In CKD Stages 2-4:
8.1 If serum PTH is above the target range for the stage of CKD (Table 3, Guideline 1) serum 25-hydroxyvitamin D should be measured. (EVIDENCE) Periodic assessment is warranted thereafter if dietary or lifestyle changes have occurred in the patient. (OPINION)
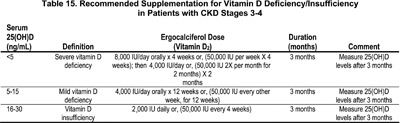
8.2 If the serum level of 25-hydroxyvitamin D is <30 ng/mL, supplementation with vitamin D2 (ergocalciferol) should be initiated (see Table 15). (OPINION)
8.3 Following initiation of vitamin D supplementation:
8.3.a The use of ergocalciferol therapy should be integrated with the serum calcium and phosphorus levels (Algorithm 1).
8.3.b The serum levels of corrected total calcium and phosphorus should be measured after 1 month, and then at least every 3 months. (OPINION)
8.3.c If the serum levels of corrected total calcium exceed 10.2 mg/dL (2.54 mmol/L), discontinue ergocalciferol therapy and all forms of vitamin D therapy. (OPINION)
8.3.d If the serum phosphorus exceeds the upper limits for age, initiate dietary phosphate restriction (see Guidelines 4 and 5) or, if hyperphosphatemia persists but the 25(OH)D is <30 ng/mL, initiate oral phosphate binder therapy. If the 25(OH)D is normal, discontinue vitamin D therapy. (OPINION)
8.3.e Once patients are replete with vitamin D, continued supplementation with a vitamin D-containing multivitamin preparation should be used with annual reassessment of serum levels of 25(OH)D, as should the continued assessment of corrected total calcium and phosphorus per stage of CKD (see Table 15). (OPINION)
In CKD Stage 5:
8.4 Therapy with an active vitamin D sterol (calcitriol) should be provided if the serum levels of PTH are >300 pg/mL. (OPINION) See Guideline 9.
Serum levels of 25(OH)D (not the levels of 1,25-dihydroxyvitamin D) are the measure of body stores of vitamin D. Recent studies in adolescents with normal kidney function in Boston have associated levels of 25(OH)D <25 ng/mL with considerable elevations of PTH. Levels of 25(OH)D are lower in young children with fractures, compared to an age-matched population without fractures. In individuals with normal kidney function over age 60, levels of 25-hydroxyvitamin D below the “normal” limit of 15 ng/mL, and also low to normal levels of 16-32 ng/mL, are both associated with increased PTH levels, reduced BMD, and increased rates of hip fracture. Such levels of reduced 25(OH)D are common in patients with CKD and GFR of 20-60 mL/min/1.73 m2, and in CKD patients undergoing dialysis. The prevention and treatment of vitamin D insufficiency in patients with CKD Stages 2-4 reduces the frequency and severity of 2° HPT. In patients with more advanced CKD (Stage 5) and in dialysis patients, it is not established that nutritional “replacement” with vitamin D (ergocalciferol or cholecalciferol) will be effective since the ability to generate adequate levels of 1,25(OH)2D3 is markedly reduced or absent. The role of reduced or absent levels of 25(OH)D remains controversial in the patient on recovery maintenance dialysis.
A reduction of serum 25(OH)D, the substrate for the kidney's generation of calcitriol [1,25(OH)2D3], produces 2° HPT in individuals with normal kidney function,254-256 and may aggravate 2° HPT in those with CKD and decreased kidney function.257,258 Severe manifestations of vitamin D deficiency, with osteomalacia and hypocalcemia, is rare unless 25(OH)D levels are <5 ng/mL (12 nmol/L); however, levels <30 ng/mL are indications of vitamin D “insufficiency”259 as manifested by significant elevations of serum levels of PTH. 259,260 Individuals with normal kidney function and with low “normal” 25(OH)D levels of 16-32 ng/mL (40-80 nmol/L) have lower BMD256; also, patients with hip fractures have lower 25(OH)D levels than age-matched patients without hip fracture.261 The only real disagreement in the literature is the upper range of 25(OH)D levels at which one does not encounter significant numbers of patients with 2° HPT,259 indicating that 25(OH)D should be maintained at higher levels.
Algorithm 1. Vitamin D Supplementation in CKD (Stages 2-4)
Studies of 25(OH)D levels in patients with CKD and varying degrees of decreased kidney function from five reports were reviewed.117,236,262,263 Among 63 non-nephrotic adult CKD patients, the median values of 25(OH)D levels in those with GFR of 60-90, 40-60, and 20-40 mL/min/1.73 m2 were 12, 19, and 18 ng/mL (30, 47, and 45 nmol/L), respectively.236 Obviously, a high fraction of these patients had levels <30 ng/mL (75 nmol/L) and many were <16 ng/mL (40 nmol/L). In a report of 76 CKD patients, 37 had CKD due to diabetes and 39 from other causes.117 The 25(OH)D level averaged 22.3 ± 9.4 ng/mL (56 ± 23 nmol/L) in nondiabetics and 11.4 ± 5.6 ng/mL (28 ± 14 nmol/L) in diabetic patients; in diabetics, serum albumin levels were lower and 76% had urinary protein concentrations >300 mg/dL, compared to 23% of nondiabetics.117 For the total group with GFR of 20-50 mL/min/1.73 m2, 47% had 25(OH)D levels <16 ng/mL (40 nmol/L) and 76% had 25(OH)D levels <26ng/mL (65 nmol/L). In these two studies,117, 236 serum 1,25(OH) 2D levels correlated with 25(OH)D levels [r = 0.51 236 and r = 0.47117], and P < 0.001. In the third study of the 19 CKD patients with GFR of 20-90 mL/min/1.73 m2, 79% had 25(OH)D levels <26 ng/mL (65 nmol/L) and 18% had 25(OH)D levels <16 pg/mL (0.4 nmol/L). In a U.S. study that included nine CKD patients with GFR of 12-60 mL/min/1.73 m2, 25(OH)D levels averaged 20 ± 6 ng/mL (50 ± 15 nmol/L) indicating that values were <30 ng/mL (75 nmol/L) in the majority of patients. Over a wide range of GFR, from 11-111 mL/min/1.73 m2, a large percentage were frankly vitamin D-deficient. Of those in CKD Stages 1-4, 86% had values <30 ng/mL. The findings that 1,25(OH)2D levels correlated with 25(OH)D levels in the three largest series117, 236 differ from observations in the population with normal kidney function, where 1,25(OH)2D levels are not dependent on the 25(OH)D levels, even in patients with vitamin D deficiency.264 The normal, highly efficient production of 1,25(OH)2D by the kidneys when the supply of 25(OH)D is markedly reduced is altered in CKD, and the data indicate that 1,25(OH)2D levels may be more dependent on the availability of 25(OH)D in CKD patients with impaired kidney function.265, 266
Patients with CKD or those who are dialysis-dependent are much more likely to have low levels of 25(OH)D in comparison to those with no kidney disease for several reasons: (a) many are inactive with reduced exposure to sunlight; (b) the ingestion of foods that are natural sources of vitamin D (fish, cream, milk, and butter) is likely to be lower than in the population with normal kidney function; and (c) serum 25(OH)D levels may be subnormal in CKD patients because the endogenous synthesis of vitamin D3 in the skin following identical exposure to sunlight is reduced in those with reduced GFR,267 in individuals over age 60,268 and in individuals with increased melanin content of the skin.269
The ingestion of a diet low in calcium content leads to greater conversion of 25(OH)D to calcitriol and the need for more vitamin D intake and/or production,270 and dietary calcium intake is frequently low in CKD patients.107 Furthermore, there is increased need for vitamin D in CKD patients with nephrotic-range proteinuria, because urinary losses of 25(OH)D and vitamin D-binding protein (DBP) are high.262,271 Kidney disease was found to be a major risk factor for low serum 25(OH)D levels in a population study of patients hospitalized in New England (with patients on dialysis excluded from the analysis).260
In countries such as the U.S. where many foods are supplemented with vitamin D, and in others such as Japan and the Scandinavian countries where fish intake is high, the incidence of vitamin D insufficiency is lower than in European countries of similar latitudes but where fish intake is low and vitamin D-supplemented foods are unavailable.259 Nonetheless, 14%-42% of apparently healthy individuals over age 60 in the U.S. had serum levels of 25(OH)D <24-25 ng/mL (60 or 62 nmol/L).272,273
In patients with Stage 5 CKD, there may be less need for vitamin D as a substrate for the renal 25-hydroxyvitamin D-1-α hydroxylase, as there is little or no generation of calcitriol by the kidneys. However, the data show that 25(OH)D levels below 15 ng/mL (37 nmol/L) are associated with a greater severity of 2° HPT even in CKD patients on dialysis.274 Nonetheless, the value of supplementation with ergocalciferol in these patients is less certain; although in dialysis-dependent patients, including anephric individuals, high doses of ergocalciferol or 25(OH)D can raise the serum levels of calcitriol.275-277
In patients with CKD and GFR of 20-60 mL/min/1.73 m2, nutritional vitamin D deficiency and insufficiency can both be prevented by supplementation with vitamin D2 (ergocalciferol) or vitamin D3 (cholecalciferol). If there is evidence of true vitamin D deficiency, this should be treated; the best available treatment is vitamin D2, although the doses needed are larger than those needed for vitamin D insufficiency. For the prevention of vitamin D deficiency, the RDA for vitamin D in children and adolescents remains at 400 IU, while in older individuals >60 years it is 800 IU. Little is known about the DRI of vitamin D for patients of any age with CKD.
There are problems with the dosage forms available. In the U.S., the only forms available are tablets of 400 IU (over the counter), and liquid forms (8,000 IU/mL) or capsules containing 50,000 IU, requiring a prescription. In individuals with normal kidney function, the recommended upper limit of vitamin D is 2,000 IU/day according to the Food and Nutrition Board, National Research Council, National Academy of Sciences.278,279 This dose can be achieved by giving one capsule (50,000 IU) once a month. 280,281 Dosage preparations of 10,000 IU of ergocalciferol have been given daily to French patients with advanced CKD for periods longer than 1 year, with no evidence of vitamin D overload or renal toxicity.282,283 Ergocalciferol vitamin D sterol may be safer than cholecalciferol, 284,285 although there are no controlled comparisons of cholecalciferol and ergocalciferol in humans, and the available commercial preparations employ ergocalciferol (as Calciferol™ or Drisdol™). Calcitriol or another 1 α -hydroxylated vitamin D sterol should not be used to treat vitamin D deficiency. In CKD Stages 1-4, when evidence of severe vitamin D deficiency is found, [25(OH)D levels <5 ng/mL (12 nmol/L)], rickets in the growing child, or osteomalacia, may be present. Treatment with ergocalciferol may be appropriate (see Table 15).281
There is strong evidence that vitamin D insufficiency, defined as 25(OH)D levels <27-32 ng/mL (67-80 nmol/L), is common in individuals >60 years in the U.S.,272,273 and many locations in Europe.286 Such low levels have clinical significance based on the finding of: a) the elevated serum levels of intact PTH as evidence of 2° HPT; and b) reduced BMD256 and higher rates of hip fracture compared to age-matched controls.287 The clinical significance of this is further demonstrated by data showing that supplementation with vitamin D, 800 IU/day, along with a modest dietary calcium supplement reduced hip fracture rate by 43% in a double-blinded, placebo-controlled trial.286,288 There have been reports in patients with CKD that suggest there may be adverse clinical consequences of suboptimal serum levels of 25(OH)D, including the finding that levels <15 ng/mL pose a major risk factor for the presence of severe 2° HPT (with radiographic abnormalities) in CKD patients on dialysis,274 although the dialysis dose provided to the patients in this study was suboptimal. A substantial prevalence of suboptimal levels of 25(OH)D in CKD patients with GFR of 20-60 mL/min/1.73 m2 has been identified in every study of such patients, but the number of individuals studied has been small. Regarding safety, the experience with ergocalciferol doses of 10,000 IU/day282,283 indicates a recommended dose of 1,000-2,000 IU/day would be safe.
In patients with GFR <20 mL/min/1.73 m2 and those requiring dialysis, there is no evidence that modest supplementation with ergocalciferol to raise serum 25(OH)D levels to 30-60 pg/mL (8.25-16.5 pmol/L) will increase the serum levels of 1,25(OH)2D (calcitriol) or lower the elevated serum levels of PTH. In CKD patients with higher GFR, there is a strong probability that such treatment would have benefit, although there are no data to support this view. One study demonstrated that serum 1,25(OH)2D levels were increased in patients with CKD and moderate kidney failure following the administration of a low-calcium diet, indicating that there is some “reserve” for the generation of 1,25(OH)2D in such patients.116
The treatment of vitamin D insufficiency or deficiency when present in CKD patients is warranted, since such therapy may reduce or prevent 2° HPT in the early stages of CKD.
Prospective, controlled clinical trials with the daily administration of ergocalciferol in a monthly amount equivalent to 1,000-2,000 IU/day are clearly warranted in patients with CKD and those undergoing dialysis, to assess the effects on serum PTH levels, serum 1,25(OH)2D levels, bone histomorphometry, and fracture rates. With the higher fracture rates known to occur in adult patients with Stage 5 CKD,289 studies to evaluate measures to minimize early 2° HPT would be warranted in patients with CKD of all ages.