This Guideline encompasses two parts: Guideline 9A, which is specific for CKD Stages 2-4, and Guideline 9B, which refers to CKD Stage 5.
Guideline 9A. Active Vitamin D Therapy in Patients with CKD Stages 2-4
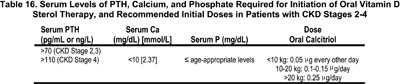
9A.1 In patients with CKD Stages 2-4, therapy with an active oral vitamin D sterol (calcitriol) should be initiated when serum levels of 25(OH)D are >30 ng/mL (75 nmol/L), and serum levels of PTH are above the target range for the CKD stage (see Table 3, Guideline 1). (EVIDENCE)
9A.1.a An active vitamin D sterol should be administered only in patients with serum levels of corrected total calcium <10 mg/dL (2.37 mmol/L) and serum levels of phosphorus less than age-appropriate upper limits (Table 16). (OPINION)
9A.2 After initiation of active vitamin D sterols, serum levels of calcium and phosphorus should be measured at least monthly for the first 3 months, and at least every 3 months thereafter. Serum PTH levels should be measured at least every 3 months. (OPINION)
9A.3 The dosage of active vitamin D sterols should be adjusted as follows:
9A.3.a If serum levels of PTH decrease to values below the target range for the CKD stage (Table 3, Guideline 1), active vitamin D sterol therapy should be held until serum levels of PTH increase to above the target range; treatment should then be resumed at half the previous dose of active vitamin D sterols. If the dosage is below a 0.25 µg capsule or 0.05 µg dose as liquid, alternate-day dosing should be used. (OPINION)
9A.3.b If serum levels of corrected total calcium exceed 10.2 mg/dL (2.37 mmol/L), active vitamin D sterol therapy should be held until serum calcium decreases to <9.8 mg/dL (2.37 mmol/L); treatment should then be resumed at half the previous dose. If the lowest daily dose of the active vitamin D sterol is being given, alternate-day dosing should be used. If the dosage is below a 0.25 µg capsule or 0.05 µg dose as liquid, alternate-day dosing should be used. (OPINION) See algorithm 2.
9A.3.c The dosage of active vitamin D sterols should be adjusted downward as follows: If serum levels of phosphorus increase to greater than age-appropriate upper limits, active vitamin D therapy should be held; the dose of phosphate binders should be increased or initiated until the levels of serum phosphorus decrease to age-appropriate levels; then, treatment at half the prior dose of active vitamin D sterol should be resumed. (OPINION)
9A.4 The dosage of active vitamin D sterols should be adjusted upward as follows: If serum levels of PTH fail to decrease by at least 30% after the initial 3 months of therapy, and the serum levels of calcium and phosphorus are within the target ranges based on CKD stage, the dose of active vitamin D sterols should be increased by 50%. Serum levels of PTH, calcium, and phosphorus must be measured monthly for 3 months thereafter.
Algorithm 2. Management of CKD Patients (Stages 2-4) with Active Vitamin D Sterols
In patients with CKD, 2° HPT occurs when the GFR declines to <75 mL/min/1.73 m2 (Stages 2-3). The administration of small doses of the active vitamin D sterol, calcitriol, can reduce the serum levels of PTH and may improve linear growth. With the use of low dosages of calcitriol, hyperparathyroidism can be suppressed without evidence of worsening of kidney function; however, careful monitoring of serum levels of calcium, phosphorus, and PTH is essential.
In adult CKD patients with GFR <60 mL/min/1.73 m2 (Stage 3), serum levels of PTH are increased.103,116,290,291 In such patients, bone biopsies show histomorphometric features of hyperparathyroid bone disease despite only modest elevations of PTH.10,292-294 Serum levels of 1,25(OH)2D3 are either normal or in the lower range of normal,103,116,290,291 despite the elevated PTH levels and serum levels of phosphorus that are often in the low range of normal.74,100,230 Normal 1,25(OH)2D3levels in the face of high levels of PTH are inappropriate and thus contribute to defective feedback suppression by 1,25(OH)2D3 of prePTH synthesis in the parathyroid glands, with a resultant increased secretion of PTH.295
In controlled trials in adult patients with Stage 3 CKD, the administration of oral calcitriol, 0.25 µg/day and occasionally up to 0.5 µg/daily,292,296 or of alfacalcidol, 0.25-0.5 µg daily10 were associated with lowering of PTH levels,294,296 improvement of histological features of hyperparathyroid bone disease,292,294,297 or an increase of BMD.296 Preliminary evidence also suggests that patients who had calcitriol therapy initiated when the creatinine clearance exceeded 30 mL/min/1.73 m2 (0.50 nmol/L/min/1.73 m2) had normal bone histology when they reached Stage 5 CKD and received a kidney transplant, while those whose treatment was started when kidney failure was more advanced were less likely to have normal bone histology when they reached end-stage kidney disease.298 Calcitriol deficiency may also contribute to growth retardation and bone disease in children with CKD. Indeed, treatment with daily doses of calcitriol (1,25-dihydroxyvitamin D3), has been reported to improve linear growth in small numbers of children with CKD Stages 2-4.299 Such findings provide the rationale for the routine administration of calcitriol to nearly all children with CKD. However, in other studies, enhanced growth velocity was not demonstrated on long-term follow-up and further studies have not shown that calcitriol consistently improves linear growth in children with CKD Stages 2-4.300 A more recent study demonstrated a direct relationship between changes in growth velocity and PTH levels in children with CKD Stages 2-3 treated with either daily or intermittent calcitriol therapy,301 similar to the findings reported in children with CKD Stage 5 and treated with peritoneal dialysis.302 Furthermore, more severe growth retardation was observed in those patients that developed adynamic bone after treatment with calcitriol was given intermittently, either orally or intraperitoneally.302 These results suggest that large doses of intermittent calcitriol therapy in conjunction with calcium-containing binders adversely affect epiphyseal growth plate chondrocytes activity, and thereby contribute to reduction in linear growth. On the other hand, others have described catch-up growth associated with PTH levels within the normal range in children with CKD Stages 2-3 treated with calcium supplements and low doses of 1-α-calcidol.303 Although the optimal PTH levels that are required to maximize growth remain to be defined, it may be prudent to maintain serum PTH according to the stage of CKD.
There has been concern about the safety of the use of vitamin D metabolites with regard to a possible adverse effect on kidney function. With the use of calcitriol in doses ≤0.25 µg/day and doses of alfacalcidol that were generally below 0.5 µg/day, the progressive loss of kidney function did not differ from observations in placebo-treated or control patients.10,292,294,297,304 In all CKD patients receiving vitamin D therapy, continued surveillance is needed, and hypercalcemia must be avoided. When calcitriol was given in doses of ≥0.5 µg/day, reductions of creatinine clearance were observed,305,306 although it is not certain that true GFR (inulin clearance) was affected.306,307 In CKD patients with serum levels of phosphorus greater than upper limits suggested by Guideline 4, dietary phosphorus restriction and/or phosphate binders should be employed and the serum phosphorus normalized before initiation of treatment with an active vitamin D sterol.
Each of the placebo-controlled trials of adult CKD patients with GFR of 20-60 mL/min/1.73 m2,10,292,297 and two studies without a placebo-control group293,294 have shown evidence of hyperparathyroid bone disease in a high fraction of baseline “control” bone biopsies. These abnormalities were common in the CKD patients recruited only on the basis of their impaired kidney function (reduced GFR or elevated serum creatinine levels) with the degree of elevation of pretreatment levels of PTH totally unknown.10,292,296,297 In each of the placebo-controlled trials, there was either no improvement or worsening10,292,297 of the features of hyperparathyroid bone disease in patients assigned to placebo therapy. Following treatment for 8, 12, or 24 months, an improvement of bone biopsy features was noted in the vitamin D-treated patients.10,292,293,297 Meta-analysis could not be done for these studies because one reported their data as mean ± SD,293 one reported medians and ranges,10 and another reported the fractions of patients who showed improvement or worsening of various histological features on bone biopsy.10 Another study was excluded because the number of subjects was too small (n < 10).297
The safety of calcitriol or alfacalcidol in CKD with moderately reduced kidney function is a matter of concern; however, the data from the placebo-controlled studies show no reduction of kidney function compared to placebo in patients entered into these trials and using relatively low doses.10,292,293,296,297 Should hypercalcemia develop during vitamin D treatment, particularly with higher doses, transient or even long-lasting deterioration of kidney function has been observed.308-310 With regard to the risk of producing “adynamic bone,” the placebo-controlled trial that included the largest number of bone biopsies failed to show any increase in the appearance of adynamic bone disease following treatment with alfacalcidol.10
The available evidence in adults is obtained from short-term studies and on a relatively small number of patients. Also, no data are available on the effect of the new vitamin D analogs, which are noted to be less hypercalcemic. Data in children with CKD Stages 2-4 are not available or very limited with respect to PTH and bone histology, or the effects of vitamin D sterol therapies.
It appears that the active vitamin D sterols are useful in the treatment of 2° HPT and high-turnover bone disease in early stages of CKD in adults. This provides a good therapeutic tool for the prevention and management of these two abnormalities in CKD patients, before these derangements advance and their treatment becomes more difficult. Attention should be paid to the beneficial effect on linear growth in reducing hyperparathyroid bone disease in CKD Stages 2-4 as well.
In children with CKD Stages 2-4, randomized, placebo-controlled trials of the extent and therapy of hyperparathyroid bone disease are warranted. In adults, further trials with longer-term treatment (≥24 months) in larger numbers of patients are needed to satisfy the concern about the safety of the therapy with vitamin D sterols. Trials with the newer vitamin D sterols, which may be less calcemic, will be of great interest. An ideal goal of such treatment would be to reduce serum levels of PTH with little or no change in serum levels of calcium. Studies should evaluate the effect on bone, in particular to ascertain whether improvement in bone mineral content or in histological features of hyperparathyroid bone disease could be achieved. Comparisons of newer vitamin D sterols with calcitriol, alfacalcidol, or even ergocalciferol, at 50,000 IU monthly, would be ideal. It is apparent that the ideal target for serum levels of PTH that should be achieved are not established, and biopsy evaluations in such trials with correlations between PTH or iPTH levels and skeletal findings would be ideal. Also, in the trials that have been published,10,294 it would be useful if the data were reanalyzed to evaluate the relationship between serum levels of PTH and the degree of parathyroid bone disease found on biopsy in relation to the degree of impairment of kidney function.
Guideline 9B. Active Vitamin D Therapy in Patients on Dialysis (CKD Stage 5)
9B.1 In patients with CKD Stage 5 and serum PTH levels >300 pg/mL, an active vitamin D sterol (calcitriol; see Table 17) should be administered to reduce the serum levels of PTH to a target range of 200-300 pg/mL. (EVIDENCE)
9B.2 The intermittent administration of calcitriol by intravenous or oral routes is more effective than daily oral calcitriol in lowering serum PTH levels. (EVIDENCE)
9B.3 When therapy with vitamin D sterols is initiated or the dose is increased, serum levels of calcium and phosphorus should be measured at least every 2 weeks for 1 month and then monthly thereafter. The serum PTH level should be measured monthly for at least 3 months and then at least every 3 months once target levels of PTH are achieved. (OPINION)
9B.4 For patients treated with peritoneal dialysis, initial oral doses of calcitriol (0.5-1.0 µg) can be given three times weekly. Alternatively, an equivalent lower dose of calcitriol (0.25 µg) can be administered daily. (OPINION)
9B.5 The dosage of active vitamin D sterols should be adjusted upward as follows: If serum levels of PTH fail to decrease by at least 30% after the initial 3 months of therapy, and the serum levels of calcium and phosphorus are within the target ranges based on CKD stage, increase the dose of active vitamin D sterols by 50%. Serum levels of PTH, calcium, and phosphorus must be measured monthly for 3 months thereafter.
9B.6 Treatment with active vitamin D sterols should be integrated with the changes in serum calcium, phosphorus, and PTH. A separate algorithm is shown for each of these three variables with suggested interventions based on the values obtained. (OPINION)
Patients with CKD who undergo dialysis have reduced serum levels of 1,25(OH)2D3. This leads to reduced intestinal absorption of calcium (thereby contributing to hypocalcemia) and impaired suppression of the parathyroid gene that initiates the synthesis of PTH. The result is 2° HPT that often progresses. Treatment with calcitriol or another active vitamin D sterol both reduces PTH secretion with resultant improvement of hyperparathyroid bone disease, and improves musculoskeletal symptoms, when these are present.
A major side-effect of vitamin D treatment is increased intestinal absorption of calcium and phosphorus; this can produce hypercalcemia and aggravate hyperphosphatemia. Treatment with active vitamin D sterols can also markedly lower serum levels of PTH and reduce bone formation strikingly; this can produce a condition with low bone turnover, termed adynamic bone disease. For these reasons, serum levels of calcium, phosphorus, and PTH must be monitored during vitamin D therapy, and vitamin D therapy adjusted accordingly (Algorithm 3, Algorithm 4, and Algorithm 5).
Treatment of 2° HPT in patients with CKD Stage 5 by oral or intravenous calcitriol, intravenous paricalcitol, oral or intravenous doxercalciferol, or oral or intravenous alfacalcidol can reduce the elevated levels of PTH,313-323 and may be useful to treat various clinical features of symptomatic 2° HPT.313,315,318 With such treatment, improved features of hyperparathyroid bone disease have been reported.314,315,324,325 Reductions of both serum total alkaline phosphatase and/or bone-specific alkaline phosphatase, consistent with a reduction of the elevated bone turnover state, have been shown during treatment with several of these vitamin D preparations.314-316,318,321,324,326
Although daily calcitriol therapy has been recommended for more than two decades to children with chronic renal disease, 2° HPT remains the predominant bone lesion in children treated with dialysis.22,23 Indeed, when patients with bone biopsy-proven high-turnover bone disease were followed for 1 year with calcitriol therapy given daily, bone lesions of hyperparathyroid bone disease persisted or progressed in the vast majority of the patients.311 Dosage regimens have generally ranged from 0.25-1.0 µg/day in such patients undergoing peritoneal dialysis.311
Over the last decade, the 1st PTH-IMA proved to be a reasonably reliable predictor of the different subtypes of renal osteodystrophy and it performed well in assessing the therapeutic response to active vitamin D sterols in patients with renal failure.22,23,327 In dialyzed children who are either untreated or are receiving small daily oral doses of calcitriol, PTH levels (measured by 1st PTH-IMA) of approximately three times the upper limit of normal generally correspond to normal BFRs. Levels >250-300 pg/mL are associated with bone biopsy evidence of 2° HPT, while values <150 pg/mL indicate an adynamic bone lesion.22
Similar values may not be applicable in dialyzed children receiving intermittent calcitriol therapy, since suppression of bone formation may develop despite persistently elevated PTH levels (measured by 1st PTH-IMA) in these patients.312 In patients treated with peritoneal dialysis, high-dose intermittent calcitriol therapy (both oral and intraperitoneal) results in marked decline in BFRs and development of the adynamic lesion in a substantial proportion of patients.312,328 Corresponding reductions in serum PTH levels were observed only in patients who received intraperitoneal doses of calcitriol, while serum PTH levels remained persistently elevated in those given intermittent oral doses of calcitriol, despite significant reductions in BFRs on repeat biopsy.312 Thus, the relationship between PTH and bone formation is disrupted during intermittent calcitriol therapy in children undergoing peritoneal dialysis.
The disparity between the histological and biochemical findings highlights the potential limitation of single PTH determinations to predict the skeletal manifestations of renal osteodystrophy, direct effects of calcitriol on osteoblastic activity and/or limitations of the current 1st PTH-IMA among the main potential factors.
In dialysis patients who have not received vitamin D, or those who have received daily oral calcitriol in doses lower than 0.5 µg/day, serum levels of PTH correlate with the degree of 2° HPT25,26,329; moreover, patients with PTH levels <400 pg/mL (44.0 pmol/L) and normal (or low) serum levels of calcium usually have only mild hyperparathyroidism.26,329 In these patients, the optimal control of serum phosphorus levels, combined with the use of calcium-based phosphate binders, may result in no further rise of serum PTH levels. When serum levels of PTH exceed 500-600 pg/mL (55.0 to 66.0 pmol/L), moderate or even severe hyperparathyroid bone disease is usual. When PTH levels exceed 1,000 pg/mL (110.0 pmol/L), larger doses of the vitamin D sterols are generally required.322,330-333 During treatment with intravenous calcitriol330 or oral doxercalciferol322 in prospective trials, there was evidence that larger doses are required for the treatment of patients with severe 2° HPT compared to patients with less severe hyperparathyroidism. Moreover, the suppression of serum levels of PTH in patients with severe hyperparathyroidism may require treatment for longer periods of time, e.g., more than 12-24 weeks.322,330-332 The reason for the delayed response of some patients is unclear; it might be related to upregulation of vitamin D receptors that are often reduced in the large nodular parathyroid glands in CKD Stage 5 patients with more severe 2° HPT.334
It is recommended that the dosage of a vitamin D sterol be adjusted in accordance with the severity of 2° HPT. The evidence that PTH levels correlate with the severity of bone disease in patients who have not received pulse-dose intravenous or oral calcitriol is quite good.25,26 However, the optimal doses of vitamin D sterols and the optimal serum levels of PTH that should be the target in patients who have received such therapy for longer than 6-12 months is less certain.
Several trials that were not placebo-controlled have shown the effectiveness of intermittent intravenous and intermittent oral calcitriol to suppress serum levels of PTH in patients undergoing hemodialysis,335,336 including some patients with severe hyperparathyroidism336-339; moreover, these results appeared more favorable than earlier experiences with daily oral dosing when reductions of dosage were commonly needed.340,341 However, the meta-analysis of four trials that compared intermittent intravenous calcitriol with oral calcitriol in randomized, controlled studies342,343 or crossover trials344,345 indicated that intravenous therapy was more effective than oral treatment (either daily or “pulse” treatment) for the suppression of PTH levels (Figure 7). There are certain qualifications about the trials combined for this meta-analysis: Two trials compared daily oral treatment with thrice weekly intravenous treatment343,345; in the trial that studied patients with the highest pretreatment PTH levels, the oral “group” was a combination of one group randomly assigned to intermittent treatment and a second group assigned to daily therapy.346 The degree of hyperparathyroidism was very mild in two trials, as the entry PTH levels averaged <400 pg/mL (44.0 pmol/L).343,344 In two trials that prospectively compared intermittent oral and intravenous calcitriol in patients with more severe hyperparathyroidism,347,348 the numbers of patients completing the study was too small (n < 10) to meet the criteria for the meta-analysis. In patients with more severe hyperparathyroidism (trials with intravenous calcitriol that adjusted the dosage upward if PTH levels were not suppressed), the use of calcitriol doses below 0.75-1.0 µg per treatment were often less effective in lowering PTH levels.330,349 Moreover, the earlier placebo-controlled trials with daily oral calcitriol found that patients could rarely tolerate daily doses of 0.5 µg per day without developing hypercalcemia.340,341
Fig 7. Meta-Analysis of Oral versus Intravenous Calcitriol on PTH Suppression
The results of oral trials with calcitriol that were not placebo-controlled lead to the conclusion that pulse or intermittent therapy yielded better results than were reported with daily therapy; meta-analysis of the results of three randomized, controlled trials that compared daily oral with intermittent oral calcitriol failed to show any superiority of intermittent therapy over daily therapy.317,346,350 Two of these studies317,350 had patients with only mild hyperparathyroidism, and few patients entered into treatment with PTH levels above 600 pg/mL (66.0 pmol/L). Despite randomization of treatment in one study,350 each of the five patients having pretreatment PTH levels >600 pg/mL (66.0 pmol/L) were assigned to intermittent therapy. In another study,346 the trial with the highest pretreatment PTH levels, the serum calcium levels were higher with daily than with intermittent therapy. Thus, conclusions about there being no difference depending on the frequency of dosing must be viewed with caution.
The major side-effects of active vitamin D sterols, including calcitriol and alfacalcidol, are increases in the serum levels of calcium and phosphorus, leading to hypercalcemia and worsening of hyperphosphatemia. These concerns have led to efforts to develop analogs of vitamin D which might have less calcemic and/or phosphatemic effects, while retaining efficacy for the suppression of high levels of PTH. 351,352 Several such analogs are now in clinical use. Paricalcitol and doxercalciferol are available in the United States, and maxicalcitol and falecalcitol are available in Asia.321,323,353,354 Extensive data in animals with normal kidney function and in experimental animals with uremia have demonstrated that maxicalcitol and paricalcitol are less calcemic and phosphatemic than calcitriol and yet retain effectiveness in suppressing PTH.355-357 Studies in vitamin D-deficient animals with doxercalciferol have demonstrated no difference in calcium or phosphorus absorption from the intestine and in changes in serum calcium compared to alfacalcidol, but doxercalciferol was associated with a decreased mortality in toxicology studies.358,359 Additional studies have shown that doxercalciferol is associated with less calciuria than alfacalcidol.360,361 Definitive quantitative data comparing these vitamin D sterols to calcitriol or to each other in controlled clinical trials are not available at the present time.
In placebo-controlled trials with calcitriol, alfacalcidol, paricalcitol, and doxercalciferol, there were increments of serum phosphorus during treatment,321,322,362-365 and analysis indicated no difference between the sterols regarding their effects on raising serum levels of phosphorus. Treatment with vitamin D should not be undertaken or continued if serum phosphorus levels exceed 6.5 mg/dL, because of this risk of further elevating serum phosphorus levels.
Another side-effect of intermittent treatment with an active vitamin D sterol is the appearance of subnormal bone formation, with “adynamic” or “aplastic” bone.328,366 In CKD Stage 5 patients who had not received pulse doses of calcitriol and had PTH levels <150 pg/mL (16.5 pmol/L), there was a high incidence of subnormal bone formation on bone biopsy, with adynamic or aplastic bone.26 When PTH levels are <65 pg/mL (7.15 pmol/L), the occurrence of adynamic bone is nearly universal.17,26 Mild hyperparathyroid bone disease may be preferable to adynamic bone because of the loss of the capacity of bone buffering for the added extracellular calcium207; this likely accounts for the increased risk of hypercalcemia in patients with adynamic bone.327,366 Also, there may be increased risk of vascular calcification in patients with biochemical features that are consistent with adynamic bone.84 In adolescents and young adults with CKD Stage 5, adynamic bone328 and even reduced linear growth occurred in association with intermittent calcitriol therapy when the PTH levels were reduced below 400-450 pg/mL (44.0-49.5 pmol/L).302 Reported observations of the development of adynamic bone in adult CKD Stage 5 patients in association with pulse therapy with calcitriol are limited to a small number367; however, there is little reason to believe that the bone of adults would not show the effects observed in pediatric-age patients.
When one elects to observe dialysis patients with PTH levels <600 pg/mL (66.0 pmol/L) without initiating vitamin D therapy, serial PTH levels should be monitored. If the levels show a progressive rise, treatment should be initiated.
Algorithm 3. Managing Vitamin D Sterols Based on Serum Calcium Levels
Algorithm 4. Managing Vitamin D Sterols Based on Serum Phosphorus Levels
Algorithm 5. Managing Vitamin D Sterols Based on PTH Levels in Children Not Receiving Growth Hormones
Many of the studies cited above with calcitriol and alfacalcidol that originated before 1980 lacked parallel control groups,313-316,318,324,325,368-370 and the assays for PTH were variable and some involved PTH fragments313-316,318 that are cleared by the kidney; thus, comparison with the current trials that utilize so-called “1st PTH-IMA” is not possible. Also, many patients in the early trials had “severe” and symptomatic bone disease, findings that have become more rare with better control of 2° HPT. With studies of the “newer” vitamin D sterols, such as falecalcitriol, paricalcitol, and doxercalciferol, there were often parallel controls.320-322,354 However, the severity of 2° HPT was mild to moderate, based on pretreatment serum levels of PTH, in most patients entered into trials with falecalcitriol320,354 or paricalcitol.321 For these reasons, comparison of data with the different vitamin D sterols must be regarded as tentative, particularly for patients with severe 2° HPT, defined as serum levels of PTH >1,200 pg/mL (132.0 pmol/L). Also, it is almost certain that such patients would be considered inappropriate for a long-term, placebo-controlled trial.
The conclusions that pulse intravenous therapy is better then pulse oral treatment must also be regarded as tentative; similarly, the conclusions that daily oral therapy is as effective as pulse oral therapy given two or three times a week may only apply to patients with mild 2° HPT for the reasons noted above.
Secondary hyperparathyroidism and hyperparathyroid high-turnover bone disease in CKD are treatable abnormalities with active vitamin D sterols. There are many of these sterols available and others are being developed. Since one of the side-effects of the therapy with these sterols is hypercalcemia, one would want to use a sterol effective in treatment of the bone disorder with little or no hypercalcemic effects.
Trials that compare different vitamin D sterols in CKD Stage 5 patients are needed. Also, prospective trials are needed to evaluate the effect of pulse-dose calcitriol or other vitamin D sterol on bone, with study of the relationship between serum levels of PTH and bone turnover using double tetracycline labeling, to assess a possibly important side-effect of vitamin D treatment. Moreover, little is known about the ideal target for serum levels of PTH during treatment with vitamin D. It is possible that the incidence of adynamic bone will increase substantially if vitamin D sterols are employed in patients who have only modest elevations of PTH levels. Studies are needed to examine the value of bone markers and to assess the relationship between the so-called “whole PTH molecule,” “1st PTH-IMA,” and bone histomorphometry during vitamin D treatment. Large studies that evaluate fracture rates should include data on previous vitamin D therapy in an effort to identify whether vitamin D treatment can modify the high incidence of fractures noted in CKD Stage 5 patients.