thus, it would be a problem to include guideline statements or recommendations.
Nonetheless, this section describes the current status of knowledge with respect to risk factors and biomarkers, and represents an overview of key areas for future clinical trials. The reader is encouraged to review this section, and examine his or her current understanding and practice within the context of these highlights.
The literature review has been conducted using the same systematic strategy as for the previous guidelines in this document. The reviews presented here have been thoughtfully constructed so that clinicians can adopt different practices based on them. However, for reasons cited above, the ability to truly recommend or suggest changes in practice would be premature at this time.
Oxidative stress is defined as the tissue damage resulting from the imbalance between an excessive generation of oxidant compounds and antioxidant defense mechanisms. It should be recognized that the generation of oxidative compounds is an important mechanism of normal physiology, playing a role in both inflammation and tissue repair processes. Thus, oxidative stress represents part of the defense mechanisms against invading micro-organisms and malignant cells, as well as a signal for tissue healing and remodeling. However, in a pathological situation, chronic activation of oxidative processes may contribute to cell and tissue injury.
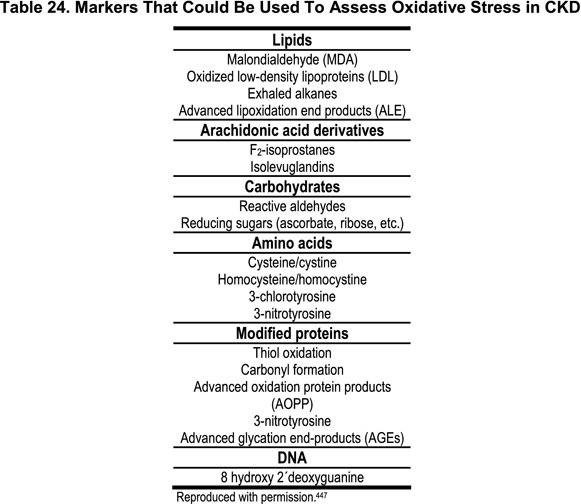
As oxidants are highly reactive species with a half-life of only seconds, in vivo determination is generally not feasible. However, some lipids, proteins, carbohydrates and nucleic acids are modified by oxy-radicals and have lifetimes ranging from hours to weeks. Therefore, these markers may serve as clinical surrogate markers of oxidative stress (Table 24). As oxidative stress occurs when the production of oxidants exceeds local anti-oxidant capacity, the prevention of the harmful effects of reactive oxygen systems—by both enzymatic and nonenzymatic antioxidant systems—are of major importance.447,448 Several deficiencies in different components of antioxidant defense mechanisms have been demonstrated in CKD. These include reduced levels of vitamin C, increased levels of oxidized vitamin C, reduced intracellular levels of vitamin E, reduced selenium concentrations, and deficiency in the glutathione scavenging system.448
Increased generation of oxidants in CKD
In the human body, oxidative activity is generated in the mitochondrial respiratory chain and in the phagocyte NADPH oxidase system.447,448 Among phagocyte-derived oxidants, chlorinating reactions catalyzed by myeloperoxidase (MPO) may be the most important. Activation of polymorphonuclear cells and secretion of MPO may link oxidative stress to both inflammation and endothelial dysfunction in CKD patients.449 The clinical importance of MPO activation is further underscored by the fact that both elevated leukocyte and blood MPO levels are associated, in the general population, with signs of CAD.450 Furthermore, in patients with acute coronary syndromes, MPO serum levels predicted subsequent cardiovascular events451 and identified patients at risk for cardiac events.452
Available evidence suggests that the balance between pro- and anti-oxidant capacities is shifted towards an increased oxidative stress in uremia.447,448 Factors contributing to increased pro-oxidant activity in CKD may include typical characteristics of the CKD patient population, such as advanced age and diabetes, uremia, chronic inflammation, malnutrition and factors associated with the dialysis treatment per se. Indeed, several recent studies have shown that various indicators of oxidative stress are increased in patients with CKD.453–455 Although some groups have reported a normal lipid peroxidation,456 most investigators457–459 have reported increased lipid peroxidation in CKD. Proteins and amino acids may also be elective targets of oxidant-mediated injury, and an increased formation of 3-chlortyrosine (a specific marker of MPO-catalyzed oxidation) has been demonstrated in HD patients.460 Moreover, increased levels of advanced oxidation protein products (AOPP) in CKD patients have been demonstrated.461 Oxidative compounds may also interact with nucleic acids to form 8-hydroxy-2′-deoxyguanosine, which has been used to evaluate leukocyte DNA damage. Significantly elevated levels of this marker of oxidative stress have been documented in CKD.462
Consequences of increased oxidative stress in CKD
In the general population, increased vascular oxidative stress was shown to predict cardiovascular events in those with CAD.463 Several recent studies indicate that increased oxidative stress may contribute to the excessive burden of cardiovascular morbidity and mortality also in CKD. It was shown that the serum anti-oxLDL antibody titer is an independent predictor of cardiovascular mortality in CKD patients.464 An association between AOPP and carotid arteriosclerosis was reported in HD patients.465 This finding was corroborated by a recent study showing that AOPP was an independent risk factor for CAD in the general population.466 Moreover, whereas oxidative stress was related to impaired endothelial function in a group of 37 CKD patients with moderate renal dysfunction,467 another group found that endothelial dysfunction is unrelated to LDL oxidation in a cross-sectional analysis of 23 dialysis and 16 nondialysis CKD patients.468 Clearly, the relationship between oxidative stress and endothelial dysfunction in CKD needs to be addressed in larger patient groups. The relationship between malonyldialdehyde (MDA) levels as an indicator of oxidative stress and the development of atherosclerosis was recently demonstrated in a cross-sectional study of 76 HD patients.469 Finally, two recent studies have demonstrated that two surrogate markers of oxidative stress, oxLDL470 and plasmalogen471 were associated with increased cardiovascular mortality in patients with advanced CKD. It is also notable that other complications in dialysis patients, such as amyloidosis, anemia, hypertension and malnutrition may be linked to increased oxidative stress.447,448 Although increased oxidative stress seems to be associated with many complications of CKD, no large, prospective epidemiological studies have yet demonstrated a link between oxidative stress and patient outcome.
Linking oxidative stress to inflammation and malnutrition
As increased oxidative stress, inflammation, and malnutrition all are common features of CKD, it has been speculated that there may be significant associations between them.449 Indeed, several recent clinical studies suggest links between oxidative stress, inflammation and malnutrition. The presence of inflammation and the duration of dialysis are the most important determinants of oxidative stress in HD patients.472 Associations between F2-isoprostanes and CRP levels have been reported in HD patients.453,454 A significant positive correlation is found between acute-phase proteins and markers of oxidative stress in a group of 64 predialysis patients.473 It has also been demonstrated that AOPPs act as mediators of oxidative stress and monocyte respiratory burst, which points to monocytes as both targets and actors in the immune deregulation associated with CKD.461 Different isoforms of vitamin E may have different activities. Thus, the administration of γ-tocopherol (in contrast to α-tocopherol) to patients with CKD results in a decrease in circulating levels of CRP.474 Finally, evidence suggests that malnourished CKD patients have increased oxidative stress compared to well-nourished patients,475 which is of interest as S-albumin can act as a binding protein for products of oxidation of carbohydrates, lipids and proteins,476 and redox active metals. Thus, it could be speculated that malnutrition, which is interrelated to chronic inflammation,434 may further contribute to cardiovascular morbidity and mortality by reducing both antioxidant defenses due to poor nutritional intake. Taken together, these observations may provide one explanation why hypoalbuminemia and inflammation so strongly correlate with cardiovascular mortality in both the general population477,478 and CKD patients.322,479
Treatment strategies for increased oxidative stress in CKD
Although epidemiological data suggest that the intake of vitamin E is inversely related to the development of CVD, large, prospective, randomized controlled trials all have failed to show that vitamin E supplementation improves cardiovascular outcomes in the general population.480 Moreover, a recent study showed that, whereas vitamin E supplementation did reduce circulating oxidized LDL, it did not reduce the progression of atherosclerosis in the general population.481 On the other hand, a study has shown positive results of vitamin E supplementation on outcome482 and the combination of vitamin E and C slowed the progression of carotid artery lesions in another study.483 As discussed elsewhere484 there may be a number of reasons why vitamin E supplementation failed to improve survival in these patient groups. In CKD patients, oral vitamin E supplementation has been shown to reduce the oxidative susceptibility of LDL,485 and to prevent the oxidative stress associated with anemia therapy or improve erythropoietin responsiveness.486 The SPACE trial tested the effect of vitamin E (800 IU/day) on a combined cardiovascular endpoint in 196 HD patients with pre-existing CVD, and showed a significant benefit from vitamin E supplementation.487 In contrast, a recent study reported no survival benefit of vitamin E in patients with mild to moderate CKD.488 In another recent study, treatment with the antioxidant acetylcysteine was associated with a reduced number of cardiovascular events in patients undergoing HD.489 Moreover, vitamin C supplementation in chronic HD patients can reduce the lymphocyte 8-OHdG levels and the production of intracellular reactive oxygen species.490 Based on these results, larger trials that are sufficiently powered to assess the effects of antioxidants on mortality appear highly desirable in CKD patients.
As the interaction between dialysis membranes and blood neutrophils can trigger oxidative stress491 direct scavenging at the membrane site is another attractive therapeutic approach. Thus, specific dialysis techniques (such as vitamin E-modified cellulose membranes) have been introduced in an attempt to reduce oxidative stress. However, although some studies have demonstrated beneficial effects of vitamin E-coated dialyzers on markers of oxidative stress,492 endothelial dysfunction,493 and cytokine induction,494 no study yet has, to the best of our knowledge, demonstrated any benefit of these expensive dialyzers on cardiovascular morbidity or mortality. Other modifications of the dialysis procedure may also reduce oxidative stress. Recently, it was shown that high-flux HD was associated with an improvement in some measures of protein oxidation.495 Another aspect of the management of CKD with potential clinical implications for oxidative stress is the treatment of anemia. As red blood cells contain high levels of antioxidants (in particular, reduced glutathione), it is possible that a rise in red cell mass may increase the total antioxidative capacity.496 On the other hand, the intravenous injection of iron may induce an increase in protein oxidation465,497 and carotid atherosclerosis.465 Therefore the relationship between anemia management and oxidative stress may be complicated.
Studies are needed to determine which surrogate marker of oxidative stress best predicts outcome in CKD patients. Further research is required to investigate the possible interactions between the presence of oxidative stress and both traditional risk factors (such as dyslipidemia) and non-traditional risk factors (such as inflammation, vascular calcification, advanced glycation end-products and endothelial dysfunction) for atherosclerosis. Studies are also needed to determine which oxidative stress pathway (i.e., nitrosative, chlorinated or carbonyl stress) is quantitatively the most important in CKD patients. Nonpharmacological (such as diet) and pharmacological (such as vitamin E and acetylcysteine) interventions for CKD patients with signs of increased oxidative stress should be developed and evaluated for efficacy in reducing oxidative stress and improving clinical outcomes in this patient group.
Oxidative stress, which is an important part of the host defense mechanism, may play a crucial role in the pathogenesis of atherosclerosis in CKD. Associations exist between increased oxidative stress, inflammation and endothelial dysfunction, which may contribute to increased risk of cardiovascular disease. As oxidants have very short half-lives they cannot be reliably evaluated in the clinical situation. Thus, the determination of oxidative stress relies on the use of more stable surrogate markers. Oxidative stress appears to play an important part in the pathogenesis of CVD in CKD patients. However, the benefit of antioxidant treatment strategies in this patient group remains undefined.