Antihypertensive therapy must take into consideration the patient’s perception of the health-care provider’s advice and prescriptions, factors that may influence self-management behaviors, and the likelihood that the patient will adhere to recommendations.
5.1 Self-management principles should be incorporated into the treatment plan (B).
5.2 Patient and family education about antihypertensive therapy should be culturally sensitive, sensitive to economic considerations, and based on the patient’s level of understanding (B).
5.3 All patients should be assessed for barriers to adherence and self-management (B), and referred for further counseling as needed (to a nurse practitioner, registered nurse, registered dietitian, masters prepared social worker, pharmacist, physician assistant, or other professional) (C).
The success of strategies for blood pressure management will ultimately depend upon patient self-management, or the ability and willingness of the patient to change and maintain certain behaviors. Behavior changes are likely to include the following: alterations in lifestyle to reduce the risk of disease (eg, diet, exercise, smoking cessation, limiting alcohol consumption); adherence to medication regimens; self-monitoring of blood pressure; and adherence to plans for medical follow-up. It is well documented in the scientific literature that adherence to professional advice is typically poor. Thus, it is not realistic simply to give advice about lifestyle behaviors or prescribe a medical treatment regimen and expect that the patient will adhere.
Framework and Definitions
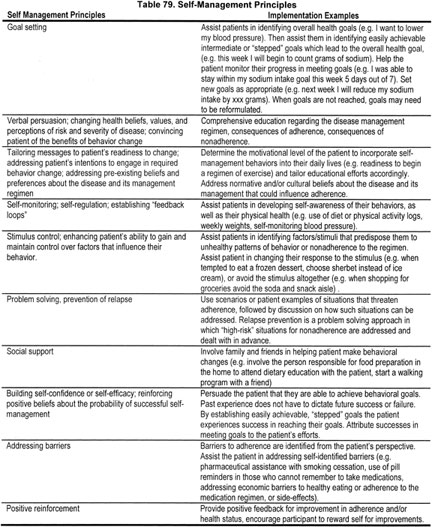
Self-management is a theory-based approach to health care that recognizes the central role played by the patient in health promotion, disease prevention, and successful management of illness. Self-management principles and implementation examples, shown in Table 79, are derived from a variety of theoretical frameworks pertaining to health behavior change and maintenance.214 Adherence refers to correctly following the treatment regimen. A culturally sensitive medical management plan is one that takes into consideration the values and practices of the patient’s reference group (eg, ethnicity or religion).
Self-management for CKD includes more than antihypertensive therapy. Antihypertensive therapy must be coordinated with other treatments to slow progression of kidney disease and reduce CVD risk, such as smoking cessation, lipid-lowering therapy, management of diabetes, and other life-style modifications.
The concepts discussed in this section are relevant to children and adults. Children require additional considerations that vary depending on age and family situation. Educational efforts must be directed to helping parents or guardians and the child to manage CKD.
Strength of Evidence
There is need for alternative approaches to traditional education regarding hypertension management (Strong). Nonadherence to medical management recommendations is a barrier to blood pressure control.215-220 Studies show that only 30% to 39% of hypertensive patients achieve adequate blood pressure control.215-218 Several reports indicate that inadequate patient adherence to the medical management regimen is one of the most important factors in uncontrolled hypertension.219-222
Recent studies regarding nonadherence to the hypertension management regimen tend to focus on medications. These studies show that as many as 65% of patients quit taking their medication223-228, and many take a dose that is below the therapeutic range.228 Thus, medication self-management and factors that contribute to nonadherence should be regularly addressed in all patient encounters.
Several controlled trials have also demonstrated that lifestyle changes can prevent the development of hypertension and that blood pressure can be effectively lowered by weight loss in combination with sodium restriction. However, the literature shows that long-term maintenance of blood pressure control is difficult to achieve using these behavioral approaches.229-233 A meta-analysis of 28 controlled trials in which low-sodium diets were prescribed for hypertensive patients showed the resulting reduction in DBP to be nonsignificant.234 As a result, some may conclude that it is more difficult to motivate patients to change their diet than it is to have them take medications.221 However, adherence to the medication regimen is also complicated, and promoting healthy lifestyle change should not be abandoned simply because behavior change is difficult to achieve. Although blood pressure control with diet alone diminishes over time, at 29 months 38% of patients were able to maintain adequate control without medication in one study.229 This is similar to the rate of control that is achieved in the general population on medication alone.214-216
Self-management strategies can improve adherence (Moderately Strong). Self-management is a relatively new paradigm for chronic disease management. While traditional patient education provides information and technical skills, self-management teaches problem-solving skills.235 The new emphasis on self-management highlights the growing recognition of the central role played by the patient in preventing and managing illness. A self-management program for 489 chronically ill patients in the Kaiser Permanente system resulted in improved health behaviors and health status.236,237 Furthermore, there is growing evidence from controlled trials that self-management approaches are more effective than information-only education in improving clinical outcomes, may reduce costs, and may soon become an integral part of high-quality primary care.235
The behavioral literature provides some guidance for incorporating self-management strategies into the medical management regimen. Intervention approaches have been shown to be useful in modifying dietary intake.238 The cornerstone of all dietary interventions is nutritional education, often dietitian-led individual or group sessions that address what foods should be avoided and consumed, how to modify recipes, and how to shop. Tailoring educational messages to patients’ psychological readiness to make dietary changes may be helpful in planning the approach to patients. Self-monitoring of dietary intake is an essential component of programs to promote dietary change, with patients tracking their intake of certain macronutrients such as sodium or saturated fat. Early in the dietary intervention, stimulus control may be employed in which patients identify and try to avoid cues (settings or situations) that result in unhealthy eating patterns, or attempt to alter their response to those cues. Helping patients problem-solve around high-risk situations in which adherence may be threatened is helpful, as is engaging their social support system to help make and maintain dietary changes. Programs that aim to increase patients’ confidence in their ability to make and maintain dietary change (referred to in the behavioral literature as self-efficacy) have also been shown to be effective in a number of dietary intervention studies. Finally, ongoing contact with an interventionist is helpful in maintaining dietary changes over the long term.238
One summary of RCTs testing dietary interventions for the control of hypertension found 15 studies comparing a weight-reducing diet to a nonintervention control group, 3 trials comparing a weight-reducing diet to antihypertensive drug therapy plus usual diet, and 5 trials comparing a weight-reducing diet to a low sodium/high potassium diet.239 The outcomes addressed in the trials included effect on blood pressure, relapse rate in individuals among whom antihypertensive medications had been withdrawn, or lowering of the dose of antihypertensive medication. The reviewers concluded that obese, hypertensive patients can lose weight when a structured, calorie-restricted diet and clinician follow-up are employed. Data from 7 of the trials suggest that a weight-reducing diet can result in blood pressure improvements. However, it is not clear in reviewing these studies the extent to which self-management strategies were used in the various interventions, or whether the use of self-management approaches resulted in better adherence or outcomes.
In terms of adherence to medication regimens, strategies to increase medication adherence in the elderly—which also appear to have application to hypertensive patients in general—have been published.240 First, a detailed medication history is essential on every patient. This should include prescription and over-the-counter medications, dosages, schedule, side-effects, and problems the patient experiences in taking medications. Education of the patient in terms of the disease, the benefits of treatment, and the consequences of nontreatment is obviously essential. Simplification of the medication regimen, when possible, to once or twice daily dosing can enhance adherence to the medication regimen. Aids (eg, charts, pill boxes, timed alarms) may be helpful in reminding patients to self-administer medications. Establishing self-medication routines (in which medication is paired with another regular activity such as morning coffee or brushing one’s teeth at night) are also useful, as is involving support persons in encouraging adherence. Older age and impaired cognitive function are independent predictors of poor hypertension control.218,241 Thus, regular assessment of the medication regimen is especially important in the elderly to assure their continued emotional, functional, cognitive, and visual capacity to adhere to the medication regimen.240
In a comprehensive review of RCTs of a variety of interventions for assisting patients in adhering to their medication regimens,242 33 controlled trials were identified, covering treatment regimens for a variety of disorders. In general, the reviewers found that for long-term medication regimens (eg, the hypertension medication regimen), the most successful strategies involved a combination of approaches including counseling, reminders, self-monitoring with feedback, and supportive care. Seven controlled trials testing adherence enhancement interventions for antihypertensive medications were reviewed in this report242 and are summarized in Table 80.
In a recent matched controlled study of a psychoeducational program for reducing risk associated with CVD, patients with kidney failure were exposed to a multifaceted intervention which included some self-management aspects including education, self-monitoring, and social support. Thirty days postintervention, the intervention group had a statistically greater proportion of participants who experienced a 5 mm Hg or more decline in their blood pressure.249a
Effective education is crucial for the successful prevention and management of hypertension (Table 81) (Strong). Patients must understand their level of risk, the condition they have, what they need to do to prevent or treat their illness, and the consequences of nonadherence. Patients with hypertension are thought to be at particular risk of nonadherence to the medication regimen because they are generally asymptomatic. In fact, researchers have shown that hypertensive patients with concurrent cardiovascular disease, in general,250 and angina, in particular,218 have better control over their disease. Lack of knowledge of target blood pressure has also been shown to be an independent predictor of poorly controlled blood pressure.218 Thus, knowledge of the asymptomatic nature of the disease and target blood pressure appear to be important for management of hypertension. Another important component of the education regimen is communication with the patient that adverse events should be reported, and can be dealt with by adjusting medications. In particular, sexual dysfunction in hypertensive men has been implicated as a cause of medication nonadherence.251 In a qualitative study, nonadherence was often an active decision that was based on misunderstanding of the condition (eg, hypertension is an intermittent condition, or only needed to be treated when symptomatic), general disapproval of taking medications, and a desire to minimize adverse effects. Those patients who were considering nonadherence and communicated this to their physician received further explanations and dosage adjustments or changes in medications, which is likely to result in better adherence, improved outcome, and better patient satisfaction.252
Educating patients about dietary regimens is complicated, requiring that patients learn about common sources of certain macronutrients such as sodium and fat, as well as how to monitor the intake of those nutrients on an ongoing basis. Educating patients about medications is similarly challenging. A series of studies show that patients recall only about 50% of what they are told by their physicians.253 Lack of information and inadequate instructions are major contributors to medication nonadherence. When explanations are couched in medical terminology that is unfamiliar, people are less likely to follow through with the prescribed regimen.240 Educational efforts must take into consideration patient beliefs regarding the nature and cause of their illness, and beliefs and understanding regarding the treatment regimen. For example, in a prospective survey of 102 patients, those who believed that they had personal control over their hypertension were more likely to be nonadherent to their treatment regimen.224
Cultural factors play an important role in the manner in which patients adhere to the hypertension management regimen (Strong). Hypertension is more common among African-Americans than Caucasians. African-American males with hypertension are particularly at risk because they often receive less treatment and, when they do, are less likely to adhere to the treatment regimen.254 Exploration of the beliefs about hypertension in low- to middle-income African-American individuals showed that predominant beliefs diverged sharply from current medical understanding of the disease. Respondents demonstrated a lack of understanding about the etiology of the disease. Many were unaware that persons with elevated blood pressure may be asymptomatic, and many felt that hypertension could be treated effectively with home remedies.255
Also, fewer hypertensive adult Hispanics use medication to control their blood pressure than do white or black adults, even after controlling for insurance, socioeconomic status, adverse health orientations, and habits. Culturally sensitive educational programs and services are needed to educate Hispanics about the importance of taking medication and making lifestyle changes to control their hypertension.256
Use of native healers by American Indians may influence self-care. In a study of 300 Navajo patients seen through the Indian Health Service in New Mexico, 62% reported having relied upon native healers, 39% on a regular basis. However, although use of native healers for medical conditions was common, patients rarely perceived any conflict between the native healer and conventional medicine.257
In providing services or programs to minority populations, it is important to consider the impact that discrimination and prior experience with the health care system may have on health-seeking behaviors and adherence to the prescribed regimen. Talking with minority groups (eg, in focus groups or with individual patients) about approaches being considered may be helpful in developing a successful service or treatment. Where dietary changes are required, it is essential to consider the inclusion of ethnic foods in recommendations for reducing sodium or fat. Although it is not always possible, including health-care professionals who are familiar with the patients’ language and culture is helpful in building rapport and trust. Addressing the cultural beliefs of the patient regarding the health-care system, in general, and dietary and medication prescriptions, in particular, are essential to their success.258
Although there is general recognition that cultural factors may influence adherence to the disease management regimen, research regarding the best approaches for promoting self-management among minority populations is very limited.
Overcoming barriers to adherence and self-management can improve blood pressure control (Moderately Strong). Nonadherence has been found to be related to a variety of potentially modifiable factors, as shown in Table 82. Addressing these barriers is essential to the success of the treatment regimen. Drug side-effects seem to be a large factor in discontinuation of antihypertensives. In a Finnish study, 68% of participants experienced adverse drug effects that resulted in 21% of female respondents and 31% of male respondents modifying their drug dose. Further analyses demonstrated that patients experiencing problems with their medication were nearly five times more likely to modify their dose, and that patients experiencing side-effects were twice as likely not to reach their blood pressure goal.259 In a US study, drug side-effects were found to be an independent predictor of poor hypertension control.218
Unfortunately, the side-effects of antihyper!-!tensives may go undetected by physicians. It has been demonstrated that while 69% of patients report having side-effects to their medications, their physicians estimate the rates to be only 10% to 20%, depending on the class of drug used.260
Occurrence of side-effects may be related to the class of drug prescribed. Two large, retrospective studies using medication databases show drug classification to be related to persistence in medication taking behavior. Both studies demonstrated that ARBs have the highest adherence, followed by ACE inhibitors, beta-blockers, calcium-channel blockers, and then diuretics.261,262 Combination therapy with low doses of two or more drugs has shown promise in enhancing adherence, because of the lower dosages (and, thus, fewer side-effects) of drugs required.263,264 It has been suggested that physicians could reduce the rate of adverse drug effects in elderly and frail patients by relying on JNC guidelines for initial dosing of such patients, rather than the more common practice of relying on dosing recommendations from the Physicians’ Desk Reference.265
The complexity of the management regimen is related to patient adherence.218 Hypertensive patients required to take only one pill a day were more adherent to the drug regimen than patients having to take medications twice a day.266,267 Similarly, in a meta-analysis of trials involving antihypertensives (including 8 studies and 11,485 observations), there was better adherence with once-daily dosing than either twice-daily or more frequent dosing regimens.268
Medication cost may influence patient adherence to the medication regimen. In one study, 14% of rural elders living in North Carolina reported having great difficulty paying for their medications and, as a result, 44% of patients took fewer medications or smaller doses than prescribed by their physician.269 Cost also appears to be a predictor of hypertension control in indigent, inner-city hypertensive patients.270 Also, depression is well known to be a factor for nonadherence in a variety of patient populations.271
Adherence in children is obviously a function of parental factors, particularly in younger patients. Although no reports were found in the literature regarding pediatric adherence to the hypertension regimen per se, pediatric adherence to medical follow-up visits has been examined. Nonadherence has been found to be related to lower socioeconomic status,272,273 transportation issues, being the child of a single parent,252 seriousness of the child’s illness,274 ethnicity, and insurance type.275 It is likely that other factors discussed above that interfere with adult adherence will also influence pediatric adherence. Educational efforts must be used to help both the parent or guardian and child manage hypertension in CKD. Further discussion is included in Guideline 13.
Low literacy is also a barrier to successful self management of hypertension.275a Patients with low health literacy were less likely to recognize an abnormal blood pressure reading and lacked knowledge of the effects of dietary and lifestyle factors on blood pressure. In a matched controlled worksite health promotion program to reduce risk for cardiovascular disease, an educational intervention tailored to the needs of a low literacy population was successful in reducing systolic blood pressure.275b
Research that pertains to CKD and hypertension is limited. However, data obtained from other clinical populations can be extrapolated for use with the CKD population. Much research has been done in other clinical populations related to lifestyle modifications and behavioral factors that are implicated in an individual’s management of hypertension.
Management of CKD is complex. It is unrealistic to expect patients to make multiple, simultaneous, major lifestyle changes. Clinicians will need to establish priorities in helping patients manage their disease.
Treatment of hypertension is complex, requiring a regimen that includes one or more of the following: medications, dietary modification, exercise, weight loss, and smoking cessation as well as consideration of the patient’s ability to implement and maintain a self-care regimen. The current system of care delivery is not always conducive to comprehensive care.
Clinicians should also attempt to maintain a simplified dosing regimen. Many patients, particularly those with multiple comorbid conditions, must take multiple medications throughout the day, which may increase the probability of nonadherence. Antihypertensive regimens using combination agents may be more acceptable to patients.
Incorporation of behavioral strategies to enhance self-management optimally requires a multidisciplinary team effort (physician, nurse practitioner, registered nurse, registered dietitian, social worker, pharmacist, physician assistant, case manager, or other professionals).
Teaching self-management is time-consuming, requiring repeated contacts with health-care professionals for education, goal setting, teaching self-monitoring, teaching problem-solving skills, and evaluation of progress. Establishing and maintaining self-management behaviors will likely require multiple and ongoing contacts with members of the health-care team.
Assessment of dietary patterns and education of the patient in dietary modification is best accomplished by a registered dietitian.
Education of the patient regarding medications should include, at a minimum, the reason the medication is being prescribed, instruction regarding side-effects, importance of adherence, consequences of nonadherence, and signs or symptoms that should trigger a return call or visit to a health-care provider. If appropriate, the patient should be instructed that alternative medications are available if side-effects become unmanageable. All information should be relayed to the patient in lay terms.
Referral to other members of the team with appropriate expertise should be considered when encountering barriers to regimen adherence such as cost; cultural factors and cultural beliefs; misperceptions or misunderstandings regarding hypertension, its treatment, and the consequences of nonadherence; or apparent inability to take medications on a regular basis (ie, forgetfulness, or difficulty managing a complex medication regimen).
Aging of the population will require regular reassessment of the patient’s ability to independently manage the medical management regimen.
Development of culturally sensitive educational materials and services is necessary to assure adherence to medical recommendations, and requires time and resources that may be beyond the control of the individual clinician.
Financial issues should be discussed with patients and their families before prescribing antihypertensive drugs, particularly in poorer societies and in populations (eg, Medicare beneficiaries) in which medication reimbursement is not universal. A less expensive drug may need to be substituted for a "preferred" agent to ensure long-term adherence and blood pressure control. This may be necessary even when the less costly medication is not the most effective for a particular patient.
The approach to patients should be individualized, taking into consideration their culture, economic situation, knowledge and beliefs regarding the disease and treatment, response to medication (in particular, side-effects), their ability (emotional, functional, cognitive, visual) to adhere to the prescribed regimen, and changes in status over time. The clinician must recognize that patient adherence involves choice, and some patients may be unwilling to make behavioral changes that are necessary to control their disease.
It is necessary to establish optimal interventions that combine behavioral approaches with pharmacological therapies to reduce risk factors for hypertension. Particular attention must be paid to identifying which behavioral strategies are most effective in producing desired behavior change.
Research should be done with the CKD population that relates to behavioral factors implicated in an individual’s management of hypertension. This research should include lifestyle factors, such as obesity, alcohol, cigarette smoking, and inactivity; social and environmental variables, such as lack of social support, socioeconomic status, and ethnicity; and individual characteristics, such as personality and reaction to stress.
Research is needed regarding effective strategies for maintaining long-term adherence to self-care requirements for prevention and treatment of hypertension.
Research is needed regarding the most effective strategies for promoting self-management behavior in minority populations.
The effect of low-dose, combination therapy on adverse effects of medication and, in turn, medication adherence, should be examined.