The following sections have been prepared to ensure that the state of the art and science related to CVD includes novel concepts, therapeutic strategies, and emerging areas of pathophysiological and practical importance to the care of dialysis patients.
The reader will notice that the format of this section is different, reflecting its different perspective: namely, the relative lack of evidence on which to base plausible guideline statements. The evidence that does exist, and is cited in this section, is either completely in nondialysis populations, or is purely associative information, with no intervention in any population yet tested. Thus, it would be a problem to include guideline statements or recommendations.
Nonetheless, this section describes the current status of knowledge with respect to risk factors and biomarkers, and represents an overview of key areas for future clinical trials. The reader is encouraged to review this section, and examine his or her current understanding and practice within the context of these highlights.
The literature review has been conducted using the same systematic strategy as for the previous guidelines in this document. The reviews presented here have been thoughtfully constructed so that clinicians can adopt different practices based on them. However, for reasons cited above, the ability to truly recommend or suggest changes in practice would be premature at this time.
The diagnosis of acute coronary syndromes in dialysis patients and the general population is usually based on the triad of symptoms, electrocardiographic findings, and cardiac biomarkers. The presence of a time-dependent elevation in serum cardiac troponin T or I levels in the setting of acute coronary syndromes is associated with increased cardiovascular morbidity and mortality.
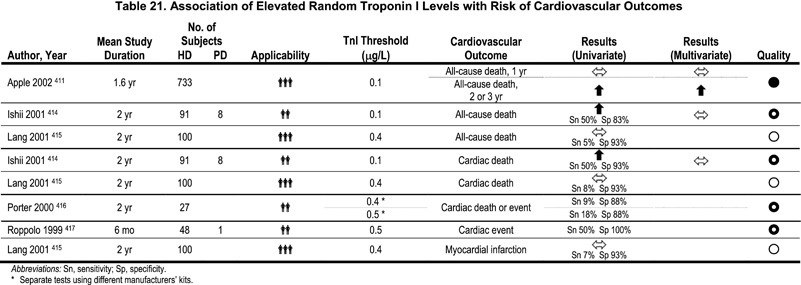
An emerging indication for the measurement of cardiac troponins is risk stratification in asymptomatic HD patients, in the absence of other signs and laboratory tests suggestive of acute coronary syndromes (Table 21,Table 22). Several published studies have demonstrated that the presence of elevated serum cardiac troponin T, and—to a lesser extent—troponin I, is a powerful predictor of mortality in HD patients. In a prospective study of 733 asymptomatic outpatients on chronic HD, serum troponin was highly predictive of all-cause mortality (Fig 5).411 Patients without detectible troponin T had a 2-year 8% mortality, with progressively higher mortality predicted by increasing ranges of the biomarker. Patients with troponin T >0.1 μg/L had a 2-year mortality of approximately 50%. Another study found a significant correlation between the increase in serum troponin T levels and the severity of CAD in a subset of asymptomatic HD patients.412 It is plausible that the elevation in serum cardiac troponins in asymptomatic dialysis patients is a reflection of silent IHD and nonischemic cardiomyopathy, and troponin levels have been related to LV mass.413 Troponin elevation (as seen in dialysis patients, i.e., not following a time-appropriate rise and fall after an index ischemic event) has been reported in patients with severe nonischemic cardiomyopathy. Regardless, it is clear that these elevations in cardiac troponin levels in dialysis patients are not spurious findings. The clearance of troponins may be altered in dialysis patients, but the source is cardiac.
Figure 5 - Kaplan-Meier Survival Curves by Baseline Troponin Levels. The number of patient at risk at baseline, 1 year, 2 years and 2.5 years for each cutoff is shown at the bottom of the graph, The 99th percentile refers to the normal reference limit. The 10% CV refers to the lowest concentration that demonstrates a 10% total precision. The ROC cutoff refers to concentrations optimized for the sensitive and specific detection of MI.411 Reproduced with permission.
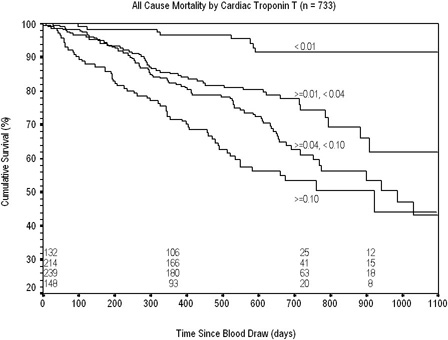
The potential clinical duality of troponin testing in dialysis patients needs to be recognized. The diagnosis of acute coronary syndromes and risk stratification in nonischemic settings are discrete, but complementary tasks. It is a key issue that a time-appropriate rise and fall of the cardiac biomarker occurs in acute coronary syndromes; as serum troponin elevation is prognostically important, but not necessarily indicative of acute coronary syndrome. The operational characteristics of different-generation troponin assays vary widely and—unfortunately, as new assays become available—nullify conclusions attributable even to recent data. Although troponin I may “currently” be the best cardiac biomarker for diagnosis of acute coronary syndrome (see Fig 5B; only 45 of 733 [6%] asymptomatic dialysis patients had any detectible troponin I), based on “specificity” criteria, this may not necessarily be correct for the next generation of troponin I and T assays.
A prospective, randomized clinical trial on troponin testing and clinical decision-making would provide valuable information. There is a need for prospective cohort studies on the correlation between troponin levels and the burden of CAD, as well as fatal and nonfatal CAD-related and non-CAD-related events.
Therefore, serum troponin T levels should be considered for risk stratification in chronic dialysis patients. In HD patients, the blood samples should be collected before dialysis. The utility of troponin T for risk stratification in PD patients has not been reported, but there is no obvious reason to suspect that these patients differ from HD patients in this regard. The assay for troponin T is widely available. However, it is currently unclear how this information can be utilized. For example, should an elevated serum troponin T level be followed by another diagnostic test (e.g., stress imaging) or therapeutic intervention (e.g., the administration of beta-blockers)? To determine the appropriate therapeutic consequences, understanding of the precise causes of death in dialysis patients with elevated serum troponin levels, and the underlying pathophysiological mechanisms, must be improved.
A credible case can be made for recommending the measurement of serum cardiac troponins in dialysis patients for the purpose of risk stratification (distinct from the diagnosis of acute coronary syndrome). Indeed, in May 2004 the U.S. Food and Drug Administration approved the measurement of troponin T in patients with chronic renal failure (i.e., dialysis) for the express purpose of risk stratification (i.e., prediction of mortality). The KDOQI Work Group has not designated this as a practice guideline, however, because of uncertainty at the present time regarding appropriate clinical strategies using this information.