2.1 The most accurate diagnostic test for determining the type of bone disease associated with CKD is iliac crest bone biopsy with double tetracycline labeling and bone histomorphometric analysis. (EVIDENCE)
2.2 It is not necessary to perform bone biopsy for most situations in clinical practice. However, a bone biopsy should be considered in patients with kidney failure (Stage 5) who have:
2.2a Fractures with minimal or no trauma (pathological fractures); (OPINION)
2.2b Intact plasma PTH levels between 100 and 500 pg/mL (11.0 to 55.0 pmol/L) (in CKD Stage 5) with coexisting conditions such as unexplained hypercalcemia, severe bone pain, or unexplained increases in bone alkaline phosphatase activity; (OPINION)
2.2c Suspected aluminum bone disease, based upon clinical symptoms or history of aluminum exposure. (OPINION) (See Guideline 11.)
2.3 Bone radiographs are not indicated for the assessment of bone disease of CKD, (EVIDENCE) but they are useful in detecting severe peripheral vascular calcification (OPINION) and bone disease due to ß2-microglobulin amyloidosis. (See Guideline 10.) (EVIDENCE)
2.4 Bone mineral density (BMD) should be measured by dual energy X-ray absorptiometry (DEXA) in patients with fractures and in those with known risk factors for osteoporosis. (OPINION)
Bone disease may occur early in the course of CKD, and worsens as the decline in kidney function progresses. In Stage 5 CKD, bone disease is common and, by the time dialysis is initiated, nearly all patients are affected. In addition, patients with CKD (especially those at Stage 5) have an above-average risk for bone fractures.39,40
Beginning at Stage 3, patients with CKD almost always have secondary hyperparathyroidism and elevated blood levels of PTH.31,41-46 In these patients, the classical lesion that is seen in bone biopsy is osteitis fibrosa cystica due to hyperparathyroidism,14,23,26,47-54 although recent studies have shown increasing prevalence of other bone lesions such as low-turnover bone disease.14,23,33,47-51,53,55-62
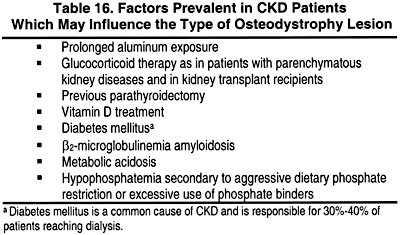
In addition to secondary hyperparathyroidism, there are other factors that are common in CKD patients and may have a major impact on boneand mineral metabolism. A partial list of some of these factors is shown in Table 16.
Current therapy with biologically active 1a-hydroxyvitamin D metabolites, as well as the use of various phosphate-binding agents, adjustments of dialysate calcium, and introduction of other drugs (such as anti-bone resorptive agents), have led to the emergence of bone disorders associated with low or nearly normal levels of parathyroid hormone. Many of these latter lesions are associated with below-normal rates of bone formation (adynamic or low-turnover bone disease).
CKD patients with prolonged exposure to aluminum-based phosphate binders (see Guidelines 11 and 12) and those with diabetes mellitus14,23,47,55-59,62 have lower blood levels of PTH than other patients with comparable levels of kidney function. Aluminum deposition in bone, secondary to aluminum overload, interferes with bone mineralization (see Guidelines 11 and 12). Therefore, low-turnover and/or adynamic bone disease may be more prevalent in these patients.
Patients with CKD may also have other factors that are not related to their CKD, but may impact bone and mineral metabolism (Table 17). Advanced age and deficiency in sex hormones (estrogen and androgens) are associated with osteoporosis and loss of bone mass. Nutritional vitamin D deficiency, medications that affect vitamin D metabolism such as anticonvulsants, and/or hypophosphatemia would cause defective mineralization of osteoid leading to osteomalacia.
Bone Histomorphometric Diagnoses
In general, bone histomorphometric examinations can help classify bone diseases into one of the following general diagnostic categories: mild hyperparathyroid bone disease; moderate-to-severe hyperparathyroid bone disease; mixed bone disease; osteomalacia; or adynamic bone disease (Table 18). Histochemical aluminum staining may show deposition of aluminum in any of these conditions, and suggest coexisting aluminum-related bone disease, coexistent with the basic type of osteodystrophy of CKD. Osteoporosis and osteopenia are characterized by decreased in trabecular or cortical bone volume on bone biopsy. Osteopenia may also be diagnosed by alternate means, such as DEXA, permitting selective determination of bone mineral density in the entire skeleton or in specific regions (eg, lumbar spine, hip, femoral neck).
In deciding when it is appropriate to perform a bone biopsy in patients with chronic kidney disease, 2 questions should be considered:
Regarding the first question, it has been established that blood levels of PTH begin to rise when GFR falls below 60 mL/min/1.73 m2,31,41-46 and levels of Vitamin D [1,25(OH)2D3] fall at this level of GFR.45,63-67 Since these developments are considered central to the development of bone disease in CKD patients, it is reasonable to assume that bone disease begins at Stage 3 of CKD (when GFR declines below 60 mL/min/1.73 m2) and that it progresses as GFR continues to decline.
Despite considerable advances in the understanding of the pathophysiology, prevention, and treatment of osteodystrophy of CKD, there is no adequate substitute for bone biopsy in establishing the histological type of osteodystrophy in these patients.23,24,26,47-51,53 Over the past 50 years, bone biopsy has provided the most accurate diagnosis of the type of bone disease in both CKD and non-CKD patients. Over the last 3 decades, quantitative bone histomorphometry with double tetracycline labeling has become the "gold standard" for the diagnosis of metabolic bone disease in CKD patients.14,23,33,48-53,55,57,68-75
There have been many reports of bone biopsy findings in patients with CKD that have documented abnormalities in bone histology with increasing prevalence, when the GFR has declined below 50 to 60 mL/min/1.73 m2.14,23,26,47-54
Several studies have demonstrated a direct correlation between elevated blood levels of intact PTH and bone biopsy findings of increased bone turnover, the main feature of bone disease due to hyperparathyroidism (Fig 6).23,24,26,32-34,58 Evidence of increased bone resorption has been detected in bone biopsies obtained from CKD patients with a GFR below 60 mL/min/1.73 m2 when blood levels of PTH begin to rise.31,41-46
The prevalence of osteopenia and/or osteoporosis also increases with decreasing levels of GFR.31 In a study of patients with CKD, the highest levels of BMD in the lumbar spine, hip and distal forearm were found in those with GFR between 70 and 110 mL/min/1.73 m2 (Stage 1 and 2 CKD), while those with GFR between 6 and 26 mL/min/1.73 m2 (Stage 4 CKD) had the lowest BMD levels (Fig 6).31 The abnormalities in bone metabolism that might be responsible for the decreased BMD were not characterized in these studies. The presence of osteoporosis is a strong predictor of increased risk for fractures in the general population. Therefore, the measurement of BMD by DEXA is an important diagnostic procedure for the identification of CKD patients who are more prone to fractures. Three recent studies have noted an increased risk of fracture in CKD patients.39,40,76 However, there are limited data on the correlation of BMD with fractures in CKD.77
There were very few studies of bone biopsies that met all of the inclusion criteria as described in the Method of Analysis of the Literature. This was due to differences in patient populations, various definitions of bone disease, and incomplete information regarding the level of kidney function. Many studies were retrospective in nature, and therefore subject to potential bias. None of the studies met the criteria for highest quality (ie, double-blind, placebo-controlled, randomized), but sufficient information was available to permit some conclusions. Overall, a relatively small amount of moderate- to high-quality studies and a small amount of data were relevant to the issues in this Guideline. Effect size could be calculated for individual studies in many instances, but it was not possible to combine multiple studies into an overall statistical analysis. Therefore, certain biases may occur in this interpretation due to the fact that most studies had to be evaluated individually.
The use of bone biopsy as a diagnostic tool requires trained personnel for the preparation of a decalcified section of the biopsy and for performing the morphometric analysis. At present, these personnel are not available in most medical institutions. Reimbursement for obtaining and interpreting bone biopsies should be made available, and will require education of payors as to the importance of bone biopsy in the diagnosis and management of patients with CKD.
The Work Group recognized that, in most circumstances, clinicians will have to depend upon indirect methods, rather than bone biopsy, to diagnose the type of bone disease associated with CKD. The reasons for lack of more frequent use of bone biopsy include: patient refusal; a mistaken perception that bone biopsy is painful and overly invasive; the lack of local resources to properly procure, process, and reliably interpret the bone biopsy; and difficulty in obtaining appropriate reimbursement for bone biopsy performance.
Recognizing these limitations, the Work Group agreed that in the following circumstances, a bone biopsy will often yield essential information and should be strongly considered:
The Work Group agreed that bone biopsy should also be considered in some patients prior to parathyroid ablation therapy. If the clinical history includes oral or parenteral aluminum exposure, then a bone biopsy may be helpful to exclude the coexistence of hyperparathyroidism and aluminum bone disease (see Guidelines 11 and 12). In these circumstances, parathyroid ablation therapy may worsen aluminum toxicity of bone; therefore, aluminum toxicity must be excluded prior to parathyroidectomy. In other patients, the levels of PTH may not be excessively elevated, yet there may be other suggestions of excessive effects of PTH (hypercalcemia, hyperphosphatemia, elevated bone alkaline phosphatase activity, bone resorption on X-ray, etc). In such patients, inappropriate parathyroid ablation can induce hypoparathyroidism and adynamic bone disease. For this reason, any patient with PTH levels less than 800 to 1,000 pg/mL (88.0 to 110.0 pmol/L) may require bone biopsy prior to parathyroid ablative therapy, to clearly document the increased bone formation rate and histological findings of hyperparathyroidism prior to an ablative procedure.
Several conditions should be satisfied to ensure that the bone biopsy provides reliable information:
Considering the invasive nature of bone biopsy, there is a need to investigate whether other markers of bone disease could be developed to replace bone biopsy for the accurate diagnosis of bone disease in patients with chronic kidney disease.
At the present time, there are not any noninvasive tests that have sufficient accuracy for the diagnosis of bone disease in CKD patients. The Work Group recommends that bone biopsy be used to accurately establish the diagnosis in CKD patients enrolled in clinical research protocols studying bone disease. These protocols may be designed to assess the sensitivity or specificity of other diagnostic tests, or to assess the effectiveness of various therapies. In either instance, accurate diagnosis of the bone disease is pivotal to the quality and utility of such studies.
Most of the currently used PTH assays are purported to measure only the "intact" PTH molecule, consisting of 84 amino acids. Most of the biological activity of the PTH molecule resides in the N-terminal, and, in large part, in the amino acid residues in positions 1 to 7. It appears that many "intact PTH" assays also detect biologically inactive fragments of PTH formed from the amino acids in the 7 to 84 positions.81-83 This phenomenon leads to spurious elevations in the levels of intact PTH in CKD patients, in that these patients do not have significant hyperparathyroid bone disease even though the PTH level is above normal. If clinicians attempt to maintain intact PTH levels of CKD patients in the "normal" range below 65 pg/mL (7.15 pmol/L), then some CKD patients have low levels of bone formation and adynamic bone disease.81-83 Hence, our current recommendations distinguish between the "desired target range" for intact PTH in CKD patients and the "normal range" that has been determined for patients with normal kidney function.