NKF KDOQI GUIDELINES
KDOQI Clinical Practice Guidelines for Cardiovascular Disease in Dialysis Patients
Section II. Guidelines on management of cardiovascular risk factors
Traditional risk factors—such as diabetes, hypertension, dyslipidemia—and those specific to dialysis patients (anemia and mineral metabolism abnormalities) require regular assessment and treatment as per current recommendations. The relative importance and weight of each of these risk factors in the dialysis population is not known and, in the absence of controlled trials in this population, current recommendations from existing organizations should be followed, with special consideration given to potential risks.
Furthermore, lifestyle issues such as smoking, physical activity, depression, and anxiety are the cornerstones of therapy as in the general population. The treatment options are often similar, but the impact of these factors is potentially more profound in dialysis patients. These factors are all discussed in this section. Special attention will be paid to the difference between the usual recommendations and those for dialysis patients.
Guideline 12: Blood Pressure
The management of blood pressure is an important component of CVD risk management for all aspects of CVD: CAD, cardiomyopathy, VHD, CBVD, and PVD. There are unique challenges in both the measurement and management of blood pressure in dialysis patients.
12.1 Measurement of blood pressure:
12.1a In patients who have undergone multiple surgical procedures for vascular accesses in both arms, blood pressure should be measured in the thighs or legs. However, health-care professionals should use appropriate cuff size and measure blood pressure only in the supine position. (B)
12.2 Predialysis and postdialysis blood pressure goals should be <140/90 mm Hg and <130/80 mm Hg, respectively. (C)
12.3 Management of blood pressure by adjustment of dry weight:
12.3a Management of hypertension in dialysis patients requires attention to both management of fluid status and adjustment of antihypertensive medications. This requires close collaboration among health-care providers. (B)
Excessive fluid accumulation between dialysis sessions should be managed with: (B)
- Education and regular counseling by dietitians
- Low sodium intake (2–3 g/day sodium intake)
- Increased ultrafiltration
- Longer dialysis
- More than 3 dialysis treatments per week
- Drugs that reduce salt appetite
12.4 Management of hypertension with drugs in dialysis patients:
12.4a Drugs that inhibit the renin-angiotensin system, such as ACE inhibitors or angiotensin II-receptor blockers should be preferred because they cause greater regression of LVH, reduce sympathetic nerve activity, reduce pulse wave velocity, may improve endothelial function, and may reduce oxidative stress. (C)
12.4b Antihypertensive drugs should be given preferentially at night, because it may reduce the nocturnal surge of blood pressure and minimize intradialytic hypotension, which may occur when drugs are taken the morning before a dialysis session. (C)
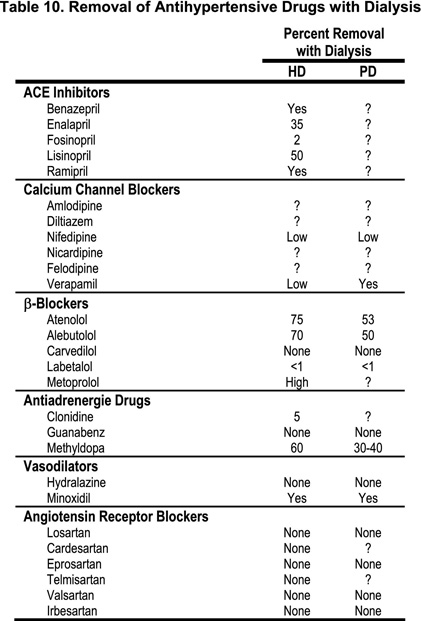
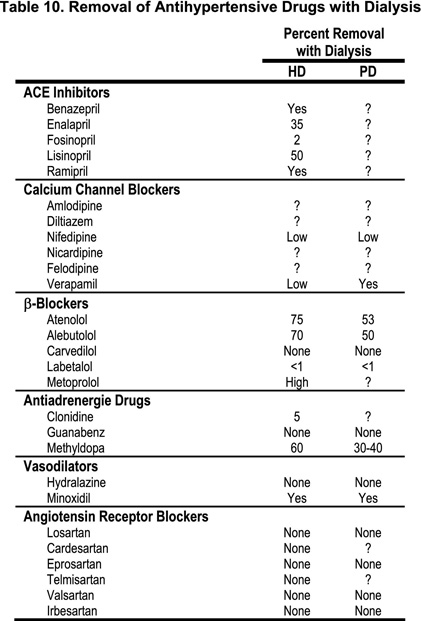
12.4c In patients with difficult-to-control hypertension, the dialyzability of antihypertensive medications should be considered (see Table 10).(C)
12.5 Determination and management of blood pressure in children should follow recommendations by The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents.50(C)
12.5a Optimal systolic and diastolic blood pressure should be <95% for age, gender and height. (B)
12.5b Management of hypertension on dialysis requires attention to fluid status and antihypertensive medications, minimizing intradialytic fluid accumulation by (C):
- education by dietitians every 3 months
- low salt intake (2 g/day sodium intake)
- increased ultrafiltration
- longer dialysis duration
- intradialytic sodium modeling to minimize intradialytic hypotension
- more than 3 dialysis treatments per week
- antihypertensives: consider if medications are cleared on dialysis.
Rationale
Definitions
Hypertension
The Seventh Report of the Joint National Committee for the Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC VII) has defined hypertension in adults in the general population as systolic blood pressure ≥140 mm Hg and diastolic blood pressure ≥90 mm Hg, and has defined normal blood pressure <120/80 mm Hg.170
Orthostatic hypotension
This is defined as a fall in blood pressure of at least 15 mm Hg systolic and 10 mm Hg diastolic after standing for at least 2 minutes. Although these levels of decline in blood pressure are usually associated with symptoms of cerebral anoxia, some patients may remain asymptomatic. By contrast, some patients may become symptomatic with lesser decreases in blood pressure. Thus, any quantitative definition of orthostatic hypotension may be misleading, and orthostatic hypotension should be diagnosed whenever the patient manifests symptoms of brain hypoxia upon standing. Heart rate variability during orthostasis is impaired in many CKD patients due to the coexistence of autonomic dysfunction. (Moderately Strong)
Blood pressure and CVD
Blood pressure and cardiovascular events
Hypertension is very prevalent among dialysis patients (50%-60%, when hypertension is defined as blood pressure >150/90 mm Hg for HD patients). The prevalence would be even higher if we were to use the JNC VII definitions above. In a study of 2,535 HD patients, only 14% were normotensive on no drugs and among the hypertensive patients, only 30% were controlled.175
Cardiovascular disease is the leading cause of death in patients receiving maintenance HD, especially in the first year of treatment. A history of long-lasting arterial hypertension is associated with an increase in cardiovascular deaths in these patients. Hypertension is the single most important predictor of coronary artery disease in uremic patients, even more so than cigarette smoking and hypertriglyceridemia.176 Although a direct relationship between levels of blood pressure and cardiovascular events has not been clearly established by controlled studies, hypertension in dialysis patients should be considered a major cardiovascular risk factor. The lack of a significant correlation between blood pressure and cardiovascular events in dialysis patients may be due to poor ventricular function, leading to lower blood pressure in some patients, when the follow-up duration is relatively short. (Weak)
It was found that, after adjusting for age, diabetes, IHD, hemoglobin and serum albumin, each 10 mm Hg rise in mean arterial blood pressure was independently associated with a progressive increase of concentric LVH, the development of de novo cardiac failure and de novo ischemic heart disease.177 Other studies however, have not shown a consistent association between blood pressure and subsequent mortality in the dialysis population. A “U-shaped” relationship between blood pressure and mortality was observed, with excess mortality risk in patients with the lowest and with the highest levels of blood pressure.178 Systolic blood pressure >180 mm Hg was associated with poor outcomes.179–181 It has been suggested that observations longer than 5 years are required to see the beneficial effect of blood pressure control. In a cohort study of 432 CKD patients (261 HD and 171 PD) followed prospectively for an average of 41 months, each 10 mm Hg rise in MAP increased the relative risk of LVH by 48% on follow-up echocardiography, increased the risk of de novo CHF by 44%, and the risk of de novo IHD by 39%. Interestingly, in this study low mean arterial pressure was independently associated with mortality.182(Weak)
A substantial body of evidence indicates that increased pulse pressure (PP), particularly in middle-aged and older subjects, is an independent predictor of risk of coronary heart disease, compared with mean arterial pressure (MAP). Pulse pressure represents the pressure increase during systole over diastolic blood pressure. It may be related to increased LV mass, decreased aortic compliance, and small-vessel remodeling,183–185 and is associated with reduced coronary vasodilator capacity.186 Reducing PP in hypertension may normalize small artery structure.187 In a recent study of a large cohort of nondiabetic patients on chronic HD, pulse pressure was found to be an independent predictor of total mortality,188 and was superior to systolic and diastolic blood pressure in predicting total mortality. Arterial stiffness can be measured noninvasively using the pulse wave velocity (PWV) technique, which is also an independent marker of cardiovascular risk in the general population.189 Epidemiological studies have shown that PWV is increased in CKD patients and it is an independent marker of cardiovascular risk in these patients.190 Aortic stiffness depends on the arterial wall structure and function, which can be influenced by blood pressure and aging.191 A recent prospective cohort study of 180 CKD patients on maintenance HD, followed for a mean duration of 52 ± 36 months, has shown that carotid pulse pressure and aortic PWV were strong independent predictors of all-cause (including cardiovascular) mortality. Brachial blood pressure, including pulse pressure, had no predictive value for mortality.192(Moderately Strong)
Pulse wave velocity frequently improves when blood pressure is reduced, particularly when ACE inhibitors193 or CCBs194 are used. In CKD patients, the failure of PWV to improve in response to decreased blood pressure is associated with worse cardiovascular outcome. Moreover, the use of ACE inhibitors may have a favorable effect on all-cause mortality and cardiovascular mortality that is independent of blood pressure changes.195(Weak)
Measurement of blood pressure in CKD patients
Methods
Blood pressure should be measured according to existing guidelines.196–198 The dialysis personnel should be trained and regularly retrained. The patient must be seated quietly for at least 5 minutes in a chair, with feet on the floor, and arm supported at heart level. Blood pressure should be measured at least 5 minutes before the needles for dialysis access are placed, as this may cause substantial stress in some patients. Blood pressure should also be measured in the standing position (at least 2 minutes) and the arm should be supported at heart level. Blood pressure should be measured both before and at the end of dialysis. Caffeine, exercise, and smoking should be avoided for at least 30 minutes prior to measurement. The auscultatory method of blood pressure measurement should be used and the disappearance of Korotkoff sounds should define diastolic blood pressure. Appropriate cuff size should be selected so that the cuff bladder encircles at least 80% of the arm. The equipment should be regularly inspected and validated considering that, in one study, automated blood pressure recordings overestimated blood pressure by 14/7 mm Hg before dialysis.199(Moderately Strong)
In patients who have undergone multiple surgeries for vascular accesses in both arms and blood pressure is technically not measurable in the arms, blood pressure could be measured in the thighs or legs. However, health-care professionals need to be properly trained, and should use appropriate cuff size and measure blood pressure only in the supine position. It must be kept in mind that blood pressure in the lower limb does not represent blood pressure measured in the arm. Systolic blood pressure and pulse pressure are amplified from the aorta towards peripheral arteries and amplification increases with the distance from the heart. Therefore, lower limb blood pressure is higher than brachial pressure. The difference is usually expressed as ankle-arm-pressure index. In young subjects the ankle pressure could be higher than arm pressure by as much as 30%. In older subjects, ankle and arm pressure tend to be the same. Therefore, the reference value for systolic blood pressure of 140 mm Hg is valid only for brachial pressure; the reference value for lower limb blood pressure is basically unknown. (Moderately Strong)
In patients with severe vascular calcifications, indirect measurements of blood pressure may be inaccurate. Intra-arterial measurements of blood pressure could provide true blood pressure, but this is not feasible in most dialysis units. (Weak)
Predialysis vs. postdialysis blood pressure. (Weak)
It is unclear which blood pressure reading should be used as the guide for therapy and control of CVD. Some data suggest that predialysis systolic blood pressure correlates best with LVH.200 Another report suggests that postdialysis blood pressure is the most representative of mean interdialytic blood pressure measured by ambulatory blood pressure monitoring (ABPM).201 Others have suggested that an average of predialysis and postdialysis blood pressure may be a better predictor of mean interdialysis blood pressure.202 In reality, neither is a particularly good predictor of interdialytic blood pressure.203 This issue is complicated by the known fall in blood pressure during dialysis in a large number (40%-50%) of patients, and by the fact that this fall is short-lived (12–24 hours). Thus, perhaps ABPM or self-measured home blood pressure are better markers of interdialytic blood pressure load; however, for practical and financial reasons, these tools cannot be applied to the totality of dialysis patients.
Circadian blood pressure variability and cardiovascular risk. (Weak)
Ambulatory blood pressure monitoring has improved the existing knowledge of the relationship between circadian variability of arterial blood pressure and end-organ damage. Normally, blood pressure tends to be the highest during the morning, and gradually decreases during the course of the day to reach the lowest levels at night.204–207 Some hypertensive patients (approximately 10%-25% of patients with essential hypertension) fail to manifest this normal nocturnal dipping of blood pressure, defined as a night-time blood pressure fall of >10%. These patients are called “nondippers,”208,209 whereas those with a normal circadian rhythm are called “dippers.” Among patients with advanced renal disease,210 and those on maintenance HD,211–214 the lack of diurnal variation in blood pressure and of the nocturnal dipping of blood pressure can affect as many as 74%-82% of patients. At times, in these patients, nocturnal blood pressure can be greater than blood pressure measured during the day. Because blood pressure is usually measured during the day, this may lead to the erroneous impression of good antihypertensive control.215 Using ABPM, it was observed that, in HD patients, blood pressure decreased after dialysis and during the first night, but by the next morning reached predialysis levels and it did not decrease during the second night.216
The phenomenon of nondipping can be improved with volume depletion and, perhaps, by dosing drugs at night rather than in the morning.
The mechanisms responsible for the abnormal circadian rhythm of blood pressure in patients with renal failure remain elusive. Autonomic dysfunction,217 reduced physical activity,218 sleep disordered breathing219,220 and volume overload221 have all been implicated. Since the phenomenon of nondipping is more prevalent among salt-sensitive patients with essential hypertension, and since this disturbance improves with salt restriction,222,223 one would predict that volume expansion would play a major role in HD patients. However, not all evidence supports a primary role of volume expansion in the phenomenon of blood pressure nondipping.224–226
The correlation between blood pressure measured in the physician’s office and cardiovascular end-points is usually weak. A large body of evidence from subjects with essential hypertension has shown that average 24-hour ambulatory blood pressure correlates with incident cardiovascular events227–231 better than office blood pressure. Ambulatory blood pressure monitoring has better long-term reproducibility than casual blood pressure measurement in HD patients.232
A relationship also seems to exist between the absence of nocturnal dipping of blood pressure and the severity of cardiovascular target organ damage.209 In a study of 57 treated hypertensive HD patients, it was observed that after an average follow-up of 34.4 ± 20.4 months and after adjusting for age, gender, and previous cardiovascular events, an elevated nocturnal and 24-hour PP, and low office diastolic blood pressure predict cardiovascular mortality.233 However, one has to remember that among HD patients there is a substantial day-to-day variability in the day-night blood pressure profile.212 Moreover, nocturnal blood pressure measurements predict cardiovascular outcome only in patients with reproducible blood pressure profiles.234
Pathophysiology of hypertension in dialysis patients
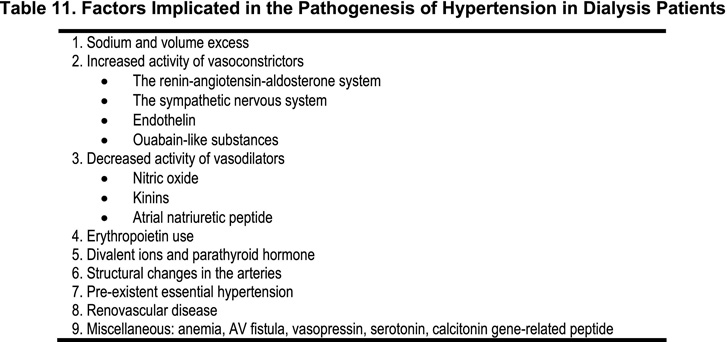
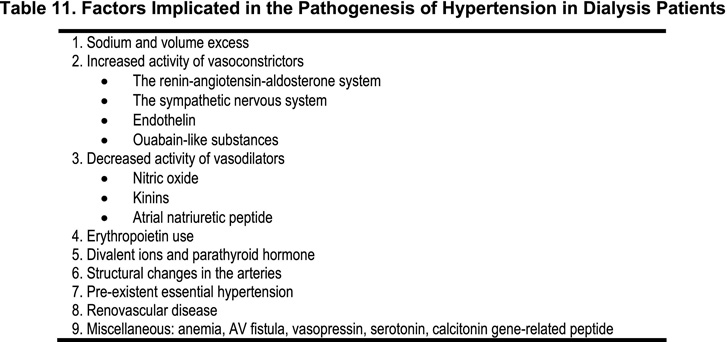
The pathogenesis of hypertension in CKD patients is complex and multifactorial. (Table 11).
Role of sodium and volume status. (Moderately Strong)
Excessive intravascular volume is a major pathogenic factor of hypertension in patients with CRF. However, the relationship between weight gain during two dialyses and hypertension is unclear. Some studies have established that volume gain affects interdialytic blood pressure, whereas other studies have not shown such a relationship.235
The HEMO study observed that volume status influenced both predialysis and postdialysis blood pressure.236 However, the intradialytic reduction in body weight (or interdialytic fluid gain) is helpful but insufficient to describe volume status and to predict blood pressure changes in HD patients.
The strongest evidence supporting a role for extracellular volume expansion derives from observations that, when excessive body fluids are removed with slow dialysis (8 hours × 3 times weekly) and “dry-weight” is achieved, blood pressure normalizes in more than 90% of dialysis-dependent patients.237 It is of interest that whilst the normalization of the extra-cellular volume was achieved in the first month of dialysis treatment, blood pressure continued to decrease for another 8 months, despite the withdrawal of antihypertensive medication. The reasons for long, slow dialysis achieving a more effective blood pressure control may be due to more effective control of the ECV expansion with a low rate of hypotension episodes. Moreover, dry weight is probably more difficult to achieve with short dialysis than with long, slow HD.
In dialysis patients, normal blood pressure can be achieved independently of the duration and dose of dialysis, provided that the control of the postdialysis ECV is adequate. Decreased ECF expansion is responsible for a significant portion of HTN control in HD regardless of modality, but variability in achieved ECV is significant.238
Longer and more frequent dialysis. (Weak)
Long, slow dialysis was shown to achieve a better blood pressure control and survival.239 Other investigators have also shown better regression of LVH with slow dialysis.240 Several studies have shown that short, daily HD treatment may be associated with a significant reduction of blood pressure, reduced use of antihypertensive medications, and lowered LV mass index.226,241,242 In other studies, daily dialysis (short diurnal or nocturnal) improved blood pressure control, but only short daily HD resulted in lower ECV.243
The improvement of blood pressure observed with short, daily HD is not necessarily due to less postdialysis ECFV. Unchanged postdialysis ECFV has been reported after the conversion to nocturnal HD and after excellent blood pressure control was achieved.244 Some have suggested that short daily HD may decrease SNS activity.
In patients who remain hypertensive despite intense ultrafiltration, sodium and volume excess may play only a secondary role. The lack of correlation between exchangeable sodium and/or extracellular volume and blood pressure in these patients supports this notion.245,246
Role of CAPD. (Weak)
Since CAPD allows for more consistent control of extracellular fluid volume than HD, it has been suggested that CAPD may provide better control of blood pressure than HD. Within 12 months of starting CAPD, between 40%-60% of hypertensive patients no longer required antihypertensive drugs.247
Better blood pressure control achieved during the first 2 months appears to be volume-related. After the initial 6 months of CAPD treatment, the sustained reduction in blood pressure does not correlate any longer with changes in volume and it is more likely related to removal of pressor hormones, although precise measurements of blood volume have not been performed.248 After 1–2 years of CAPD treatment, blood pressure may rise again, and so does the need for antihypertensive drugs, presumably due to fluid retention related to sclerosis of the peritoneum, decreased efficiency of the peritoneal membrane in removing fluids, and reduced kidney function.
Role of erythropoietin. (Moderately Strong)
The advent of recombinant human erythropoietin (rhEPO) has substantially improved the management of anemia and the quality of life in patients with chronic renal failure. However, increasing the hematocrit with rhEPO can lead to several adverse side effects, including worsening of hypertension.
During studies in dialysis and pre-phase III multicenter trials of rhEPO in dialysis patients, an increase in diastolic blood pressure of more than 10 mm Hg and/or a need to increase antihypertensive therapy occurred in 88 of 251 (35%) of previously hypertensive patients. A similar increase in blood pressure was noted in 31 of 71 (44%) of normotensive patients; in 32% of these patients, antihypertensive therapy had to be instituted.249,250 This adverse rise in blood pressure has not been noted in patients receiving rhEPO for other reasons, suggesting that renal disease may confer a particular susceptibility251 to the hypertensive action of rhEPO. The rise in blood pressure during rhEPO administration usually occurs within 2–16 weeks, although some patients may experience a rise in blood pressure several months after the initiation of therapy.
Patients who are at greater risk for developing hypertension during rhEPO therapy are those with severe anemia, those in whom anemia is corrected too rapidly, and those with pre-existing hypertension.
Management of blood pressure in dialysis patients
Target blood pressures
Despite the obvious importance of defining an ideal goal blood pressure for HD patients, this issue has not been resolved. According to JNC VII recommendations, normal blood pressure is <120/80 mm Hg.170 In patients with essential hypertension, receiving antihypertensive therapy, the recommended goal blood pressure is <135/85 mm Hg. This recommendation is largely based on the HOT study.252 The same study indicated that, in diabetic patients, the goal blood pressure should be set lower and should probably be below 130/80 mm Hg.
In patients with renal disease, particularly those with proteinuria greater than 1 g per 24 hours, a goal blood pressure of 125/75 mm Hg provides maximum protection against progression of renal disease.253 This recommendation, however, does not apply to African-Americans with hypertension and renal disease in whom no difference in progression of renal disease was observed between MAP of 107 and 92 mm Hg.254 Furthermore, these studies did not address the effect of different levels of blood pressure control on CVD.
It has been suggested that blood pressure of less than 150/90 mm Hg is a reasonable goal for most patients undergoing HD. The Work Group on chronic renal failure and renovascular hypertension, however, recommended a goal blood pressure of <130/85 mm Hg.255 In the only prospective study so far performed in the dialysis population, a blood pressure of 140/90 mm Hg minimized the occurrence of LVH and death.182
It is the opinion of this Work Group that, in HD patients, a reasonable goal is predialysis blood pressure <140/90 mm Hg (measured in the sitting position), provided there is no substantial orthostatic hypotension and these levels are not associated with substantial and symptomatic intradialytic hypotension. (Weak)
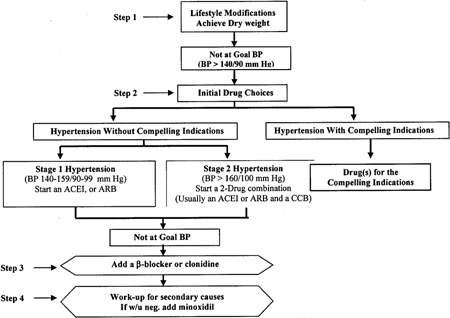
Treatment algorithm. (Weak)
The management of hypertension in dialysis patients is frequently challenging and it requires the knowledge of the pharmacokinetic and pharmacodynamic properties of all the agents used. We propose an algorithmic approach to the management of hypertension in dialysis patients (Fig 4).
Figure 4 - Hypertension Treatment Algorithm in Dialysis Patients
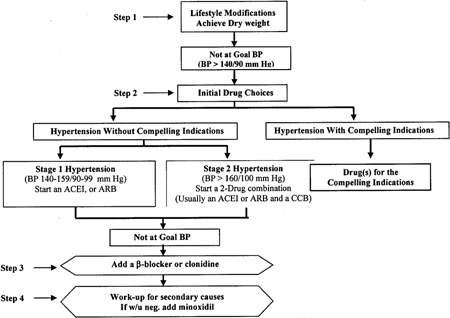
Lifestyle modifications should be an integral part of the management of hypertensive CKD patients. The importance of salt restriction should be continuously emphasized. Achievement of dry weight and reduction of ECFV should be pursued, although this is not easy to monitor or accomplish, and it may not be effective in every patient.
If those measures are unsuccessful (and frequently they are), antihypertensive drugs should be initiated. As a first line of treatment in the majority of patients, we propose the use of ACE inhibitors or ARBs. The latter also reduce LVH in HD patients, and may be more potent than ACE inhibitors.195,256–258 In an observational study, the use of an ACE inhibitor has been associated with decreased mortality in cohorts of CKD Stage 5 patients.259
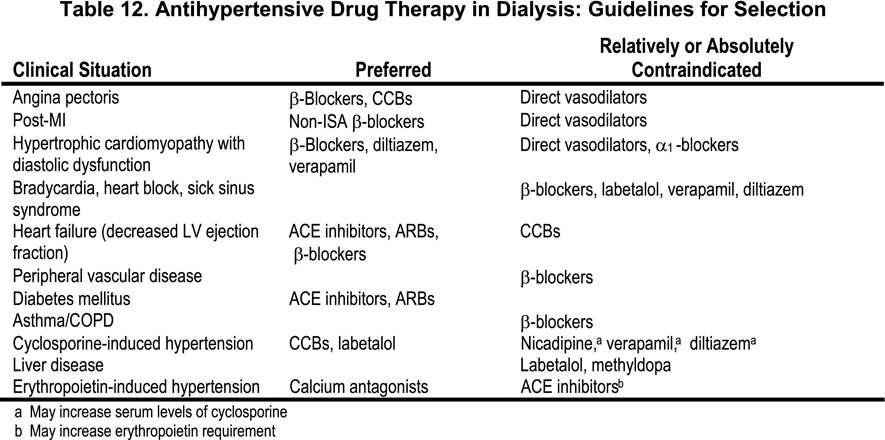
Table 12 describes some of the criteria to be used in the selection of antihypertensive drugs in dialysis patients based on compelling indications.
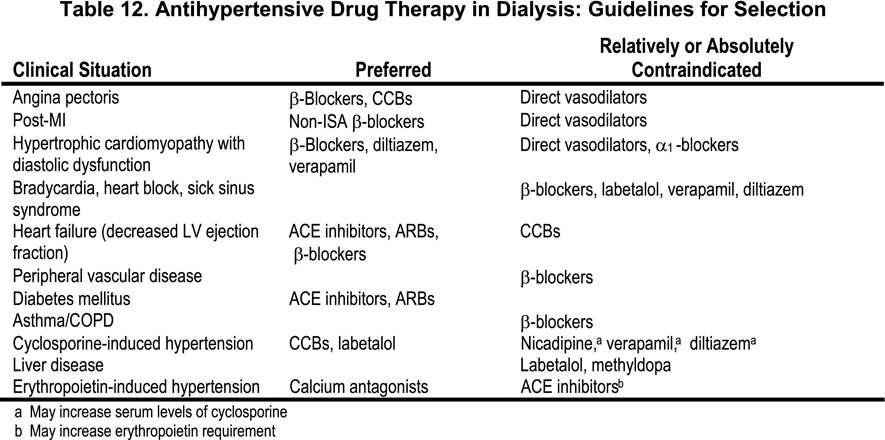
In patients with previous myocardial infarction or with well-established coronary artery disease, β-blockers should be preferred. Exposure to beta-blockers is associated with decreased mortality in CKD (see also Guideline 6).130 Calcium channel antagonists and anti-alpha-adrenergic drugs should be an integral part of the management of hypertension to achieve control if necessary. Observational studies suggest that CCBs are associated with decreased total and cardiovascular mortality.260 In the most severe forms of hypertension, multiple antihypertensive drugs are needed, including minoxidil. If full doses of one agent are ineffective, a second or a third drug should be added. If blood pressure is not controlled with dialysis and three antihypertensive agents of different classes, the patient should be evaluated for potential secondary causes of resistant hypertension. If no evident cause for resistant hypertension is found, and the patient remains hypertensive after a trial with minoxidil, one should consider treating the patient with continuous ambulatory peritoneal dialysis (CAPD). If CAPD proves ineffective, surgical or embolic nephrectomy should be considered.
Resistant hypertension. (Weak)
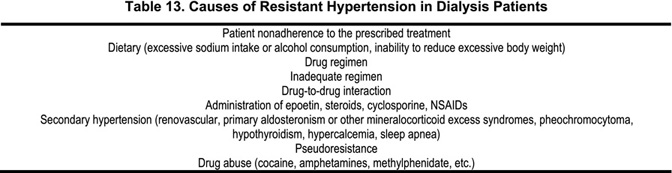
In dialysis patients, hypertension is considered resistant if blood pressure in a compliant patient remains above 140/90 mm Hg after achieving dry weight, and after an adequate and appropriate triple-drug regimen. In elderly patients with isolated systolic hypertension, resistant hypertension is defined as the failure of an adequate regimen to reduce systolic blood pressure to less than 140–150 mm Hg. The regimen should include nearly maximal doses of at least three different pharmacological agents selected from ACE inhibitors, calcium antagonists, β-blockers, antiadrenergic agents, or direct vasodilators, such as hydralazine or minoxidil.
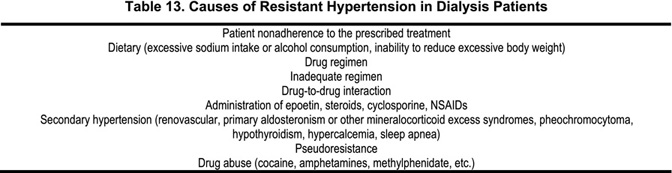
Several factors can cause resistant hypertension, including patient noncompliance, inadequate regime, drug-to-drug interactions, pseudoresistance, secondary hypertension, and unrecognized pressor mechanisms (Table 13).
Paradoxical rise of blood pressure during dialysis. (Weak)
Hypertension induced by HD is a topic that has received little attention. It occurs in a small number of patients during HD. The causes of this phenomenon have not been well worked out. Sometimes it is precipitated by removal of certain antihypertensive drugs during dialysis.
Hemodialysis reduces blood levels of some ACE inhibitors (enalapril, ramipril) but not others (benazepril, fosinopril, methyldopa, atenolol, acebutolol, nadolol, minoxidil and nitroprusside); by contrast, levels of clonidine, carvedilol, labetalol, CCBs and ARBs do not change significantly (see Table 12). At times, excessive volume depletion may result in hypertension rather than in hypotension. This has been attributed to excessive stimulation of the renin-angiotensin system precipitated by the decrease in blood volume. An alternative possibility, which has not been properly investigated, is that this might be the result of excessive activation of the sympathetic nervous system and resulting vasoconstriction.
In a recent study of seven patients with this characteristic, all with marked cardiac dilation, intense ultrafiltration reduced blood pressure and cardiac dilation and eliminated the paradoxical elevation of blood pressure during dialysis.261 The explanation of this phenomenon remains elusive.
Limitations
- One major limitation of these guidelines is the lack of large-scale clinical trials correlating levels of blood pressure with cardiovascular disease events. Particularly puzzling is the U-shaped relationship between systolic blood pressure and cardiovascular morbidity and mortality, and the apparent lack of high blood pressure effects on cardiovascular disease events until systolic blood pressure reaches approximately 180 mm Hg. The increase mortality in patients with lower blood pressure could be related to poor ventricular function. The lack of effects of blood pressure on cardiovascular events over a wide range of blood pressure between 100–180 mm Hg could be related to variable ventricular function, and to “survival bias,” whereby high-risk patients with higher blood pressure may not have survived to be entered into the study.
- Another limitation of these guidelines is related to the great variability of blood pressure with dialysis and the lack of firm criteria on definition of hypertension in this patient population.
- Another major limitation of these guidelines is the lack of controlled studies on the effect of different blood pressure goal and different therapeutic intervention on CVD events. Most of the recommendations are based on inference from studies performed in the general population with normal renal function. Other studies were performed in patients with various degrees of kidney disease, but not on dialysis therapy, and the outcomes were deterioration of renal function but not CVD.
Implementation Issues
- Measurement and recording of blood pressure is already implemented in most HD programs. Not all dialysis programs, however, routinely measure blood pressure in the sitting and upright position both before and after dialysis. Further definition and evaluation of the associated costs and benefits are required to determine the need for and implementation of 24-hour ABPM.
- Longer and/or more frequent short dialysis may be necessary to achieve control of blood pressure and fluid/volume status in many patients. However, current Medicare reimbursement policies, and patient resistance to more frequent and/or longer dialysis renders the implementation of these recommendations difficult.
Research recommendations
- More studies are necessary to better determine goal blood pressures in dialysis patients.
- Studies are needed to determine which antihypertensive drugs are best suited for dialysis patients.
- More studies are necessary to determine optimal dosing (dose and time of administration) of antihypertensive drugs in dialysis patients.
- Further studies are needed to ascertain the potential advantage of daily dialysis over dialysis performed 3 times weekly to achieve better blood pressure control and better cardiovascular outcomes.
Back to top | Main Page