The continuous quality improvement (CQI) process has been shown to improve outcomes in many disciplines, including CKD stage 5.
5.1 Each home-training unit should establish quality improvement programs with the goal of monitoring clinical outcomes and implementing programs that result in improvements in patient care. (B)
5.2 Quality improvement programs should include representatives of all disciplines involved in the care of the PD patient, including physicians, midlevel practitioners, nurses, social workers, dietitians, and administrators. (B)
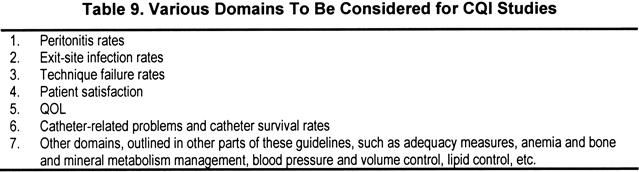
5.3 Suggested domains of clinical activities one should consider monitoring are listed in Table 9. (B)
It is important that each facility establish a CQI program because such programs have been shown to improve outcomes in a variety of disciplines, including the care of patients with CKD stage 5. The domains to be examined need to be considered carefully at each facility. Areas that present particular problems at an individual facility should receive special attention. Because the CQI program will involve review of patient-related activities from a variety of domains, it is important that representatives of all disciplines involved in the care of PD patients (physicians, nurses, social workers, dietitians, and administrators) be included in the CQI process.
There are certain special domains that should be considered for CQI examination for PD facilities, outlined in Table 9. These domains are in addition to the standard therapeutic targets outlined in other parts of the KDOQI Guidelines, which include adequacy measures, blood pressure and volume control, anemia and bone mineral metabolism management, lipid control, etc.
Technique failure is an important issue for PD facilities.127-129 Technique failure is defined as patients discontinuing PD for reasons other than death or transplantation. It accounts for a variable percentage of the reasons that patients terminate PD therapy. The most common reasons reported for technique failure include peritonitis, catheter-related problems, psychosocial factors, and problems with ultrafiltration or poor clearances.127-129 Programs are encouraged to evaluate the reasons that patients terminate PD therapy and then develop strategies for improving outcomes.
Peritonitis remains a leading cause of morbidity for PD patients and has been associated with mortality, hospitalizations, and termination of PD therapy.130-132 Although peritonitis rates have improved significantly during the past several years, peritonitis remains a major issue for PD units. It is important for facilities to develop strategies for tracking peritonitis rates, assessing the organisms responsible for peritonitis, and developing strategies to better understand the reasons for peritonitis. In addition, treatment guidelines for peritonitis have been established by the International Society of PD.130 Each facility needs to evaluate which treatment strategy is best for its program; this depends on understanding the rate of peritonitis, organisms causing peritonitis, and possible reasons for peritonitis.
Exit-site infections are a problem for PD patients because these infections may be responsible for peritonitis and lead to catheter removal.133-135 Treatment guidelines have been developed for the management of exit-site care and infections.133,134 Facilities should evaluate their exit-site infection rates and review whether their treatment practices provide acceptable levels of care.
A variety of catheters and insertion methods have been used for PD patients. There is insufficient evidence to recommend one type of catheter or one catheter placement technique.136 Each facility should examine catheter success rates and methods of catheter insertion and track these results over time.
QOL assessments for dialysis patients have been the focus of several studies. A variety of instruments have been used for these assessments; there is no generally agreed-upon or accepted instrument to perform these assessments. However, it should be noted that various findings on these QOL assessments have correlated significantly with morbidity and mortality rates in patients with CKD stage 5 maintained on both HD and PD therapy.137-141 Monitoring QOL may be particularly important for a home-based therapy.142 This is especially so because PD therapy is associated with significant technique failure rates and requires patient cooperation and compliance. It should be noted that QOL assessments may present problems in terms of using standardized instruments in geographically, linguistically, and culturally different groups. Although some domains of QOL problems are amenable to therapy,76,143 it has not been shown that interventions to improve QOL decrease adverse clinical outcomes.
Patient satisfaction with therapy for CKD stage 5 also has been attracting increased attention recently.144,145 As treatment options for patients with CKD stage 5 expand, it is important to monitor how patients feel about their treatment and their facility so that appropriate modifications can be made to improve patients' perceptions of their therapy and care. This is an important issue to consider for all patients, but is particularly relevant for patients on a home-based therapy, for whom adequate communication between the staff and the patient is essential. There are no generally agreed-upon instruments to assess patient satisfaction with care, but facilities are encouraged to consider examining methods of evaluating this domain.
Although CQI programs generally are considered to be beneficial, there are no studies of PD facilities that document the efficacy of such programs on improving patient outcomes.
The institution of effective CQI programs requires that adequate information be made available and resources be provided to the facility to effectively manage these programs. It is important for the facility to strive to provide the materials necessary to permit CQI programs to operate effectively.
Some of the areas suggested for CQI activity in Table 9 do not have established standards or instruments to assess these domains (eg, patient satisfaction, QOL). Several studies attempted to assess these domains, and each facility will need to review these studies and select instruments that it believes are appropriate.