Blood pressure can be determined by resting blood pressure measurement in the health-care provider’s office (casual blood pressure [CBP]), self-measured blood pressure (SMBP), or ambulatory blood pressure monitoring (ABPM).
3.1 Blood pressure should be measured according to the recommendations for indirect measurement of arterial blood pressure of the American Heart Association and Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC 7) (A).
3.2 Patients should be taught to measure and record their blood pressure, whenever possible (C).
3.3 Ambulatory blood pressure monitoring should be considered for patients with CKD for the following indications (C):
3.3.a Suspected white coat hypertension
3.3.c Hypotensive symptoms while taking antihypertensive medications
CBP recorded in a clinic/office setting is the standard technique for measurement of blood pressure. Techniques for this measurement are well detailed in the Seventh Report of the Joint National Committee (JNC) on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure5,5a as well as many recent reviews.142-144 The purpose of Guideline 3 is to review the recommended measurement methods for adults, particularly in relation to CKD. A discussion of blood pressure measurement and interpretation in children is given in Guideline 13.
The measurement of blood pressure in this technological age has never been more confusing or difficult. The currently available CVD risk prediction data come from studies that primarily used an auscultation technique with mercury manometer.144 Environmental concerns have led to the abolishment of mercury columns in many US and most European health-care facilities.145 Aneroid manometers can be accurate if maintained by an intensive and difficult to achieve calibration and maintenance program. Automated devices using oscillometric technology have gained great popularity due to ease of use and improved interobserver variability. Not surprisingly, these devices that measure vessel oscillations do not always correlate well with auscultatory techniques146 and also require frequent calibrations performed by the manufacturer. Thus, from a clinical perspective, it is not clear which are the best monitors to use for CBP measurement.
However, even if CBP measurement by standardized protocols is performed under ideal circumstances, they have a number of limitations, especially in conditions, such as CKD, in which known aberrations in circadian blood pressure patterns exist. SMBP provides multiple blood pressure measurements in the patient’s own environment but is a technique with many technical and reporting reliability issues. Studies relating the SMBP data to target organ damage are lacking. ABPM provides objective blood pressure measurements in the patient’s own environment over the full circadian period and correlates well with target organ damage. Normative data, based on epidemiological studies, outcome measures, and cardiovascular events, have now been developed for ABPM. Guideline 3 briefly summarizes more recent data on SMBP and ABPM, with a more detailed discussion in Appendix 3. As technology advances, the ultimate goal for antihypertensive therapy is to develop what has been termed "the virtual hypertension clinic"147 using CBP for screening, ABPM for initial diagnosis, and monitoring changes in treatment; and SMBP with electronic linkage between the patient and the health-care provider for maintenance and follow-up.
Definitions
Casual blood pressure (CBP): CBP refers to a blood pressure measurement taken in the physician’s office or clinic setting using one of several techniques. Auscultatory techniques with aneroid or mercury manometers and automatic oscillometric devices are most commonly used. Measurement under standardized conditions should be taken at least twice and an average of the two recorded at every health-care encounter.5 Multiple measurements at different encounters are required for accurate correlation to end-organ damage.
Self-measured blood pressure (SMBP): SMBP refers to blood pressure measurements taken by the patient in his/her usual environment. SMPB devices142 are varied in design from manual to fully automated and in blood pressure measurement technique (mercury, aneroid, oscillometric). Little is known about the accuracy, reliability, and predictive value of SMBP, especially in CKD patients. Patients performing SMBP should be trained and periodically monitored.
Ambulatory blood pressure monitoring (ABPM): A variety of fully validated, reliable, automated, and accurate monitors are available. Blood pressure measurements taken every 15 to 20 minutes are recorded over 24 to 48 hours. Oscillometric monitors are most commonly used and auscultatory monitors with or without ECG gating also give excellent results. Data downloaded from the monitor are generally divided into day (diurnal) or night (nocturnal) periods. Daytime (awake) ambulatory blood pressure (ABP) values are lower than clinic readings, 10% to 20% higher than nighttime (asleep) readings, and provides measures of SBP and DBP load (percentage of blood pressure readings exceeding the upper limits of normal for a given time period). As blood pressure is more closely related to the sleep-wake cycle rather than day and night, as illustrated by the blood pressure rhythm following the inverted cycle of activity in night-shift workers, the time of sleep and wake during ABPM should be recorded in the patient diary or objectively determined with a motion-logger (actigraph). Recently, monitoring has been approved for reimbursement in selected settings including the identification of white-coat hypertension (WCH). A consensus view on ABPM technique is available.148 While reproducibility on repeated ABPMs for group data is excellent, concerns regarding individual patient reproducibility have been raised.149
Ambulatory hypertension: Ambulatory hypertension is most commonly diagnosed by a mean SBP or DBP exceeding normal values for the full 24-hour period. Other definitions include blood pressure values that exceed normal during the waking period (diurnal hypertension) or the sleep period (nocturnal or sleep hypertension). Blood pressure load has a strong predictive value for end-organ damage. Other promising analytic techniques need further validation, such as the cosinor analysis, modified LMS of Cole and Green (where the distribution of a measurement Y is described by its median [M], the coefficient of variation [S], and a measure of skewness [L] required to transform the data to normality),150 blood pressure index, and hyperbaric index.
White coat hypertension (WCH): WCH refers to a condition in which blood pressure is repeatedly elevated on CBP measurement in the presence of a health-care professional but normal by ABP or SMBP. WCH for adults is defined by CBP >140 mm Hg, but a mean blood pressure by ABPM of <135/85 mm Hg for the wake period or <135/80 mm Hg for the full day. Some consider that the criteria include a blood pressure load <25%. Whether WCH is associated with end-organ damage is controversial and definition-dependent. Patients with WCH defined by 24-hour mean blood pressure <135/85 mm Hg have a prevalence of end-organ damage or CV events not different from normotensive patients. However, WCH may prove to be a prehypertensive state.
Dipping: Dipping describes an ABP pattern in which the mean wake SBP or DBP falls at least 10% during sleep. A sleep-related blood pressure reduction that is greater than 20% to 30% has been termed super-dipping, which is associated with neurological sequelae.151
Nondipping: Nondipping describes a pattern of a blunted sleep-related fall in mean SBP or DBP (<10%). This pattern is commonly seen in CKD. The most severe form is a reversal of blood pressure in which the sleep blood pressure is equal or higher to awake values. Some have termed this "reverse dipping" and connotes a very high risk for end-organ damage.
Scope of Work
Studies reviewed for this guideline included authoritative reviews, including JNC 615 and JNC 75,5a; a meta-analysis conducted for AHRQ142 National High Blood Pressure Educational Program (NHBPEP)/National Heart, Lung and Blood Institute,152 and American Heart Association (AHA) Working Meeting on Blood Pressure Measurement 2003152 and its summary report144; AHA recommendations for indirect measurement of arterial blood pressure,153 European Society of Hypertension recommendations for conventional, ambulatory, and home blood pressure measurement143; and an international conference on ABPM in 2001.154 More detailed information about blood pressure measurement techniques can be found in these reports.
Strength of Evidence
Accurate measurement of blood pressure is important for detection, evaluation, and treatment of hypertension (Strong). JNC 7 provides a new, simplified classification of hypertension severity for adults aged 18 years and older (Table 23). The classification is based on the average of two or more properly measured seated blood pressure readings on each of two or more office visits. When SBP and DBP fall into different categories, the higher category should be selected to classify the individual. Accurate measurement in CKD is especially important, because hypertension is more common in CKD, and because JNC 7 identifies CKD as a "compelling indication" for more aggressive antihypertensive therapy because of the higher risk of CVD in CKD than in the general population.
Accurate assignment of blood pressure status is crucial from a public health standpoint.144 The risk associated with increasing blood pressure is graded and continuous and begins at 115/75 mm Hg. Overestimating or underestimating blood pressure by even 5 mm Hg can mislabel over 20 million persons as having high normal blood pressure rather than hypertension; conversely, another 20 to 30 million could be misclassified as hypertensive exposing these persons to the expense and adverse effects of treatment. This issue is compounded by the challenge of the "white coat" or "office" effect. Misclassification in CKD can be compounded by altered circadian blood pressure rhythms such as a nondipping pattern.
The following techniques that are recommended for accurate measurement of casual blood pressure in the general population are also recommended in CKD (Strong). The following issues are common to all measurements and all devices. Issues related to type of blood pressure measurement and specific devices are discussed next.
Casual blood pressure measurement using the mercury manometer is the "gold standard" for clinical studies, but has important limitations in clinical practice (Strong). One of the most controversial areas is the choice of equipment for blood pressure measurement. Measurements should be taken preferably with a mercury sphygmomanometer if available. Otherwise, a calibrated aneroid manometer or a validated electronic device can be used. Technical problems exist with all forms of blood pressure measurement. Even the gold standard of intra-arterial blood pressure measurement has technical problems and variability depending on the chosen artery, catheter positioning within the artery, and equipment used. The two major noninvasive CBP measurement techniques are auscultatory and oscillometric. The hybrid manometer and devices based on wideband K2 method are future technologies that may be helpful.143
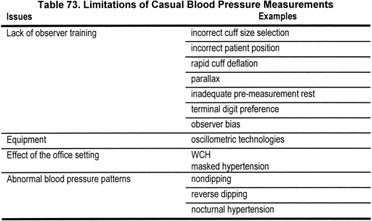
CBP measurements can be misleading due to errors from lack of observer training, incorrect cuff size, incorrect patient position, rapid cuff deflation, terminal digit preferences, monitor not kept at eye level (parallax), and inadequate premeasurement rest as well as the stress of the office setting (Table 73). The aforementioned problems have led to a proliferation of easier-to- use automated devices using oscillometric technologies. Users of these devices need to realize that the oscillometric technique is not based on the same physiological observation as auscultation144 and thus may yield different results.
Even if office blood pressure measurements follow standardized protocols under ideal circumstances, the measurements are limited by tremendous variability. Use of a single measurement to characterize the chronic behavior of a continuous variable may be unrealistic. Further, the measurement may not be representative of blood pressure levels in the patient’s own environment and at different times of day. This is especially true when known aberrations in circadian blood pressure patterns exist in a given clinical condition, such as in CKD. Whatever the chosen device, the guidelines of the future should be evidence-based rather than consensus-based.
Regulatory agencies need to establish standards for the use of validated devices, the frequency of calibration, and the continued certification of observers using manual devices. The use of automated devices does not eliminate all major sources of human error and thus observers still require training. Manufacturers of automated devices should validate their algorithms in special populations such as the elderly and those with CKD.
Mercury manometers. Despite their status as the gold standard, mercury manometers, when systematically evaluated, have a significant number of problems that may preclude accurate use, even if the observer and patient issues are overcome. In several studies, a high prevalence of technical problems (18% to 38%) was noted, such as dirty columns, oxidized mercury, faded column markings, air mixed in the mercury column, or mercury leakage leading to inaccurate measurement in 21% of monitors.156-158 In a systematic evaluation of sphygmomanometers, none of the 356 instruments tested met all standards and 86% did not meet safety standards.159 In addition, because of the environmental hazard posed by mercury, most mercury manometers in hospitals and other health care facilities in the United States are being replaced by other instruments.
Aneroid manometers. The aneroid manometer functions by use of a system comprised of a metal bellows, a mechanical amplifier, springs, and a gauge that displays the pressure in the cuff and tubing of the sphygmomanometer. Aneroid devices are often felt to be less accurate than mercury columns because they are so difficult to keep in calibration.153 Aneroid manometers were evaluated in many of the same studies cited for the assessment of mercury manometers and demonstrate even more inaccuracies than with mercury.
Oscillometric devices. Oscillometric monitors measure the mean arterial pressure by determining the maximum oscillations in the vessel. The device then calculates SBP and DBP from proprietary algorithms. There is great variability in blood pressure readings among available devices. We have no standards for normal blood pressure based on this technology. Further, there are concerns that increased arterial stiffness as seen in CKD and the elderly can lead to greater variations in blood pressure results by oscillometry compared to auscultation. Some companies are developing special algorithms for these situations.
Self-measured blood pressure is a useful adjunct to casual blood pressure monitoring (Moderately Strong). Self-measurement of blood pressure has five general advantages: (1) distinguishing sustained hypertension from WCH; (2) assessing response to antihypertensive medication; (3) interpreting symptoms that may be due to hypotension; (4) improving patient adherence to treatment; and (5) potentially reducing costs. The blood pressure of persons with hypertension tends to be higher when measured in the clinic than outside of the office. There is no universally agreed-on upper limit of normal home blood pressure, but readings of 135/85 mm Hg or greater should be considered elevated.5 The techniques of a well-performed CBP should be used with SMBP including a 5-minute rest before the sitting measurement. The technique is carefully outlined in the European Society of Hypertension Report.143
Choice of monitors for personal use. A mercury sphygmomanometer is generally not practical for home use. Therefore, either validated electronic devices (oscillometric) or aneroid sphygmomanometers are recommended for use along with appropriately sized cuffs. Finger and wrist monitors are inaccurate. Periodically, the accuracy of any device should be checked by comparing readings with simultaneously recorded auscultatory readings taken with a mercury device. Few of the many self monitors on the market have passed British Hypertension Society160/Association for the Advancement of Medical Instrumentation standards.161 A Task Force of the European Society of Hypertension has suggested new criteria for this assessment.162 A review of available monitors has been published recently.160,163
Comparison of SMBP with CBP measurement and ABPM. Blood pressure measured by any technique outside of the physicians office tends to have lower values. In six studies comparing SMBP and CBP, a consistently lower blood pressure by SMBP (SBP 5.4 ± 17.7 mm Hg and DBP 1.5 ± 6.3 mm Hg) was demonstrated. Three studies comparing ABPM and SMBP show similar daytime blood pressure results. While ABPM is the gold standard for the determination of WCH, SMBP is comparable to ABPM for prevalence of WCH (approximately 20%). The published literature is insufficient to provide an answer to the predictive ability of SMBP for target-organ damage or clinical events. Interventions that included SMBP for assessment of antihypertensive effect showed improved blood pressure control in 6 of 12 trials.142 Of the two trials that used technology storing the blood pressure data in the monitor, significantly reduced blood pressure was seen. Thus, while the results are inconsistent, there is promise—especially with report-generating monitors—that SMBP can lead to reduced blood pressure.
SMBP reliability. The reliability of the patient recording of the blood pressure measurement is critical if this technique is to be trusted. Patients consistently misreport the results of the monitor when patient manual recordings are compared to a device that stored readings unbeknownst to the patient. Patient reports had mean differences in blood pressure of at least 10 mm Hg for SBP and 5 mm Hg for DBP compared to stored readings.164 In another study, 36% of patients underreported and 9% overreported blood pressure readings. Log books also had phantom readings noted; conversely, patients failed to report measurements that were taken and stored.165 Similar findings were observed with other monitoring technologies such as glucometers for diabetic patients166 and for recording metered dose inhaler usage in asthmatic patients.167 Thus, objective recording of the data is strongly advised. The Work Group concluded that SMBP is a useful adjunct to CBP measurement with properly validated monitors, can be performed by many patients, and is consistent with the goal of self-management.
ABPM is useful to identify abnormal blood pressure patterns in CKD and is closely correlated with target-organ damage (Strong). Monitoring of blood pressure in an ambulatory setting provides multiple, objective blood pressure measurements in the patient’s own environment over a full circadian period.168 While ABPM has become a valuable clinical and research tool, it has yet to gain wide acceptance in the United States due to reimbursement issues, equipment expenses, and time efforts to train patients in monitor use. The Center for Medicare and Medicaid Services (CMS) has approved ABPM use for patients suspected of white coat hypertension.169 In Europe, however, ABPM has become a mainstay of blood pressure diagnosis and management. WHO-ISH suggests it be used for unusual variability of blood pressure, office hypertension in low-risk patients, symptoms suggesting hypotensive episodes, and resistant hypertension. JNC 7 suggests ABPM can be useful for suspected WCH, resistant hypertension, hypotensive symptoms while taking antihypertensives, episodic hypertension, and autonomic dysfunction.
Recent authoritative reviews suggest advantages of ABPM in essential hypertension.142 ABPM facilitates the diagnosis of WCH, a prehypertensive state that shows a lack of end-organ damage similar to that seen in normotensive individuals.170 Conversely, it has been reported that as many as 9% of patients may have normal office blood pressure but elevations during ABPM; a condition termed "masked hypertension" which is also associated with end-organ damage.171-173 Among persons with hypertension, an extensive and very consistent body of evidence indicates that ambulatory blood pressure correlates more closely than casual blood pressure with a variety of measures of target-organ damage such as left ventricular hypertrophy.15,174
Ambulatory blood pressure values are usually lower than clinic readings. While awake, individuals with hypertension have an average blood pressure of more than 135/85 mm Hg and during sleep, more than 120/75 mm Hg (Table 74). In most individuals, blood pressure decreases by 10% to 20% during the night; those in whom such reductions are not present are at increased risk for cardiovascular events.
CKD is commonly associated with alterations in the circadian patterns of blood pressure; the most frequent of these rhythm abnormalities is nocturnal (sleep) period hypertension and a nondipping blood pressure pattern.176-178 As stated in JNC 7, the level of mean ABP or blood pressure load correlates better than office measurements with target organ injury. Abnormal ambulatory patterns have been shown to be related to varying degrees of abnormal protein excretion,179 to more rapid progression of kidney disease,180-182 and to CV damage and events.183 Due to these abnormal patterns, the correlation between CBP and ABP is poor, as is the relationship of CBP to end-organ damage.178,184
Several ABPM patterns noted in CKD patients and not detected by CBP measurement can impact therapeutic decisions. First, the requirement for antihypertensive therapy may be affected by the diagnosis of WCH.185 Secondly, the identification of a nondipping, reverse dipping, or nocturnal hypertension may lead to more aggressive antihypertensive regimen and affect the timing of dosing.180 Further, a recent study of treated hypertensive patients172 suggests that ambulatory blood pressure of >130/80 mm Hg is associated with cardiovascular events even with a normal office blood pressure. Thus, data are accumulating, but are not yet conclusive for the usefulness of routine ABPM for antihypertensive therapy.
In summary, ABPM is a powerful tool that has a close correlation with end-organ damage, including progression of kidney disease, and cardiovascular and cerebrovascular outcomes. It is of particular benefit in patients with CKD who have a known alteration in the circadian blood pressure pattern. The presence of a nondipping pattern or nocturnal hypertension in a patient with CKD places an already high-risk patient into an even higher risk level. Possibly, this knowledge can be helpful in suggesting an even more intensive therapeutic regimen. However, the Work Group did not find a sufficient number of large studies demonstrating an additional benefit of ABPM over CBP measurements in the management of hypertension in CKD. Thus, the Work Group concluded that additional evidence is required to recommend ABPM as a routine diagnostic tool or as a guide to blood pressure management in CKD. Until such evidence is available, health-care providers may find benefit in choosing to recommend ABPM for patients with CKD.186 Circumstances for effective utilization of ABPM in patients with CKD are seen in Table 75.
A summary of special considerations in blood pressure measurement for patients with CKD is found in Table 76.
ABPM is becoming more widely used, yet important limitations remain such as the expense of equipment and software, and personnel required to apply the equipment; high test-retest variability in some individuals, and reimbursement issues. While reimbursement for the use of ABPM in diagnosing white coat hypertension has been approved by the Center for Medicare and Medicaid Services, it is not yet approved for conditions with altered patterns of blood pressure as in CKD.
Self-measurement of blood pressure has a much lower cost and few side-effects. It allows improved assessment of blood pressure and its control but the technology requires more careful scrutiny of quality and accuracy and the use of devices to objectively record the data to improve reporting. Digital read-out devices simplify SMBP. Clinicians need to devote time for teaching and assessing patient accuracy. Development of instructional material for patients with a wide range of educational levels and cultural backgrounds will be important.
The disappearance of mercury manometry will lead to new challenges and opportunities. We may be entering a new age of blood pressure measurement with the introduction of innovative technologies that will allow not only accurate, noninvasive measurement of blood pressure but also an assessment of blood pressure as a dynamic process with the ability to measure the cardiac and vascular components of blood pressure, thereby bringing new understanding and opportunities for early diagnosis and therapies.
There are many unanswered questions related to the measurement of blood pressure in the CKD population.