4.1 Minimally adequate dose:
The minimally adequate dose of HD given 3 times per week to patients with Kr less than 2 mL/min/1.73 m2 should be an spKt/V (excluding RKF) of 1.2 per dialysis. For treatment times less than 5 hours, an alternative minimum dose is a URR of 65%. (A)4.2 Target dose:
The target dose for HD given 3 times per week with Kr less than 2 mL/min/1.73 m2 should be an spKt/V of 1.4 per dialysis not including RKF, or URR of 70%. (A)4.3 In patients with residual urea clearance (Kr) greater than or equal to 2 mL/min/1.73 m2, the minimum session spKt/V can be reduced. One method of minimum dose reduction is described in CPR 4.4. In such patients, the target spKt/V should be at least 15% greater than the minimum dose. (B)
4.4 Missed and shortened treatments:
Efforts should be made to monitor and minimize the occurrence of missed or shortened treatments. (B)
Minimally Adequate Dose (CPG 4.1)
The present adequacy guideline for a minimally adequate dose remains unchanged from the previous (2000) guidelines.6 In deciding whether this guideline needed to be changed, the committee considered 3 lines of evidence. The first was results of the primary analysis of the NIH HEMO Study, published in 2002.1 The committee also had access to as-treated results of the HEMO Study, which were published at the time the draft guidelines were released in November 2005.98 This report was judged to be of some importance because it identified a dose-targeting bias in the analysis of delivered therapy versus mortality in cross-sectional data sets, which potentially impacts on the weight of evidence derived from such data sets. The second was a series of articles suggesting that dosing of dialysis should not be based on URR or its derivative, Kt/V (which essentially is volume of blood cleared divided by the modeled urea volume, V), but on the volume of blood cleared (Kt) only.78,99-101 The third was a series of analyses of delivered dose (ie, URR) versus mortality based on either the USRDS-Medicare data set or the Fresenius Medical Care subset of these data.102-104
HEMO Clinical Study: Primary (Randomized) Results
Primary results of the HEMO Study, which randomized patients to a delivered eKt/V of 1.16 versus 1.53, equivalent to URR values of about 63% versus 75% or spKt/V values of about 1.3 versus 1.7, revealed little evidence to support increasing the dose of dialysis beyond the current (2000) KDOQI recommendations, respectively.6 The lack of benefit, without even a trend that was close to statistical significance, appeared not only in the primary outcome of mortality, but also in a variety of main secondary composite outcomes relating to various causes of hospitalization combined with mortality. Furthermore, analysis of minor secondary composite outcomes dealing with nutritional measures—including changes in weight and serum albumin levels,105 as well as QOL measures106—also failed to support a beneficial effect of increasing the dose of dialysis. Of all trials evaluated, the HEMO Study was by far the largest, and its randomized design and measurement of hard outcomes were given an enormous weight in determining whether the 2000 KDOQI HD Adequacy Guidelines needed to be changed. The Work Group realized that the recently published European guidelines recommended substantially higher minimal doses of HD based on an eKt/V measure, corresponding to spKt/V minimum targets of about 1.4 to 1.5.12
HEMO Clinical Study: As-Treated Results
The HEMO dose-versus-mortality question also was assessed within each treatment arm, measuring the effects of actual delivered dose over time versus mortality.98 This study identified a dose-targeting bias and suggested that patients in a cross-sectional analysis receiving less dialysis are also at greater risk for death. This increased death risk was of a high magnitude and was incompatible with a biological effect of dose. Although conditions of the 2 HEMO Study arms were not representative of how dialysis is prescribed in the field, documentation of such a strong potential dose-targeting bias (which may be operative in cross-sectional studies, albeit to a lesser degree) convinced the Work Group members to place less weight on dose-versus-mortality relationships derived from observational studies despite the large numbers of patients included in such studies.
Studies Advocating Alternate Measures of Urea-Based Adequacy
These studies are discussed in more detail in CPG 2, Methods for Measuring and Expressing the HD Dose. Since the 2000 KDOQI HD Adequacy Guidelines were published, 1 group of investigators in particular, using data derived from Fresenius Medical Care North America patients in the United States, argued that dose of dialysis should not be factored by modeled V.78,100,101 The arguments against using URR or its derivative Kt/V fall into 2 general categories: (1) doing so may result in relative underdialysis of women and small patients of both sexes, and (2) because modeled V is itself a predictor of mortality, use of dialysis dose factored by V may confound dialysis dose-versus-mortality relationships found in cross-sectional studies in complex and not always predictable ways. A secondary analysis of the intent-to-treat results of the HEMO Study suggested that the higher dose of dialysis may result in better survival in women, who also tended to be smaller than the men in that particular trial.13 The Work Group decided, based on suggestive evidence, that more dialysis (beyond 2000 KDOQI levels) may be better for women and, perhaps, smaller patients, but that the level of evidence did not reach a point at which the existing guideline should be changed. Hence, 2 CPRs were derived suggesting that more dialysis in women and/or in smaller patients might be beneficial (see Section II). Despite the theoretical arguments, as well as attempts to address confounding effects of V in cross-sectional data sets, the committee believed that, at present, the data are not compelling enough to depart from the 2000 recommendation to follow small-molecule clearance using Kt/V.
Given the increased use of conductivity to measure clearance during the dialysis session, the Work Group also considered using an anthropometric volume as the clearance denominator when clearance was measured by conductivity. Using an anthropometric volume as denominator was speculated to result in a more stable denominator, less affected by errors in predialysis and postdialysis urea nitrogen determinations. For example, (Kecn× T/Vant, where Vant = anthropometrically-estimated total body water distribution volume) could be used instead of Kt/V urea. The Work Group's conclusion was that there were not sufficient data comparing sequential dialysis adequacy measures by using both conductivity and urea kinetics in the same patients to make such a major revision, although it was recognized that from a quality-assurance perspective, it would be less challenging to ensure a constant dialysis dose given a more constant denominator. Concerns also were raised about altered modeled to anthropometric urea volume ratios in individual patients, although given the relative flatness of the adequacy to mortality curve, this issue may be of secondary importance.
Another potential strategy discussed was to normalize the dialysis amount to a denominator based on BSA as opposed to urea volume, whether the latter was derived from modeling or anthropometrics. For example, this is accomplished easily by multiplying the target Kt/V value by 3.27 × V/V0.667 (V raised to the 2/3 power). Such a correction method (developed by the Frequent HD Network investigators) gives the same dialysis dose when V = 35 L, but then augments the dose when V is less than this amount and reduces the dose when V is larger, giving, in effect, a dose based on BSA instead of V. Again, for lack of definitive clinical outcomes evidence supporting this approach, it was left for perhaps a future revision of the guidelines when more data might be available.
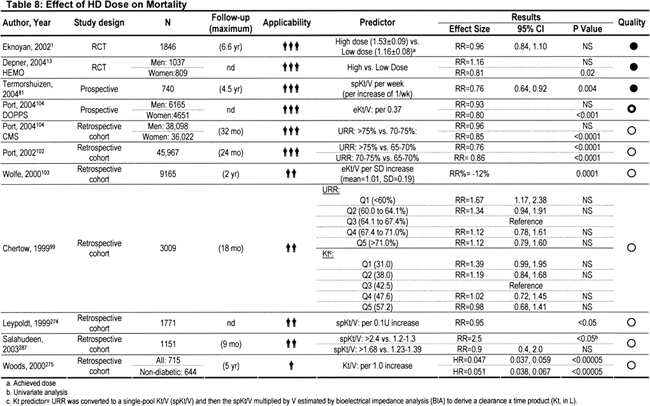
Dose-Related Mortality in Large Observational Data Sets
Since the KDOQI 2000 HD Adequacy guidelines were published, a number of studies, including analyses of USRDS Annual Data Reports, continued to examine the relationship between dose of dialysis and mortality. Most, but not all, observational studies reported dose in terms of either spKt/V or URR. The dose-versus-mortality relationship was examined as a function of race and sex57,104 and as influenced by various measures of body size102,103 and nutritional status.99 Because the general median spKt/V increased over time, these analyses included much larger samples of patients receiving higher doses of dialysis. Most of these analyses suggested that increasing the dose of dialysis above the target recommended in the 2000 guidelines to levels targeted in the high-dose arm of the HEMO Study (spKt/V ~ 1.7) should decrease mortality by a substantial amount (Table 8). However, the lack of concordance between these observational results and negative results of the HEMO Study, coupled with the dose-targeting bias identified in the as-treated analysis of HEMO Study patients, restrained the Work Group from recommending a global increase in recommended spKt/V for patients dialyzed 3 times per week.
Renal Clearance Compared With the 2000 Guidelines
The 2000 KDOQI HD Adequacy Guidelines were applied to patients with a Kr less than 5 mL/min/1.73 m2, for which Kr is defined as the average of urea and creatinine clearances. In the present guidelines, the committee decided to use urea clearances for the purpose of specifying minimally adequate urea fractional removal. This allows more accurate measurement of protein catabolism in patients with significant Kr and an opportunity to combine Kr with Kd (see CPG 2). Urea clearance of 3 mL/min corresponds approximately to an average of urea and creatinine clearances of 5 mL/min. In the present guidelines, this number was reduced to 2 mL/min of normalized urea clearance to enable some decrease in dialysis dose for patients with moderate degrees of RKF, as discussed in the accompanying CPR. A more complete discussion of why this “step” strategy was adopted, rather than the addition of residual clearance as a continuous function, is detailed in the accompanying CPR.
Target Dose (CPG 4.2)
The KDOQI 2000 HD Adequacy Guidelines specified a target spKt/V of 1.3, with a minimally adequate dose of 1.2 per dialysis given 3 times per week. During the course of measuring the dose of therapy many times in each patient enrolled in the HEMO Study, the variability of modeled volume and hence of spKt/V was determined accurately. The within-patient coefficient of variation for single-pool V in the HEMO patient data set was close to 10%. The relationship between target Kt/V and subsequent achieved Kt/V is shown in Table 9.
As shown in Table 9, the previous recommendations to target 1.3 would result in about 21% of treatments at any given time apparently being less than the Kt/V minimum target of 1.21 (the fraction > 1.2 is 0.79, so 0.21, or 21%, would be < 1.2). Thus, it appears that targeting 1.3 would result in needless prescription modifications and/or troubleshooting. Targeting therapy at an spKt/V of 1.4 and averaging results from 3 monthly measurements of adequacy results in a much greater proportion of treatments (in the range of 97%), greater than the minimum 1.2 adequacy target. Setting the target dose of dialysis to 1.4, rather than 1.3, also seemed to be justified given suggestive results (not yet qualifying for guideline-generating status) that subsets of patients might benefit from higher doses of dialysis.
Avoiding Missed Treatments (CPG 4.3)
Measurement of fractional urea removal during a single dialysis treatment obviously is not a monthly average of dialysis adequacy and has validity only if dialysis treatments are delivered reliably 3 times per week on a regular basis. A number of studies document that the number of missed and/or shortened dialysis treatments in US dialysis patients (4% missed treatments per month) is more than the number missed by their counterparts in other countries, such as Japan.107 Whereas the KDOQI 2000 HD Adequacy Guidelines suggested increasing the frequency of measuring Kt/V or URR in patients for whom treatments frequently were shortened or missed, they did not address the issue of monitoring and minimizing the occurrence of missed and shortened treatments. A number of studies suggested that poor compliance in HD, especially in terms of number of missed treatments, is an important predictor of mortality and hospitalizations.14-16 For this reason, the Work Group believed that every dialysis center should have a mechanism in place to monitor and minimize the occurrence of missed and shortened dialysis treatments.