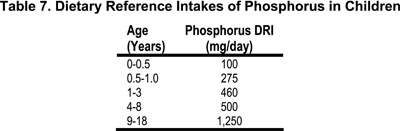
5.1 Dietary phosphorus should be decreased to the Dietary Reference Intake (DRI) for age (Table 7) when the serum PTH concentration is above the target range for the stage of CKD and serum phosphorus is within the target range for age (Table 6, Guideline 4). (OPINION)
5.2 Dietary phosphorus should be decreased to 80% of the DRI for age (Table 7) when the serum PTH concentration is above the target range for the stage of CKD and serum phosphorus is above the target range for age (Table 6, Guideline 4). (OPINION)
5.3 After initiation of phosphorus restriction, serum phosphorus concentrations should be monitored at least every 3 months in patients with CKD Stages 3-4, and monthly in patients with CKD Stage 5. Serum phosphorus values below the target range for age should be avoided.
In children20,74,96 and adult patients97-103 with CKD, serum concentrations of PTH are increased early, i.e., when the GFR is only mildly to moderately reduced, and the values of PTH vary inversely with those of GFR.103 When the GFR decreases into CKD Stage 3 and below (<60 mL/min/1.73m2), serum concentrations of PTH are above the normal range in most children and adult patients, and histological evidence of bone disease is observed.20,104,105 At this level of GFR, however, serum concentrations of phosphorus are within the normal range or even mildly decreased,74,96,98,106,107 and values become clearly increased only when CKD Stage 4-5 is reached. Thus, in CKD Stages 2 and 3, hyperphosphatemia is rarely present and 2° HPT can be attributed, at least in part, to the reduction in serum concentrations of 1,25(OH)2D.74,96,101-103,108-117
Although serum phosphorus levels are not increased in the early stages of progressive CKD, dietary phosphorus is nevertheless an important determinant of the severity of hyperparathyroidism in mild and moderate, as well as severe, renal insufficiency. In both children and adult patients with mild and moderate CKD (Stages 2 and 3) in whom serum concentrations of PTH were increased and those of serum phosphorus normal, dietary phosphorus restriction induced a decrease in serum levels of PTH and an increase in levels of 1,25(OH)2D, the latter to normal or supernormal values.74,100,118 Conversely, in children with Stage 3 CKD, supplementation of dietary phosphorus to intakes approximately twice the DRI for age induced a worsening of hyperparathyroidism and further decrease in serum levels of 1,25(OH)2D.74 Such changes in serum PTH could be attributed, at least in part, to diet-induced changes in serum levels of 1,25(OH)2D. Phosphorus manipulation in patients with CKD Stage 2 and 3 induced little or no change in morning fasting serum phosphorus concentrations.74,100,118
Thus, in CKD Stages 2 and 3, the severity of hyperparathyroidism can be amplified or reduced by increases or decreases, respectively, in dietary phosphorus intake. Since dietary phosphorus intakes above the DRI can contribute to the severity of hyperparathyroidism, it is the opinion of the Work Group that phosphorus intakes be decreased to the DRI even when serum phosphorus levels are within the target range. In CKD Stages 4 and 5, serum phosphorus levels are typically above the target range, and phosphorus restriction to approximately 80% of the DRI is recommended.
The higher serum concentrations of calcium and phosphorus in healthy infants and young children, and their physiological decrease with age, presumably reflect the increased requirements of these minerals by the growing skeleton. This is particularly important in the newborn infant, as infancy is the period of most rapid accretion of bone mineral. Hence, when dietary phosphorus is restricted to control hyperphosphatemia and 2° HPT in children with CKD, serum phosphorus values below the target range should be avoided. Rickets due to phosphorus deficiency occurs in preterm infants fed insufficient amounts of phosphorus, and in infants and children with hypophosphatemia due to inherited disorders of renal phosphate transport.119 Severe restriction of dietary phosphorus in children with moderate and severe renal insufficiency was associated with a decrease in fasting levels of serum phosphorus and histological findings of worsening osteomalacia.118
Studies in children with CKD Stages 2-3 that examine the relationship between serum phosphorus concentration and 2° HPT suggest that dietary phosphorus restriction can improve 2° HPT and maintain normal serum phosphorus levels. Data in adult patients with CKD support an association between the increase in serum phosphorus concentration and decrease in GFR, and reveal that hyperphosphatemia is observed when the creatinine clearance decreases to CKD Stages 4-5.120
The effectiveness of dietary phosphate restriction in controlling the hyperphosphatemia of CKD in children and adults was analyzed in 19 studies examining 2,476 patients. Fifteen randomized controlled trials121-135 and four nonrandomized controlled trials136-139 met the inclusion criteria. The vast majority of studies evaluated restricted protein diets, which are usually (but not always) equivalent to low phosphorus diets. In many of these studies, calcium94,140-147 and vitamin D supplements were used,80,83,85,86,94,140-148 or phosphate binders were also administered to the patients in addition to the dietary intervention. Thus, the interpretation of these data should be done with caution. Various end-points were utilized:
Quality of life. One study reported that low protein diet did not adversely affect employment,138 but the results of the Modification of Diet in Renal Disease (MDRD) study indicated that patients with CKD (Stages 3 and 4) treated with very restricted protein diets were less able to socialize.149
Mortality. Nearly all of the included studies evaluated the role of dietary restriction of protein/phosphorus on mortality. The reported results were variable. When these data were analyzed by meta-analysis, no effect on mortality was found.
Kidney function. Seven of nine studies in adult patients with CKD suggest that dietary phosphorus restriction may stabilize kidney function.121,124,125,129-131,133,136,139 Conclusions in this regard could not be drawn from studies in children or in adults with severe CKD.
Bone and mineral metabolism. Several small studies reported that dietary phosphorus restriction in patients with CKD had no significant effect on serum alkaline phosphatase,123,125,134,137 PTH levels125,134,136,138 serum calcium levels,123,125,134,136,137 serum phosphorus levels,123,132,134,136,137,150 and urinary phosphate excretion.127,129,132 In contrast, in a careful and well-controlled study of four patients with Stages 1 and 2 of CKD conducted in a metabolic ward before and after 8 weeks of dietary phosphate restrictions in proportion to the decrement in GFR, there was a reduction in blood PTH levels to normal without significant changes in the serum levels of phosphorus, significant decrements in blood levels of alkaline phosphatase and in urinary excretion of phosphate, and significant increments in blood levels of 1,25(OH)2D3 and intestinal absorption of calcium.100 Also, the dietary phosphate restriction was associated with marked improvement in bone resorption and defects in bone mineralization as evidenced by studies of bone biopsy.100
In children, the initiation of moderate dietary phosphate restriction needs to be accompanied by close monitoring of linear bone growth. In four studies in children, there was no evidence for adverse effects as a result of dietary phosphate restriction.124,128,151,152 In addition, studies in adults did not support any adverse effect on nutritional status as a result of dietary phosphate restriction.123-125,127,129,131,133,134,137,139,153,154
Compliance with dietary restriction in the research setting of clinical studies may not reflect the situation in clinical practice. While compliance with dietary phosphorus restriction in clinical practice is commonly believed to be poor, there is a lack of data to support this supposition. Most studies have found compliance rates of 35%-91% with low-protein diets.124,132,149,155 One study reported 41% and 77% compliance at years 1 and 3, respectively.156 The compliance rates with dietary phosphate restriction were similar to compliance rates for low-protein diets. It was not addressed whether the improvement at year 3 is related to continuous education and/or the realization by the patient of the adverse effects of noncompliance.
Given the lack of evidence of adverse effects, and the evidence of positive benefit of dietary phosphate restriction, it is the consensus of the pediatric (and adult) Work Group that modification of dietary phosphate intake be initiated in patients with CKD when PTH levels are elevated.
Despite the relatively large number of prospective randomized trials evaluating dietary phosphorus restriction, most of these studies specifically utilized protein-restricted diets and therefore restricted phosphate intake indirectly. While protein and phosphorus are closely related in foods, it is possible to restrict protein without fully restricting phosphorus. Much of the data are also difficult to interpret since most of the reports provided analysis for “prescribed diet” rather than “consumed diet.” Furthermore, in many studies, the patients had concomitant therapy with vitamin D and/or phosphate binders, making interpretation of the results difficult.
While the available data do not support the common belief that dietary phosphate restriction negatively impacts nutritional status, it must be stressed that dietary phosphate restriction has the potential of adversely impacting nutritional status if done in a haphazard manner. The data that demonstrate the ability to maintain good or stable nutritional status during dietary phosphate restriction were obtained in studies in which dietitians provided careful instruction and regular counseling and monitoring. In the research setting, patients are monitored closely and have regular contact with their renal care providers. Those patients who have been “casually” instructed to watch their protein or phosphate intake, without regular follow-up, may be at risk for serious side-effects, such as malnutrition. Unfortunately, there are no data on those patients who are not regularly and closely followed.
It is critical to provide consistent instruction and regular follow-up during prescription of dietary phosphate restriction. In patients with CKD, compliance with dietary phosphate restriction is difficult and requires intensive dietitian support. In CKD patients treated with dialysis (Stage 5), care must be taken to reduce phosphate intake while maintaining adequate protein intake as recommended by the KDOQI Guidelines on Nutrition.157 The phosphate level of the diet should be as low as possible while ensuring an adequate protein intake. If one multiplies the recommended protein level by 10-12 mg phosphate per gram of protein, a reasonable phosphate level can be estimated. The average amount of phosphorus per gram of protein ranges from 12-16 mg. In order to limit phosphorus significantly, those protein sources with the least amount of phosphorus must be prescribed (see Table 12, Guideline 7).
There is a need for large, multicenter longitudinal studies evaluating the effects of dietary phosphate restriction (as opposed to only protein restriction) on nutritional status, growth in children, morbidity, mortality, bone disease, and progression of decline in kidney function. These studies should be conducted in patients with all stages of CKD, beginning in Stage 2.