JNC 7 summarizes the use of ambulatory blood pressure monitoring (ABPM) as follows5,5a:
It was the opinion of the Work Group that special considerations regarding blood pressure patterns in CKD justified an evaluation of the usefulness of ABPM in CKD. This evaluation suggested to the Work Group that ABPM should be used more often as a diagnostic tool and guide to antihypertensive therapy in CKD, and that controlled trials were needed to determine more precisely the circumstances in which it should be routinely used in CKD. All members of the Work Group concluded that a more thorough review of the subject was warranted. Suggestions in this Appendix reflect the opinions of several members of the Work Group.
Key definitions for this ABPM report can be found in Guideline 3. In addition to a consideration of reviews, an evaluation of primary articles was performed. For the primary literature review, articles were examined on individuals with essential hypertension as well as CKD, regardless of blood pressure, which (1) reported the correlation of office blood pressure with ABPM; (2) defined the prevalence of WCH; (3) described the prevalence of abnormal patterns of ABPM (nondipping or reverse dipping) in individuals with CKD; and (4) evaluated the relationship between ABPM and outcomes in CKD. Searches were also performed to identify studies examining how antihypertensive therapy affects ABPM, and its correlation with outcomes. Screening criteria for articles in ABPM are given in Appendix 2. Articles were reviewed by one member of the Work Group (RJP); data were not abstracted into evidence tables, and strength of evidence is not graded explicitly.
ABPM in Essential Hypertension
Recent authoritative reviews suggest advantages of ABPM in essential hypertension. ABPM has been widely used for the past decade but its use has been limited in the United States because of the expense of the equipment, the time involved in patient training and data analysis, and—until recently—the lack of consistent reimbursement. In Europe and parts of Asia, ABPM has become the standard for the measurement of blood pressure.
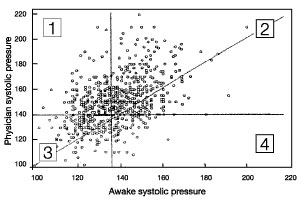
(1) Monitoring of blood pressure in an ambulatory setting provides multiple, objective blood pressure measurements in the patient’s own environment over a full circadian period. A study comparing the diagnosis of hypertension made by casual blood pressure (CBP) with ABPM is shown in Fig 63. When there is agreement between the two methods, the diagnosis of "true" normotension (area 3) or "true" hypertension (area 2) results. If CBP is elevated but ABP normal, this is defined as WCH (area 1). These patients have a level of end organ involvement that is not different from normotensive patients. When CBP is normal but ABP is elevated, this is termed "masked hypertension" (area 4). Patients with masked hypertension have end-organ damage similar to that in persistently hypertensive patients. All of these combinations may be observed in patients with CKD, but there are no studies specifically addressing the prevalence of each combination in CKD patients.
Fig 63. Comparison of the diagnosis of hypertension using casual blood pressure and ambulatory blood pressure monitoring. Figure compares the diagnosis of hypertension made by CBP and ABPM in 573 patients. Area 1 represents WCH; Area 2 represents true hypertensives; Area 3 represents true normotensives; Area 4 represents masked hypertension.598a
In adults, diagnostic ABP thresholds have been carefully defined in multicenter studies. The definitions take into account distributions of ABP in normal and hypertensive populations, validation of diagnostic thresholds in terms of LVH, and in terms of morbidity and mortality (Table 184).175 A meta-analysis of 18 studies demonstrated that CBP levels were greater than 24-hour, wake, or sleep ABP.142
(2) ABPM facilitates the diagnosis of WCH. ABP has been most useful in making the diagnosis of WCH.170 In a meta-analysis, the prevalence of WCH was found to be approximately 20% in the population of adults diagnosed as hypertensive by CBP. Too few studies were available for the analysis to determine the reproducibility of this classification. The question of whether WCH is an intermediate state between normotension and hypertension, or a prehypertensive state, remains unanswered. The ABPM Task Force168 determined that event-based studies in hypertensive patients have convincingly demonstrated that the risk of CVD is less in patients with properly defined WCH than those with higher ABP levels, even after controlling for concomitant risk factors. Based on prognosis, WCH can be defined as a CBP that is persistently ≥140/90 mm Hg with an average daytime ABP of below 135/85 mm Hg.168 WCH was associated with reduced risk of CVD compared to sustained hypertension, although the authors concluded that no prospective study adequately compared risk in patients with WCH versus normotensive patients. Under standardized conditions, the self-measurement of blood pressure can identify WCH, although there are insufficient data to compare the prognostic accuracy of SMBP with CBP and ABPM.142
The importance of the white coat effect is controversial. While WCH is defined by a normal ABP, the white coat effect takes into consideration the decrease in blood pressure seen with ABP compared to CBP. For example, a patient with a CBP of 180/120 mm Hg may have an ABP of 150/90 mm Hg. The patient is still hypertensive by ABP. Most, but not all, experts feel that the white coat effect (in this patient 30/30 mm Hg) is not of prognostic significance.
(3) Level of blood pressure and abnormal patterns by ABPM show a high correlation with end-organ damage. ABP has been shown to have an excellent correlation to hypertensive end-organ damage, such as cardiovascular mortality and events, abnormal left ventricular mass and function, cerebrovascular events, glomerular and tubular proteinuria, and is capable of identifying abnormal circadian blood pressure rhythms such as nocturnal hypertension. ABP is also important in demonstrating the rapid rise in early morning blood pressure that is associated with a high risk for CV events. Many of these studies are summarized in Table 185.599 An example of some of the patterns commonly seen with ABPM are seen in Fig 64.
Fig 64. Standardized common patterns of ABPM. Standardized common patterns of ABPM (ECF Medicatl Ltd., Blackrock, Co. Dublin, Ireland, www.ecfmedical.com). Common to all plots: vertical axes show blood pressures; horizontal axes shot 24-hour clock times; horizontal bands indicate normal values for 24-hour SBP and DBP; shaded vertical areas indicate night-time. (A) Normal ABPM pattern. This ABPM suggests normal 24-hour SBP and DBP (128/78 mm Hg daytime, 110/62 night-time), (B) White-coat hypertension. This ABPM suggest WCH (175/95 mm Hg) with otherwise normal 24-hour SBP and DBP (133/71 mm Hg daytime, 119/59 mm Hg night-time). (C) White-coat effect. This ABPM suggests mild daytime systolic hypertension (149 mm Hg), borderline daytime diastolic hypertension (87 mm Hg), borderline night-time systolic hypertension (121 mm Hg), and normal night-time DBPs (67 mm Hg) with white-coat effect (187/104 mm Hg). (D) Systolic and diastolic hypertension. This ABPM suggests mild daytime systolic and diastolic hypertension (147/93 mm Hg), but normal night-time SBP and DBP (111/66 mm Hg). (E) Isolated systolic hypertension. This ABPM suggests severe 24-hour isolated systolic hypertension (176/68 mm Hg daytime, 169/70 mm Hg night-time). (F) Hypertensive dipper. This ABPM suggests severe daytime systolic hypertension (181 mm Hg), moderate daytime diastolic hypertension (117 mm Hg) and normal night-time SBP and DBP (111/68 mm Hg). (G) Hypertensive nondipper. This ABPM suggest severe 24-hour systolic and diastolic hypertensive (210/134 mm Hg daytime, 205/130 mm Hg night-time).
There is a growing body of evidence showing that nondipping is associated with a worse prognosis, irrespective of whether night-time dipping is studied as a continuous or a class variable.174 The meta-analysis confirmed that a nondipping or reverse dipping pattern was associated with an increased risk of adverse events. A comparison of prediction of risk by ABP versus CBP in the meta-analysis was not deemed possible due to the uncertain quality of the CBPs, not ABPs. While repeated ABPM has excellent reproducibility for group data, this may not be the case for the individual patient.149
The international conference on ABPM in 2001 agreed that, while the incidence of cardiovascular events has some correlation with CBP, ABPM significantly refined the prediction. In the Syst-Eur Trial, 24-hour SBP measurements were found to be a significant predictor of cardiovascular risk.600 Some, but not all, studies have reported an independent and positive relationship between measures of variability (standard deviation of blood pressure divided by the mean blood pressure level) of daytime and night-time blood pressure and cardiovascular outcome. Finally, it has been suggested that ABP patterns can be predictive of pre-eclampsia early in pregnancy and that intervention with aspirin may prove beneficial in prevention.601 There are insufficient studies to assess the correlation of SMBP to end-organ damage.142
(4) There is insufficient evidence to conclude that adjusting medications using ABP is superior to using CBP measurements. The meta-analysis concluded that ABP has not been studied adequately to assess its role in antihypertensive therapy. Nonetheless, ABP’s predictive power for end-organ damage must be considered in drug trials. Further, ABP can give information unavailable through CBP, such as the trough to peak ratio over a period of time, rather than a single measurement. The missed-dose analysis can be helpful in demonstrating the duration of action of medication. Further, the ABPM may eliminate the need for placebos in drug trials and require fewer patients enrolled in order to prove efficacy.602
ABPM in CKD
CKD is associated with alterations in the circadian patterns of blood pressure; the most common of these rhythm abnormalities is sleep-associated hypertension and a nondipping blood pressure pattern. Patients with CKD have a high prevalence of a nondipping pattern (67%).176-178 These patterns are reproducible, with 67% of patients with CKD maintaining their baseline circadian rhythm and 82% having a predictable pattern on repeated monitoring. These patterns were even more reproducible in transplant and dialysis patients.174 The mechanisms for this pattern have not been clearly elucidated.603 It was also demonstrated that the prevalence of nondipping patterns is higher at lower GFR. Fifty-three percent of CKD patients with serum creatinine of <4.5 mg/dL (<400 µmol/L) had nondipping pattern progressing to 75% with creatinine of >6.8 mg/dL (>600 µmol/L) (Fig 65).604 The nondipping pattern observed in patients with type 1 and 2 diabetes605 has also been related to the presence of microalbuminuria.606 CKD patients, particularly kidney transplant patients, may have a reversed blood pressure pattern of higher sleep than wake BPs.
Fig 65. Blunting of the diurnal blood pressure rhythm of predialysis patients is more severe at lower GFR (higher serum creatinine concentration). To convert to mg/dL, divide by 88.4. Reproduced with permission.604
Abnormal ambulatory patterns have been shown to be related to varying degrees of abnormal protein excretion. Abnormal or nondipping pattern by ABPM is strongly correlated with microalbuminuria, macroalbuminuria, and proteinuria in a manner superior to CBP. This has been shown in studies of type 1 diabetes,179,607 type 2 diabetes,605,608 type 1 and type 2 diabetes combined,609-611 and essential hypertension.611-613 Some of the cross-sectional studies were performed in individuals labeled as having "essential hypertension" or "diabetes," but not specifically CKD. However, many individuals with microalbuminuria or macroalbuminuria would now be considered to have CKD based on the presence of this marker of kidney damage. Thus, these studies are pertinent to the target population for these guidelines. In the few studies examining possible mechanisms, autonomic dysfunction has been implicated.607,611
Furthermore, it has been shown that ABPM can identify individuals at risk for development of CKD. In type 1 diabetes, nocturnal blood pressure elevations determined by ABPM predated the development of microalbuminuria (Fig 66).179 Identifying individuals at risk for development of microalbuminuria provides an important window of opportunity for primary prevention.
Fig 66. Kaplan-Meier curves showing the probability of developing CKD (microalbuminuria) according to the pattern of daytime and nighttime systolic pressure in diabetes. The probability of microalbuminuria differed significantly between the two groups (P = 0.01 by the log-rank test; chi-square = 6.217 with 1 df). The risk of microalbuminuria was 70% lower in the subjects with a normal nocturnal pattern than in those with an abnormal nocturnal pattern.179
Abnormal ambulatory patterns have been shown to be related to CV damage and events. There are few studies in patients with CKD examining the relationship of ABP to morbid or mortal events. Three hundred and twenty-five patients with NIDDM were studied with ABPM with the circadian rhythm assessed by cosinor analysis.183 After an 8-year follow-up, 201 patients had a normal circadian rhythms and 87 had a reversed one. Twenty subjects in the group with normal rhythm (9.9%) had nonfatal (cerebrovascular, cardiovascular, peripheral vascular or retinal events) or fatal events versus 56 patients (64.4%) in the reversed group. Circadian pattern of blood pressure and age had the greatest effect on adverse events in Cox proportional hazards model (Fig 67).
Fig 67. Survival curves of diabetic subjects with normal (N) and reversed (R) circadian blood pressure rhythms. The unadjusted relative risk for diabetic subjects with a reversed circadian blood pressure rhythm was 20.6-fold higher than that of subjects with a normal rhythm (P < 0.001; Cox-Mantel’s test).183
The meta-analysis of 25 studies examining the relationship of ABP levels with target-organ damage was positively associated with ABP. In 10 studies, at least one dimension of ABP predicted subsequent clinical events prospectively.
Fig 68. Relationship between end-systolic left ventricular diameter and percent fall in blood pressure (sleep to awake) in hemodialysis patients and kidney transplant recipients. The less the fall in blood pressure during sleep, the more dilated the LV chamber. Reproduced with permission.618
The correlation of end-organ damage to cardiovascular end points is similar in patients with CKD to that reported in essential hypertensive patients. The same correlation between ABP and measures of left ventricular mass is seen, regardless of the cause of CKD: ADPKD,614 CKD,184,615 glomerulonephritis,616 hypertension with albuminuria,186,612 IgA nephropathy,617 NIDDM,183 and in kidney transplant recipients178,618 (Fig 68). The recurring theme in these articles is the finding of a positive correlation of left ventricular mass with ABP parameters; most commonly, a nondipping pattern or sleep-related hypertension. In each of the studies there were either weak or, more commonly, no correlations between CBP and these outcomes. The combination of the 24-hour systolic ABP with a measure of dipping, the night to day ratio, was a strong predictor of cardiovascular end points in the Systolic Hypertension in Europe Trial (Fig 69).
Fig 69. Night to day blood pressure ratio and 24-hour SBP at entry as predictors of the 2-year incidence of cardiovascular end-points in 393 patients randomized to the placebo group of the Systolic Hypertension in Europe Trial. Using Cox regression analysis, the event rate was standardized to female sex, mean age (69.6 years), a lack of previous cardiovascular complications, nonsmoking status, and residence in Western Europe. Incidence is given as the probability of an event per 100 patients. Reproduced with permission.600
Abnormal ambulatory patterns have been related to more rapid progression of kidney disease. There are five studies that examine the association of ABP with kidney disease progression. Out of 126 patients with IgA nephropathy, those who had ambulatory hypertension developed higher plasma creatinine values whereas the normotensive patients, with or without antihypertensive therapy, had stable serum creatinine. Nondippers made up 93% of the hypertensive patients. The normotensive patients who were nondippers also had higher creatinine values than dippers.180 In a 3-year study, 48 patients with CKD were studied: 28 dippers and 20 nondippers.181 Nondippers had a faster decline in GFR (4.4 mL/min/y) versus dippers (3.2 mL/min/y) and a higher mean protein excretion. In a similar study of diabetic patients, nondippers had a 7.9 mL/min/y decline compared to 2.9 for dippers182 (Fig 70). Finally, Nakano et al619 examined 257 patients with NIDDM. Patients had a normal circadian rhythm (193) or a reversed pattern (63). More of the reversed patients (23.5%) progressed to hemodialysis compared to those with normal rhythm (3%).619 Jacobi et al620 demonstrated the direct relationship between ABP and serum creatinine 6 months posttransplant (Fig 71).
Fig 70. Diurnal blood pressure rhythm in diabetic kidney disease. Comparison of two groups of patients with diabetic kidney disease matched for daytime blood pressure, cholesterol, proteinuria and diabetic control—one cohort (left) with normal diurnal blood pressure, and an average creatinine clearance decline of 2.9 mL/min compared to the other cohort (right) with abnormal diurnal blood pressure, and a rate of creatinine clearance decline of 7.9 mL/min. Reproduced with permission.182
Fig 71. Correlation of creatinine values in patients 6 months after kidney transplantation with 24-hour SBP (left) and DBP (right). Reproduced with permission.620
Due to these abnormal patterns, the correlation between CBP and ABP is poor, as is the relationship of CBP to end-organ damage. Three studies of diabetic patients showed a significant association of ABP to urinary albumin excretion where CBP failed to do so. Once again, SBP and nocturnal elevations had the closest correlation to this measure of end organ damage. In nondiabetic CKD patients, five studies have demonstrated the same finding. McGregor et al178 demonstrated a nondipping pattern in kidney transplant recipients which was associated with LVH, whereas CBP did not. Tucker et al184 showed that casual SBP and DBP had a weak correlation (0.25 to 0.22) to LVH in CKD patients, while systolic ABP had a correlation of 0.52 and diastolic ABP 0.42. Nocturnal BPs had an even better correlation.
Patients with CKD can have WCH; the diagnosis of WCH could affect the requirement for antihypertensive therapy. The prevalence of WCH has not been determined reliably in CKD, especially in relation to CKD stages. In essential hypertension, WCH is more likely to occur in patients with lesser stages of hypertension severity. Thus, the prevalence of WCH might be lower in patients with CKD. Nonetheless, the diagnosis may have importance in determining the need for antihypertensive therapy.
There are three studies specifically examining the issue of WCH in various types of CKD, which mirror results observed in patients with essential hypertension. The prevalence of WCH among patients is definition-dependent. The more severe the hypertension, the lower the prevalence of WCH608 (Fig 72).
Fig 72. Rates of major cardiovascular events in a normotensive group (A), two groups with WCH defined using restrictive (B) or liberal (C) criteria, and a group with ambulatory hypertension (D). Reproduced with permission.621,622
The prevalence of end-organ damage is low in CKD patients with WCH.170 In the HARVEST study of 942 patients with Stage 1 hypertension, patients with WCH had significantly lower left ventricular mass and microalbuminuria compared to established hypertensive patients. There was no difference in end-organ damage between WCH and normotensive controls.185
The diagnosis of nocturnal hypertension in CKD could affect the requirement for antihypertensive therapy. Concerns in CKD patients who have altered patterns of blood pressure and a nondipping blood pressure pattern include (1) CBP may not correctly represent blood pressure burden and risk; and (2) confining the definition of WCH to the daytime blood pressure comparisons by ABPM, a common practice, or SMPB may include patients with sleep-related hypertension in the WCH category. This issue will require further study.
There is insufficient evidence to determine whether ABPM is a better monitoring tool than CBP for assessing the effectiveness of antihypertensive therapy to reduce kidney disease progression or CVD risk in CKD. Several studies in CKD have shown advantages of ABPM on surrogate outcomes. In treating hypertensive CKD patients, LVH was found to be present only when the patients were noted to have persistently abnormal ABP, but not CBP. When treatment decisions were made by CBP, 13% of patients had LVH compared to none of the patients controlled by ABP criteria.186 A comparison of lisinopril with nisoldipine showed a decrease in microalbuminuria with no change between albuminuria groups by CBP; however, there were differences between groups for night-time SBP by ABP.623 In type 1 and type 2 diabetic patients, both pretreatment and posttreatment changes in microalbuminuria were associated with nocturnal blood pressure changes, but not CBP.609 In the Heart Outcomes Prevention Evaluation (HOPE) trial, the ACE inhibitor ramapril was clearly shown to reduce cardiovascular events in patients with vascular disease.105 Blood pressure measurement protocols were less than adequately defined. Further, the small changes noted in CBP (3/2 mm Hg) in light of the major improvement in events were interpreted to mean that this beneficial effect was due to the character of the drug itself, rather than the blood pressure lowering effects. However, a substudy using ABPM in the HOPE trial showed a clear and significant reduction in blood pressure, particularly at night, raising doubts about the prior conclusion (Fig 73).624,625 Most recently, the prognostic value of ABP was documented in the Office versus Ambulatory Blood Pressure Study, where 1,963 hypertensive patients were followed for a mean of 5 years.172 The investigators demonstrated that ABP was an independent and significant risk factor for CV events, even after adjustment for classic risk factors, including office blood pressure. They also noted that CV outcomes are better predicted by ABP than CBP. Most notable was the finding that patients whose mean 24-hour ABP was ≥135 mm Hg when receiving treatment were nearly twice as likely to have CV events as patients with <135 mm Hg, regardless of their CBP measurement.
Fig 73. Comparison of cuff blood pressure, 24-hour ABPM, and night-time ABP in the HOPE Study and a HOPE Substudy.
Clinicians may find benefit in recommending ABPM for patients with CKD. Although the Work Group did not recommend routine monitoring of ABP, it recognizes that health-care providers may find benefit in recommending this technique for individuals with CKD for the indications listed in JNC 7 and those listed in Table 75. Indeed, its prognostic value has also been documented in patients with treated hypertension.172 ABPM results have a close correlation with end-organ damage, including progression of kidney disease and clinical CVD outcomes. It may be of particular benefit in patients with CKD who have a known alteration in the circadian blood pressure pattern that cannot be revealed using CBP measurements. The presence of a nondipping pattern or nocturnal hypertension in a patient with CKD places an already high-risk patient into an even higher-risk group. This knowledge may be helpful in suggesting an even more aggressive therapeutic regimen.