The following sections have been prepared to ensure that the state of the art and science related to CVD includes novel concepts, therapeutic strategies, and emerging areas of pathophysiological and practical importance to the care of dialysis patients.
The reader will notice that the format of this section is different, reflecting its different perspective: namely, the relative lack of evidence on which to base plausible guideline statements. The evidence that does exist, and is cited in this section, is either completely in nondialysis populations, or is purely associative information, with no intervention in any population yet tested. Thus, it would be a problem to include guideline statements or recommendations.
Nonetheless, this section describes the current status of knowledge with respect to risk factors and biomarkers, and represents an overview of key areas for future clinical trials. The reader is encouraged to review this section, and examine his or her current understanding and practice within the context of these highlights.
The literature review has been conducted using the same systematic strategy as for the previous guidelines in this document. The reviews presented here have been thoughtfully constructed so that clinicians can adopt different practices based on them. However, for reasons cited above, the ability to truly recommend or suggest changes in practice would be premature at this time.
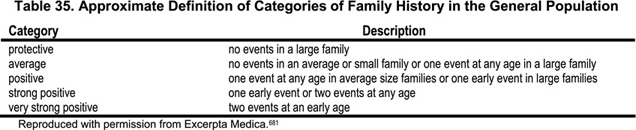
Family history (Table 35) is a strong predictor of CVD in the general population. It remains predictive for CVD even after correction for measured familial risk factors such as hypertension, cholesterol, obesity and diabetes.681—685 The familial aggregation of genes and shared environment strongly contribute to the increased frequency of a positive family history. A study of more than 120,000 families from the Health Family Tree Study and the Family Heart Study observed that 14% of the families that had a positive family history of CHD accounted for 72% of persons with early CHD (onset before age 55 for men and age 65 for women) and 48% of CHD at all ages. For strokes, 11% of families with a positive family history for stroke accounted for 86% of early strokes (before age 75) and 68% of all strokes.681 Family history collection is therefore a validated and inexpensive tool for family-based preventive medicine and medical research in the general population. However, there are no sufficiently powered studies in the CKD population that have investigated the value of this tool for risk assessment. Instead, several studies have examined a handful of candidate genes for CVD in dialysis patients.
The studies on candidate genes can be stratified into three groups. Two groups were already investigated in more than three patient cohorts and showed, in the majority of the studies, either a statistically significant association with CVD endpoints in dialysis patients (e.g., the apo(a) size polymorphism and the MTHFR polymorphism) or rejected such an association (ApoE and ACE polymorphism). The third group investigated candidates mostly in one cohort, and its results need to be confirmed by further studies.
Positive genetic association studies
Apo(a) size polymorphism
There is clear evidence that the apo(a) K-IV repeat polymorphism is associated with CVD in the general population, as well as in dialysis patients [see section on Lp(a) and apo(a) size polymorphism]. In brief, almost all studies found an association between LMW apo(a) phenotypes and atherosclerotic complications or total mortality (see Table 30).
677C→T polymorphism of the MTHFR enzymeA recent meta-analysis suggested that elevated homocysteine is, at most, a modest independent predictor of IHD and stroke in the general population686 Interestingly, moderate increases of homocysteine are reported in subjects who are carriers of a variant of the MTHFR gene. Those with a C-to-T substitution at position 677,687 have a reduced enzyme activity and about 20% higher homocysteine concentrations,688 especially when associated with low folate intake.689 A meta-analysis of all case-control observational studies from the general population revealed that the TT genotype was associated with 16% higher odds of CHD compared to individuals with the CC genotype.690 Five studies, mostly in HD patients, investigated this polymorphism in relation to various cardiovascular endpoints (Table 36).562,565,691–693 Four of the five studies found an association with outcome in univariate and/or in multivariate analysis562,691–693 which was not confirmed by another large study.565 Recently, a prospective follow-up study694 of earlier reported cross-sectional analysis in 459 patients was published.562 In contrast to the earlier findings, the prospective follow-up study did not show an association of this mutation with CVD.694 Taken together, it seems that there might exist an association between this mutation and CVD; however, the association is uncertain (Table 36).
Negative genetic association studies
Apolipoprotein E polymorphism
The ApoE polymorphism is significantly associated with intermediate phenotypes (e.g., concentrations of ApoE, ApoB, total and LDL cholesterol)695 and disease endpoints (coronary or peripheral atherosclerosis) in the general population.696,697 Only a few studies have investigated the ApoE polymorphism in relation to atherosclerosis in CKD patients and reported contrasting results.614,628,698,699 Thus, it appears that the ApoE polymorphism is not helpful for atherosclerosis risk stratification in dialysis patients (Table 37).
ACE polymorphism
A common ACE gene variant is known, with an insertion (I) or deletion (D) of a 287-bp fragment within intron 16. The D allele is associated with increased ACE levels and the polymorphism explains about half of the variation in plasma and tissue levels of ACE. An association between the DD genotype and CAD in the general population is controversial.700 In dialysis patients, most studies (especially the larger ones) did not reveal an association with clinical endpoints of cardiovascular disease (Table 38).691,701–707
Interesting candidates under investigation
The anti-inflammatory cytokine interleukin-10 (IL-10) counteracts the cascade of inflammatory factors leading to an acute-phase reaction.708 An interesting observation was recently reported for a polymorphism in the promoter of the IL-10 gene.709 This polymorphism, at position -1082, leads to low production of IL-10 (-1082A allele)710and the AA genotype is associated with a higher cardiovascular morbidity709 compared to the GG genotype. This reflects the reduced ability of the -1082 AA genotype to downregulate inflammatory processes as compared to the -1082 GG genotype.
Myeloperoxidase is an abundant enzyme in the production of free radicals. A functional genetic variant of this enzyme in position -463 (G→A) is associated with a lower myeloperoxidase expression and a lower prevalence of CVD in HD patients.711
The predictive value of family history of CVD should be investigated in patients with renal disease. Further large dialysis cohorts should investigate the value of Lp(a) concentrations and apo(a) phenotypes for risk assessment. This question should especially be addressed in PD patients as well as in various ethnicities. Arising candidate genes for CVD should be investigated in dialysis patients.
Family history and/or genetic testing are potential tools for CVD risk assessment or risk stratification, since they examine factors that cannot be changed by intervention. At the moment, insufficient data are available to determine whether family history is as predictive for CVD in dialysis patients as it is in the general population.
Laboratory testing for genetic factors may be considered for the apo(a) K-IV repeat polymorphism. This test can be done at any time, but the time of first presentation is preferred for an early stratification. Patients with LMW apo(a) phenotypes are exposed to an increased risk for mortality and CVD. Testing for MTHFR variants does not add significant information to that already obtained by measuring homocysteine levels. Further genetic testing is not indicated at the moment.
Patients with a positive family history and/or a LMW apo(a) phenotype may be considered high risk, and they may benefit from intensive risk factor assessment and interventional management.