Dietary and other therapeutic lifestyle modifications are recommended as part of a comprehensive strategy to lower blood pressure and reduce CVD risk in CKD.
6.1 Dietary sodium intake of less than 2.4 g/d (less than 100 mmol/d) should be recommended in most adults with CKD and hypertension (A).
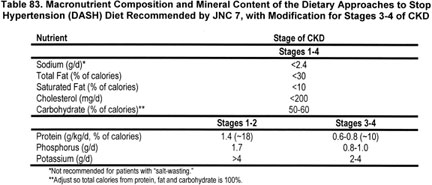
6.2 Other dietary recommendations for adults should be modified according to the stage of CKD (Table 83) (B).
6.3 Lifestyle modifications recommended for CVD risk reduction should be recommended as part of the treatment regimen (Table 84) (B).
6.4 Referral to a registered dietitian should be considered to help patients achieve dietary recommendations (C).
In the general population, dietary and lifestyle modifications that lower blood pressure are widely advocated as part of strategies to prevent and treat hypertension. Individuals with CKD have significant comorbid conditions in addition to high blood pressure, for which dietary modifications are recommended, including diabetes, CVD, obesity, and hyperlipidemia. Therefore, Guideline 6 compiles dietary modifications recommended for the general population as they apply to CKD Stages 1-4 for management of high blood pressure and other comorbid conditions.5,276,277 NKF-K/DOQI dietary recommendations for CKD Stage 5 are detailed elsewhere.278 In addition to dietary changes, other lifestyle modifications should be part of a comprehensive lifestyle intervention.
Individuals with multiple comorbid conditions in addition to CKD should receive dietary advice from a registered dietitian as part of routine care. Some currently popular weight loss diets may contain excessive protein or potassium for later stages of CKD
Scope of Review
Controlled trials evaluating lifestyle modifications for blood pressure management in CKD are limited. For this guideline, recommendations for high blood pressure and other conditions were integrated with recommendations for CKD.
Strength of Evidence
Dietary and lifestyle modifications are recommended in the general population for reduction of CVD risk (Strong). Prospective cohort studies and controlled trials have identified specific dietary patterns that are effective at reducing the risk of CVD. Diets that include nonhydrogenated, unsaturated fats as the predominant form of dietary fat appear to provide the most protection against coronary heart disease. Diets that include whole grains as the main form of carbohydrates, an abundance of fruits and vegetables, and adequate omega-3 fatty acids also offer significant protection.279 It has been proposed that such diets—together with regular physical activity, avoidance of smoking, and maintaining a healthy weight—could prevent the majority of CVD in adults.280 The beneficial effects of diet on traditional CVD risk factors, including lipid reduction, prevention of diabetes, and blood pressure reduction, may account for most of the overall CVD risk reduction.
Dietary and lifestyle modifications are recommended for prevention and treatment of high blood pressure in the general population (Strong). JNC 7 recommends lifestyle modifications as initial therapy in newly diagnosed hypertensive patients and as adjuvant therapy in persons on medications.5 Apart from physical activity, most lifestyle recommendations are nutrition-based and include (1) reduction of dietary sodium consumption to <100 mmol/d (2.4 g/d); (2) weight loss (for overweight and obese persons) and weight control (for nonoverweight); (3) moderation of alcohol intake (≤2 drinks per day for men and ≤1 drink/day for women); and (4) adoption of the Dietary Approaches to Stop Hypertension (DASH) diet.
The DASH diet is effective in reducing blood pressure in adults with high normal and Stage 1 hypertension (Strong). The DASH Trial demonstrated substantial reductions in blood pressure in adults with high normal blood pressure (135/85 to 139/89 mm Hg) and Stage 1 hypertension (blood pressure 140/90 to 159/99 mm Hg)230,281,281a with adoption of a diet that emphasizes fruits, vegetables, and low-fat dairy products; includes whole grains, poultry, fish, and nuts; contains only small amounts of red meats, sweets, and sugar-containing beverages; has decreased amounts of total and saturated fat and cholesterol and a modest increase in protein. The 8 to 10 servings of fruits and vegetables per day are approximately twice the average of 4.3 servings per day consumed by US adults. The magnitude of blood pressure reduction in the hypertensive subgroup was 8 to 10 mm Hg lower in those who consumed the DASH diet compared to those that consumed the control diet (Fig 33). The magnitude of blood pressure reduction is similar to the reduction seen with pharmacological therapy in other trials.
Fig 33. Mean change in SBP (mm Hg) from baseline in hypertensive participants of the DASH study during 8 weeks of intervention by diet assignments—DASH or control diets. Horizontal axis, weeks after dietary instruction; vertical axis, change in systolic blood pressure (mm Hg) from baseline. Figure modified and reprinted with permission.281a
In the DASH-Sodium Trial,281 adoption of the DASH diet lowered blood pressure at all sodium levels compared to a diet similar to that consumed by US adults. In addition, blood pressure was lowered in consumers of a DASH diet or a typical American diet by reducing the sodium intake from 140 mmol/d (3.2 g/d) to 100 mmol/d (2.4 g/d, the currently recommended upper limit). An even greater blood pressure reduction (ie, a larger reduction per mmol Na) was achieved with consumption of either diet at a still lower level of sodium 65 mmol/d (1.5 g/d).
While the DASH and DASH-Sodium Trials have demonstrated the short-term efficacy and safety of these diets in adults with high normal blood pressure and hypertension, these trials did not include hypertensive adults with CKD.
Reduction in dietary sodium intake lowers blood pressure in CKD (Strong). Clinical and experimental studies clearly show that sodium handling by the kidney is altered in CKD, and that sodium retention has a major role in hypertension in CKD.281d The primary mechanism appears to be expansion in extracellular fluid (ECF) volume.282 Dietary sodium restriction is recommended to reduce ECF volume expansion and lower blood pressure. Based on the results of the DASH and DASH-Sodium Trials, the Work Group recommended that most individuals with CKD should reduce sodium intake to less than 100 mmol/d (2.4 g/d). Further reduction in sodium intake to <50 mmol/d (<1.2 g/d) might lower blood pressure further, but may be more difficult to achieve.
Not all patients with CKD have ECF volume expansion. In some tubulointerstitial diseases, defects in tubular sodium reabsorption lead to ECF volume depletion ("salt-wasting" nephropathy), usually accompanied by episodic hypotension rather than hypertension. Dietary sodium should not be restricted in such patients. Nevertheless, some patients with salt-wasting nephropathy develop hypertension and require treatment with antihypertensive agents. Salt-wasting is more common in children with CKD and is discussed in Guideline 13.
There is insufficient evidence to determine the most appropriate low sodium dietary regimen for patients with CKD. While the DASH diet is effective in short-term blood pressure lowering in the general population, the macronutrient components and mineral components of the DASH diet, other than sodium restriction, have not been studied carefully in CKD. It was the opinion of the Work Group that the DASH diet may be appropriate for individuals with CKD Stages 1-2, but not for later stages, as discussed below. The recommendations for sodium, protein, potassium, and phosphorus for CKD Stages in Table 83 are consistent with the DASH diet and with the usual intakes in adults in the United States.
The DASH diet contains a higher protein, potassium, and phosphorus content than is recommended for patients with CKD Stages 3-4 (Strong). The optimal level of dietary protein intake to slow the progression of CKD and maintain protein nutritional status is not known. The DASH diet has a protein content (18% protein; approximately 1.4 g/kg/d) that is higher than the recommended daily allowance (US-RDA) for healthy adults (0.80 g/kg/d),283,283a and exceeds NKF-K/DOQI guidelines for CKD Stage 3 (0.75 g/kg/d) and CKD Stage 4 (0.60 g/kg/d).278 The K/DOQI recommendations are based on observations that reduced dietary protein intake reduces the generation of nitrogenous wastes and inorganic ions, which can lead to uremia. In addition, post hoc analyses from the Modification of Diet in Renal Disease (MDRD) Study suggest that low-protein diets may slow the progression of kidney disease in CKD Stages 3-4.284 Thus, the Work Group recommended that the DASH diet should not be routinely recommended to patients with a GFR <60 mL/min/1.73 m2 because of its higher protein content. The Atkins Diet (a high protein diet) has been gaining popularity in the United States as a weight-loss diet. However, this diet and others that emphasize high protein intake or protein supplements should not be recommended in CKD.
Patients with CKD are at increased risk for hyperkalemia due to reduced capacity for potassium excretion. The DASH diet contains approximately 4,500 mg/d (approximately 110-115 mEq/d) of potassium compared with a more typical American diet that contains approximately 1,700 mg/d (approximately 40 to 45 mEq/d). Enriched sources of potassium in the DASH diet are fruits, certain vegetables, and fruit juices. Consumption of a diet high in fruits and vegetables may lead to hyperkalemia in patients with CKD (particularly in patients with GFR <60 mL/min/1.73 m2) or with concurrent use of ACE inhibitors, ARBs, or potassium-sparing diuretics. The DASH diet should not be routinely recommended to patients with GFR <60 mL/min/1.73 m2 because of its high content of fruits and vegetables. Certain salt substitutes contain high amounts of potassium salts. Salt substitutes should not be recommended in CKD.
Patients with CKD are at increased risk for bone disease and calcium-phosphate deposits in soft tissues due to reduced capacity for phosphorus excretion. The optimal dietary phosphorus concentration for patients with kidney disease has not been established. The DASH diet is higher in phosphorus (1.7 g/d) than the recommended daily allowance (RDA) of 700 mg/d,283a,284a and higher than is desirable for people with CKD and GFR <60 mL/min/1.73 m2. Recommended maximum phosphorus intake in this group is 0.8 to 1.0 g/d, adjusted to protein intake.285,291 The DASH diet should not be routinely recommended to patients with GFR <60 mL/min/1.73 m2 because of its higher content of phosphorus.
Comparison With Other Guidelines
Table 85 compares diets recommended for the general population, hypertension (DASH diet by JNC 7), diabetes (American Diabetes Association), and hypercholesterolemia (National Cholesterol Education Program). For patients with diabetes, the American Diabetes Association (ADA) diet recommends 10% to 20% of the calories from protein, with lower goals from protein (10% of calories, 0.8 g/kg/d) in those with overt nephropathy (corresponding approximately to CKD Stages 2-5).
There are few controlled trials designed to determine the effectiveness and safety of dietary therapies to lower blood pressure in patients with CKD.
Lifestyle modifications that reduce blood pressure are advocated as part of strategies to prevent and treat hypertension. The current challenge to health-care providers has been developing and implementing practical and effective approaches for use in clinical practice. Physician-directed and office-based treatment of high blood pressure using nonpharmacological strategies can be accomplished, but success is dependent upon several factors, including the skills of the physician and staff, available resources, organizational structure of the office, and a patient’s willingness to change. Important ingredients for success include the education and training of the physician and of office personnel to deliver lifestyle advice and the availability of management algorithms that incorporate available resources (see Guideline 5). Referral to a registered dietitian with experience in counseling patients with CKD is recommended. This is especially important for patients with other indications for dietary modifications, such as diabetes, hyperlipidemia, and obesity.
The Centers for Medicare & Medicaid Services (CMS) has approved coverage for Medical Nutrition Therapy (MNT) services in the outpatient setting for people with CKD (defined as a GFR of 13 to 50 mL/min/1.73m2 and not on dialysis) when a referral is made by a physician to a registered dietitian. Reimbursement has been approved under Medicare Part B on the premise that MNT helps in disease management and will slow the progression to kidney failure. MNT is also covered for patients with diabetes.
(1) Conduct randomized, controlled trials to determine optimal dietary patterns to reduce blood pressure and slow the progression of kidney disease.
(2) Perform research to determine the effects of sodium reduction on blood pressure in patients with CKD.
(3) Conduct outcome studies to determine the effectiveness and value of MNT in CKD.