Hypertension is common in children with CKD. Because of their young age at onset of CKD and hypertension, children have a high lifetime exposure to risk factors for CVD. Thus, children with CKD are at high risk of complications from hypertension.
13.1 Measurement of blood pressure in children should be performed with age- and size-appropriate equipment, and blood pressure values should be interpreted according to normal values adjusted for age, gender, and height percentile, as recommended by the 1996 Update on the Task Force Report on High Blood Pressure in Children and Adolescents: A Working Group Report from the National High Blood Pressure Education Program (A).
13.2 The cause of CKD and age of the child should be considered in selecting the class of antihypertensive agent (A).
13.3 Target blood pressure in children should be lower than the 90th percentile for normal values adjusted for age, gender and height or 130/80 mm Hg, whichever is lower (B).
13.4 Because of the specialized nature of CKD and blood pressure management in children, a pediatric kidney disease specialist should be involved in their care, when possible (C).
The long-term consequences of hypertension in the adult population including CVD in CKD are well documented. As in the adult population, hypertension in children is more common in obese children, in the African-American population, and in children with a family history of hypertension. The consequences of hypertension detected in childhood and adolescence are beginning to be elucidated but there are no long-term studies to correlate childhood hypertension to CVD during adulthood. However, it has been shown that coronary artery plaques correlate with SBP in young adults who died of other causes,559 and cardiac abnormalities detected by echocardiography are found in a substantial proportion of adolescents with hypertension560,561 and in children with ESRD.562 Ambulatory hypertension has also been shown to correlate with echocardiographic evidence of left ventricular dysfunction and increased intima-media thickness.563 Thus, it is reasonable to conclude that children with hypertension have an increased risk of complications of hypertension. Indeed, because of the early onset of hypertension and the extended lifetime exposure to these risk factors, it is logical that children with CKD and hypertension have a particularly high risk for these complications.
The rising prevalence of obesity in childhood has implications for risk of CKD in childhood and for the treatment of hypertension in children with CKD. First, obesity is a risk factor for hypertension and type 2 diabetes, leading causes of CKD in adults. Thus, the incidence and prevalence of CKD in children may increase in the future. Second, obesity in children with CKD may lead to an increased risk of hypertension or worsen pre-existing hypertension, increasing the risk of premature onset of CVD. Coexisting type 2 diabetes may further increase the risk of CVD. As in adults, multi-intervention therapy will be necessary for effective therapy of CKD in children (Guideline 1).
Definitions
For this guideline, the age range for children is defined as birth through 18 years. Few studies have been performed in children with CKD to demonstrate the efficacy of blood pressure management in preserving kidney function or in preventing CVD. Thus, current recommendations for therapy in children need to take into consideration studies performed in adults with CKD and studies demonstrating the efficacy of management of hypertension in children without CKD.
Studies of adult patients with high blood pressure and CKD have led to the recognition of accelerated CVD and that hypertension is a major risk factor for CVD in CKD.4 Studies in the adult population with CKD have also demonstrated that antihypertensive therapy retards the progression of CKD. Similar studies documenting that these risk factors and complications are pertinent to children have not been performed. However, studies have demonstrated that signs of CVD are apparent in children with CKD564,565 While there are very few published studies to demonstrate that therapy of hypertension in children with CKD decreases CVD, it is likely that children with CKD and hypertension are at risk for the same complications that occur in adults. In fact, children with CKD are probably at higher risk for CVD due to the early age at onset of CKD and hypertension, and a higher cumulative lifetime exposure to these risk factors. USRDS statistics demonstrate that the death rate of children with kidney failure treated by dialysis and transplantation is markedly higher than the death rate in healthy children and that cardiac events are an important cause of death.566 Thus, optimal blood pressure management in children with CKD is very important to decrease the risk of CVD. Compared to adults, several differences in children need to be considered when blood pressure management is initiated in children with CKD.
Strength of Evidence
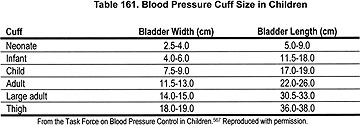
Normal blood pressure is lower in children than adults. Appropriate measurement devices and age-adjusted normal values are necessary for accurate measurement and interpretation of blood pressure in children (Strong). Blood pressure should be measured with equipment that is appropriate to the age and size of the child, and The Report of the Second Task Force on Blood Pressure Control in Children—1987 and the Task Force Report on High Blood Pressure in Children Update detail the methods for accurate measurement of blood pressure in children as well as normative values.567,568 Correct blood pressure measurement in children requires the use of a cuff that is appropriate to the size of the child’s arm. The cuff should cover at least two thirds of the upper arm and the bladder should encircle 80% to 100% of the circumference of the arm. There are six different sizes of cuffs for use in children (Table 161 and Figs 58 through 61).
Fig 58. Blood pressure cuff dimensions. Dimensions of bladder and cuff in relation to arm circumference. A, ideal arm circumference; B, range of acceptable arm circumferences; C, bladder length; D, midline of bladder; E, bladder width; F, cuff width. Reproduced with permission.153
Automated devices using oscillometric methods to measure blood pressure are very commonly used in newborns and young infants. Blood pressure should be measured when the infant is calm and quiet while resting comfortably. The Task Force recommends that blood pressure be measured at least twice in a controlled environment after at least 3 to 5 minutes of rest in the seated position. Normative data are based on blood pressure measurements in the right arm with the child seated.
Fig 59. Determination of proper cuff size, step 1. The cuff bladder width should be approximately 40% of the circumference of the arm measured at a point midway between the olecranon and acromion. Reprinted with permission.568
Fig 60. Determination of proper cuff size, step 2. The cuff bladder should cover 80% to 100% of the circumference of the arm. Reprinted with permission.568
Fig 61. Blood pressure measurement. Blood pressure should be measured with cubital fossa at heart level. The arm should be supported. The stethoscope bell is placed over the brachial artery pulse, proximal and medial to the cubital fossa, below the bottom edge of the cuff. Reprinted with permission.568
Normal blood pressure is lower in children than in adults. Blood pressure increases with age and with body size. Body size is an important determinant of blood pressure in children, and blood pressure should be compared to normal values adjusted for age, gender, and height percentile. The blood pressure levels for the 90th percentiles of blood pressure for boys and girls age 1 to 17 years by percentiles of height are available in the Task Force Update.568,569 Table 162 presents an abbreviated listing of the age-appropriate 90th percentile of blood pressure according to height percentiles in girls 2 to 17 years of age, while Table 163 presents an abbreviated listing of the age-appropriate 90th percentile of blood pressure according to height percentiles in boys 2 to 17 years of age. To use these charts, the age of the child and the height percentile of the child is determined with standard growth charts, then the 90th percentile blood pressure for the age and height percentile of the child can be determined from the chart. For example, the 90th percentile SBP and DBP for a 6-year old girl whose height is at the 5th percentile would be 104 mm Hg and 67 mm Hg, respectively, while the upper limit of normal SBP and DBP for a 6-year old girl whose height is at the 95th percentile would be 110 mm Hg and 70 mm Hg, respectively. The 90th percentile SBP and DBP for a 14-year-old boy whose height is at the 5th percentile would be 120 mm Hg and 76 mm Hg, respectively, while the 90th percentile SBP and DBP for a 14-year-old boy whose height is at the 95th percentile would be 128 mm Hg and 80 mm Hg, respectively.
Blood pressure monitoring in children can be preformed at home by the parents or the child with standard blood pressure equipment. Similarly, blood pressure monitoring can be preformed in the school environment by school nurses.
As in adults, children with CKD have disturbances in circadian rhythms in blood pressure, and ambulatory blood pressure in children correlates better with end organ damage than clinic blood pressure (Strong). Children with CKD have altered patterns of blood pressure that make the diagnosis of hypertension in the normal clinic setting more difficult when relying on casual blood pressure measurements.570 The primary rhythm abnormality is a blunted sleep-related fall in blood pressure, that is, "nondipping," which is commonly associated with sleep-related hypertension. The abnormal patterns become more prevalent as GFR declines in dialysis patients571 and in kidney transplant recipients.572-574 It has been suggested575 that ambulatory blood pressure monitoring (ABPM) can aid in differentiating primary from secondary hypertension in children. A combination of daytime DBP load >25% and nocturnal SBP load of >50% was very specific for secondary hypertension in children.
One of the most valuable uses of ABPM in pediatrics is the prediction of CVD. CVD mortality is rare in children, although much more common in CKD patients than the general pediatric population. Thus, determination of more subtle hypertensive damage is critical to the assessment of effects of hypertension or therapy of hypertension in children. ABP has been shown to correlate with measures of LVH better than clinic blood pressure in CKD patients.563,576-578 The most common abnormality associated with CVD is the blunted sleep-related fall in blood pressure and sleep-related hypertension. However, the Work Group concluded that, while abnormal patterns of blood pressure have been identified by ABPM in children with CKD, there is insufficient evidence to recommend ABPM as a routine diagnostic tool or as a guide to blood pressure management in patients with CKD.
The prevalence of types of CKD and causes of hypertension in children differs considerably from those seen in adults (Strong). Children with CKD and high blood pressure should be investigated for the underlying cause of CKD and appropriate therapy should be initiated based upon the diagnosis.1 Diabetic kidney disease and hypertensive nephrosclerosis are uncommon in children, while obstructive uropathy with associated renal dysplasia is one of the most common causes of CKD in children.566,579,580 The most common cause of hypertension and CKD in children varies according to the age of the child (Table 164). CKD and hypertension in the school age child is more commonly caused by scarring of the kidneys, dysplasia, glomerulonephritis, obstructive nephropathy, and polycystic kidney disease, while hypertension in the neonate may be due to renal artery thrombosis, coarctation of the aorta, obstructive nephropathy, or bronchopulmonary dysplasia.566,569,580
Some types of CKD in children are associated with excessive loss of sodium and chloride (Strong). Lifestyle modifications in children consist of weight reduction, exercise, and dietary modifications, similar to those in adults. However, the type of CKD needs to be considered when initiating dietary modification, in particular, restriction of sodium chloride. Restriction of salt is appropriate in children with CKD associated with salt and water retention, but many patients with tubulointerstitial diseases, such as obstructive uropathy and associated renal dysplasia, are unable to conserve salt; restriction of sodium chloride in such patients is inappropriate.579 Therefore, the Work Group concluded that practitioners should consider the underlying cause of CKD before initiating dietary modifications in children.
Weight reduction results in lowering of SBP and DBP in obese children.581 In adolescents and school-aged children, exercise training has been shown to lower SBP and DBP.582-584
ACE inhibitors or ARBs may be preferred antihypertensive agents to slow the progression of CKD in children (Weak). Several studies have demonstrated a beneficial effect of antihypertensive therapy in children with CKD in lowering blood pressure. ACE inhibitors have been shown to be effective antihypertensive agents in children, and an ARB has been shown to effectively lower blood pressure and reduce proteinuria in children with CKD.585-588
However, very few studies have been performed to demonstrate that blood pressure management has an effect on kidney disease progression or CVD outcomes in children with CKD. Studies in children with CKD treated with ACE inhibitors have demonstrated a beneficial effect of therapy on proteinuria, and one study demonstrated that ACE inhibitor therapy in children with CKD resulted in reduced LVH.589-592 A study in adolescent diabetic patients and a study in children with CKD demonstrated that proteinuria decreased following the initiation of ACE inhibitor therapy.589,590 Similarly, a study using captopril therapy in children with CKD and hypertension demonstrated a reduction in LVH that correlated with the reduction in SBP.592 Based on these studies and on studies in the adult population, it was the opinion of the Work Group that it is reasonable to consider an ACE inhibitor, or an ARB if an ACE inhibitor cannot be used, as a preferred antihypertensive agent in children with CKD.
Safe and effective use of blood pressure medications in children with CKD requires adjustment of the dose according to age and weight (Strong). Numerous studies document variation in disposition and metabolism of drugs according to age and weight in children.568,593 For example, neonates are very sensitive to the effects of ACE inhibitors, and prolonged hypotension and adverse effects has been observed in neonates treated with doses of ACE inhibitors commonly used in older children.594,595 Similarly, use of ACE inhibitors in premature infants should be used with caution, since the RAS has been shown to play a role in renal development.596 Since nephrogenesis occurs after birth in premature infants, ACE inhibitors should be used with caution since their use may interfere with nephrogenesis as it occurs in utero.597 Therefore, the class of the antihypertensive agent and the dose of an antihypertensive agent in children with CKD should include consideration of the age of the child and should be adjusted for the patient’s weight.
There are insufficient data on the optimal level of blood pressure in children with CKD. Based on studies of children without kidney disease and the experience in CVD risk reduction in adults, the Work Group adopted the recommendations of the Task Force that target blood pressure should be less than the 90th percentile for normal values adjusted for age, gender, and height percentile. Based on studies in adults reviewed in Guideline 7, the Work Group considered that the blood pressure of children with CKD should be lower than the 90th percentile for age or less than 130/80 mm Hg, which ever is lower. The blood pressure goal of less than the 90th percentile for age, gender, and height has also been adopted by the British Renal Association.597a The Caring for Australians with Renal Impairment (CARI) concluded that there is no evidence concerning target blood pressure in children with kidney disease and that there are insufficient data to recommend different target blood pressures for different causes of kidney disease based on sex, age, or ethnicity of children.
Indications for diuretic therapy vary according to the type of CKD (Strong). Diuretic therapy is appropriate in children with CKD associated with salt and water retention. However, diuretic therapy is not appropriate in patients with tubulointerstitial disease associated with salt-wasting, such as obstructive uropathy and associated renal dysplasia.579
Because of the specialized nature of CKD and blood pressure management in children, a pediatric kidney disease specialist should be involved in their care, when possible (Weak). Care of the children with CKD and high blood pressure needs to take into consideration the multiple other complications of CKD including management of anemia, renal osteodystrophy, chronic acidosis, growth and development of the child, school attendance, and other psychosocial issues.579,580 Because of the complexity of these issues, blood pressure management in children with CKD should involve a specialist trained in such care.
Comparison to Other Guidelines
These guidelines are consistent with recommendations from the Task Force, British Renal Association, and Caring for Australians with Renal Impairment (CARI).
There are virtually no studies in children that evaluate the effect of antihypertensive therapy on progression of CKD or the incidence of CVD. Multiple studies demonstrate that antihypertensive therapy is effective in lowering blood pressure in children and some studies demonstrate that antihypertensive therapy with an ACE inhibitor is effective in reducing proteinuria. Thus, the recommendations in this guideline are based upon studies in adults and studies in children using surrogate markers.
Accurate measurement of blood pressure in children requires the appropriate equipment and experience in the technique of blood pressure measurement in children. Antihypertensive therapy should be coordinated with other therapies for CKD and CVD risk reduction, including monitoring height and weight to assess growth and development and prevention, detection, evaluation, and treatment of obesity.
Studies to investigate the role of blood pressure management in children with CKD on progression of CKD and CVD need to be undertaken so that appropriate recommendations can be formulated. There is a major lack of studies to address the role of adequate blood pressure management in children with CKD, on progression of kidney disease, and on CVD. While studies in adults demonstrate that ACE inhibitors and ARBs are preferred antihypertensive agents in retarding the progression of CKD, no such studies exist in children. It is important to recognize that children are unique and that studies are required to assess the safety and efficacy of these and other antihypertensive agents on the progression of kidney disease and on somatic and kidney growth. Further studies of hypertension in CKD in children should include ABPM. It is a valuable clinical tool that can provide additional information about the alterations in blood pressure patterns observed in CKD and the prediction of CVD.