Prospective randomized trials and observational studies have confirmed that the presence of RKF is one of the most important predictors of a patient's survival.
6.1 One should strive to preserve RKF in HD patients. (A)
6.2 Methods for preserving RKF differ among patients (see CPR 6). (B)
When HD therapy is first initiated, most patients have small and significant (but inadequate) levels of RKF, and many have normal or even high rates of urine output. This level of RKF may persist for many months and years, adding continuous solute clearance and other kidney functions to the intermittent clearances provided by dialysis treatments. The volume of urine produced each day allows more fluid intake, reducing the otherwise larger fluctuations in body fluid volumes between dialysis treatments that contribute to volume overload syndromes, hypertension, and cardiac hypertrophy. Unlike hemodialyzer clearance, RKF is subject to temporary or permanent reduction caused by numerous toxic insults that often confront patients with CKD stage 5.
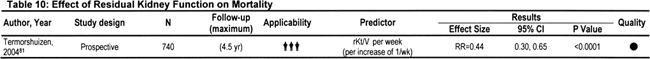
The impact of residual function on duration of life and QOL has been evaluated extensively in PD patients,68,225-227 but only recently has attention been given to it in HD patients (see Table 10).81 This difference is especially striking because the number of long-term HD patients in the United States is more than 10 times as large as the number receiving PD. Possible reasons for ignoring RKF include a lack of RKF measurements in HD patients, complacency because of confidence in the larger dose of dialysis possible with HD, previous rapid decrease in urine output after HD therapy is begun, and the added inconvenience and expense of collecting urine. Measurement of RKF in HD patients also likely was ignored because, in contrast to PD, nearly all KRT is managed for the patient by nurses and technicians. Selecting a subgroup of patients who prefer self-care (PD) also selects for willingness to perform self-measurements of RKF. There also has been concern that PD is minimally adequate; thus, RKF may play a more essential role. Earlier studies showed that RKF decreased more rapidly in patients initially treated with HD compared with continuous ambulatory PD (CAPD).228 However, recent studies showed that RKF is preserved better in HD patients than in the past, possibly because of the use of more biocompatible membranes, discontinuation of acetate as a bicarbonate precursor, high-flux dialysis, and the earlier initiation of dialysis therapy, especially in patients with diabetes.81,229-231 More recent studies suggest that with the use of ultrapure water to dilute concentrated dialysate, RKF decreases at a rate indistinguishable from that in CAPD patients.232
The protective role of RKF for preserving life and extending longevity in PD patients is well recognized68,226,227; previous KDOQI guidelines promoted the preservation of RKF in this population.233 More recent data show that RKF in HD patients affords many of the same benefits, including a lower dialysis dose requirement and improved patient survival.234 The reduced need for dietary potassium and fluid restriction and reduced requirement for fluid removal during HD can enhance QOL and reduce the frequency of hospitalizations. In HD patients, the continuous nature of RKF contrasts with the intermittent schedule of dialysis, whereas for PD patients, both are nearly continuous. Evidence that includes mathematical analysis of solute kinetics and comparison of outcomes in PD versus HD patients suggests that continuous clearance is more efficient than intermittent clearance.235 Such arguments have been used, for example, to explain the much lower weekly dialysis clearance requirement in PD compared with HD patients despite nearly equal outcomes, especially in the first year of treatment. If this difference in efficiency is accepted, the contribution of RKF to overall kidney plus dialyzer function is greater than the simple addition of time-averaged clearances would suggest.
Because it appears that RKF can be preserved, every effort should be made to protect existing renal function in HD patients, especially if daily urine volume exceeds 100 mL. When measures are taken to protect RKF after initiation of HD therapy, patients may continue to experience long-term benefits, even at very low GFRs.
Suggested methods to protect RKF are detailed in CPR 6.
Data that support reducing the dose of dialysis in patients with significant residual function are all observational. The recent randomized trial of HD dose1 intentionally excluded patients with significant residual function; therefore, little dosing information for patients with RKF is available. It is possible that patients with residual function can derive more benefit from doses of dialysis targeted for anephric patients compared with the downward adjusted dose; therefore, a firm recommendation to reduce the dose is not possible at this time.
In rare cases, persistence of nephrotic-range proteinuria may necessitate renal embolization or removal of the kidneys. Occasionally, renal endocrine function (eg, renin secretion) contributes to hypertension, necessitating ablation or removal of the native kidneys. This scenario is much less common today compared with 40 years ago because potent antihypertensive agents are readily available. Occasionally, removal of residual kidney mass may be required to manage bacterial pyelonephritis. Before transplantation, removal of obstructed kidneys or kidneys with stones or cysts causing infections that cannot be completely eradicated with antibiotics may be warranted. In these cases, careful timing of the transplantation and nephrectomy can maximize benefit from RKF while also reducing the risk of transplantation. In some cases, removal of a transplanted kidney is warranted to eliminate symptomatic inflammation caused by continued allograft rejection.