All antihypertensive agents can be used to lower blood pressure in CKD. Multidrug regimens will be necessary in most patients with CKD to achieve therapeutic goals. Patients with specific causes of kidney disease and CVD will benefit from specific classes of agents.
7.1 Patients with CKD should be considered in the "highest-risk" group for CVD for implementing recommendations for pharmacological therapy, irrespective of cause of CKD (A).
7.2 Target blood pressure for CVD risk reduction in CKD should be <130/80 mm Hg (B).
7.3 Antihypertensive agents should be prescribed as follows, when possible:
7.3.a Preferred agents for CKD should be used first (see Guidelines 8, 9, 10, 11) (A);
7.3.b Diuretics should be included in the antihypertensive regimen in most patients (A).
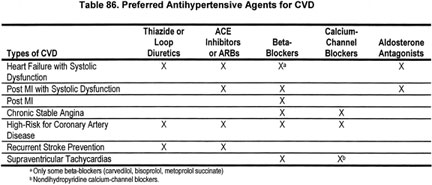
7.3.c Choose additional agents based on cardiovascular disease-specific indications to achieve therapeutic and preventive targets (Table 86) and to avoid side-effects and interactions (B).
7.4 The antihypertensive regimen should be simplified as much as possible (B).
7.4.a Long-acting (once-daily agents) should be used when possible (B).
7.4.b Two agents, either as separate prescriptions or as a fixed-dose combination containing preferred agents, may be considered as initial therapy for SBP >20 mm Hg above goal according to the stage of CKD and CVD risk (C).
7.4.c Fixed-dose combinations may be used for maintenance therapy after the antihypertensive regimen has been established (B).
The goals of antihypertensive therapy in CKD patients are to lower blood pressure, reduce the risk of CVD, and slow progression of CKD. Guideline 7 reviews the use of antihypertensive agents in CKD to lower blood pressure and reduce CVD risk. Use of antihypertensive agents to slow the progression of kidney disease is reviewed in Guidelines 8, 9, and 10.
Numerous studies have documented the high risk of CVD in patients with CKD. There are several reasons for the high risk of CVD—in particular, the older age of patients, the higher prevalence of traditional CVD risk factors (such as hypertension, diabetes and hyperlipidemia), and the presence of CKD-related risk factors such as coronary calcifications from an elevated calcium-phosphorous product. Because of their high risk of CVD, all individuals with CKD are included in the highest-risk group for CVD. A multipronged strategy is necessary to reduce the risk of CVD in this patient population, and hypertension is only one of the therapeutic areas that need to be addressed. The NKF-K/DOQI guidelines on dyslipidemia and bone metabolism will include information on additional strategies to reduce CVD risk in patients with CKD.285a,291
A large number of controlled trials have examined the efficacy of antihypertensive agents on reducing the risk of CVD, and many guidelines have been published on the use of antihypertensive agents to reduce CVD risk. Unfortunately, relatively few patients with CKD have been included in controlled trials of CVD risk reduction. Therefore, recommendations in JNC 6 and other guidelines available at the time of the Work Group review were not developed specifically for patients with CKD. The 1998 report of the Task Force for Cardiovascular Disease in Chronic Renal Disease developed criteria for extrapolation of recommendations on risk factor reduction from the general population to patients with CKD.3 The Task Force concluded that recommendations for target blood pressure and antihypertensive agents in the general population could be extrapolated to patients with CKD.
This section provides a review of the guidelines for the treatment of hypertension as well as a summary of the antihypertensive agents that can be used to achieve these therapeutic goals. "Preferred antihypertensive agents" are defined as antihypertensive agents that reduce CVD risk or slow the progression of certain types of kidney disease by mechanisms in addition to lowering blood pressure. Thus, preferred agents may be indicated in patients either with or without hypertension. The tables included in Guideline 7 show classes of antihypertensive agents and the indications for these agents in CKD, in addition to their effect on blood pressure.
Criteria for Extrapolation of Recommendations From the General Population to CKD
The Work Group adopted the criteria developed by the NKF Task Force on Cardiovascular Disease in Chronic Renal Disease for extrapolating evidence from the general population to the target population (Table 87).
Scope of Work
There are few controlled trials comparing levels of blood pressure or classes of antihypertensive agents to reduce CVD risk in CKD. Thus, the Work Group extrapolated from guidelines of high-risk patients in the general population. The Work Group was convened in 2001, after the release of JNC 6 but prior to the release of JNC 7 in May 2003. The Work Group elected to review recommendations in JNC 6, as well as other guidelines for the treatment of hypertension and CVD that were published since JNC 6. Guidelines were identified by a review of guidelines listed in the National Guideline Clearinghouse (www.guideline.gov). A total of 21 guidelines were retrieved, of which 5 were found not to be relevant for this review. The remaining guidelines are summarized in Table 88.
During the Work Group’s deliberations, results of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) were reported, and JNC 7 was released. Some members of the Work Group (A.S.L. and M.V.R.) were able to review data from a subgroup of ALLHAT participants with CKD (defined as estimated GFR <60 mL/min/1.73 m2), which was later reported in abstract form.292,293 Thus, the Work Group also relied on evidence contained in the ALLHAT report, the ALLHAT CKD subgroup, some of the key clinical trials included in JNC 7, as well as recommendations of JNC 7. Clinical trials in the general population were abstracted or compiled in evidence tables.
The Work Group also summarized information on antihypertensive drug classes in the general population, including indications, recommended doses, contraindications, side-effects, and interactions. In addition to the sources described above, textbooks and reviews were used as source material for this section. Diuretics and beta-blockers are discussed first, since these were the first agents tested in clinical trials of CVD. Newer agents, ACE inhibitors and ARBs, and calcium-channel blockers are discussed next, because there have been a large number of clinical trials in the general population to determine whether these agents are preferred for specific CKD and CVD indications. Agents that act on the alpha-adrenergic system and directly acting vasodilators are discussed briefly. Recently, there has been increased interest in aldosterone antagonists, which are discussed last.
Strength of Evidence
General principles in the use of antihypertensive agents in CKD (Fig 34 and Table 89) (Moderately Strong). All classes of antihypertensive agents are effective in lowering blood pressure in CKD. Figure 34 and Table 89 summarize these principles.
Fig 34. Hypertension and antihypertensive agents in CKD. Superscripts refer to items in Table 89.
Patients with CKD should be considered in the "highest-risk" group for CVD for implementing recommendations for pharmacological therapy, irrespective of cause of CKD (Strong). As noted earlier, patients with CKD have rates of CVD that are 5 to 500 times higher than age- and sex-matched controls in the general population (Fig 4). Thus, it is of the utmost importance to reduce the risk of CVD in patients with CKD.
Target blood pressure for CVD risk reduction in CKD should be <130/80 mm Hg (Moderately Strong). Numerous epidemiological studies show a graded, independent, and strong relationship between the level of arterial blood pressure and CVD. Above a SBP of 115 mm Hg, and above a DBP of 75 mm Hg, the risk of CVD doubles with each increment of SBP of 20 mm Hg or DBP of 10 mm Hg. In persons over age 50, SBP greater than 140 mm Hg is a critical and more important CVD risk factor than DBP.
Controlled trials in essential hypertension conclusively show a beneficial effect of lowering blood pressure to <140/90 mm Hg. Controlled trials in high-risk individuals with diabetes or heart failure suggest beneficial effects of reduction of blood pressure to even lower values. Based on these studies, and on observational studies, a number of guidelines for patients with either diabetes mellitus or congestive heart failure recommend a goal blood pressure of <130/80 mm Hg (Table 88).
There are few studies regarding blood pressure goals for CVD risk reduction in patients with CKD. Thus, the Work Group elected to extrapolate the recommendations for high-risk patients to patients with CKD. Based on the summary of guidelines in Table 88, the Work Group recommendations to reduce the risk of CVD in CKD are an SBP <130 mm Hg and a DBP <80 mm Hg. In certain select cases, it may be appropriate to maintain a blood pressure higher than the recommended goal of <130/80 mm Hg. These conditions include orthostatic hypotension, postprandial hypotension, autonomic dysfunction, and severe peripheral vascular disease that is exacerbated by a blood pressure less than 130/80 mm Hg. Based on studies of the relationship of SBP and kidney disease outcomes reviewed in Guidelines 8 and 9, the Work Group recommended caution in lowering SBP <110 mm Hg and more frequent monitoring in patients treated with antihypertensive agents and SBP <120 mm Hg.
Frequency of monitoring blood pressure in CKD depends on blood pressure level (Weak). Table 90 provides recommendations for frequency of monitoring blood pressure and adjustment of antihypertensive drug regimen, depending on baseline SBP. This protocol has not been studied, but appears reasonable in the opinion of the Work Group.
Some classes of antihypertensive agents are "preferred" for reducing CVD risk and progression of CKD (Strong). A "preferred" agent is a class of antihypertensive agent that has a beneficial effect to reduce the risk of CVD or slow the progression of kidney disease by mechanisms in addition to lowering blood pressure. Preferred agents may be indicated for patients with or without hypertension. In patients with hypertension, a preferred agent should be the initial antihypertensive agent to be used for the specific type of CVD or CKD. Table 86 shows preferred agents to reduce the risk of CVD. Guidelines 8, 9, and 10 review preferred agents to slow the progression of kidney disease.
For each patient, the clinician should determine if there is an indication for a preferred agent based on the type of CKD, coexisting CVD, and other comorbid conditions, and determine the therapeutic goals for each indication. Table 91 lists CKD and CVD indications for classes of antihypertensive agents. In individuals with more than one indication, treatment decisions should be individualized, based on stratification of risk for progression of CKD, reducing the risk of CVD, or other outcomes, as discussed in the Background. If there is no preferred agent for a specific type of CKD or CVD or other condition, then antihypertensive therapy is indicated only if blood pressure exceeds the target level.
Classes of antihypertensive agents (Strong). This section provides an overview of each of the major classes of antihypertensive agents. Table 91 summarizes the CKD and CVD indications for each class of agents. Table 92 summarizes side-effects and contraindications of classes of antihypertensive agents. Tables 93 through 99 list doses of most common agents in each class. More detailed discussions of ACE inhibitors and ARBs and of diuretics are provided in Guidelines 11 and 12, respectively.
Diuretics (Table 93). Fluid retention is one of the major causes of hypertension in CKD. Thus, almost all patients with CKD will require the use of a diuretic in order to achieve the blood pressure goal. Three major classes of diuretics can be used to treat hypertension: thiazide, loop, and potassium-sparing diuretics. Aldosterone antagonists are considered separately. Available thiazide diuretics include hydrochlorothiazide and chlorthalidone.
Thiazide diuretics have a long history of effectiveness in blood pressure reduction and CVD risk reduction.5,5a The purpose of ALLHAT was to compare newer antihypertensive agents to thiazide diuretics, as single agents, in controlling blood pressure and preventing clinical CVD events in high-risk patients with hypertension.107 Altogether, 42,419 patients were randomly assigned to treatment with a thiazide diuretic chlorthalidone, an ACE inhibitor lisinopril, a dihydropyridine calcium-channel blocker amlodipine, or a peripheral alpha blocker doxazosin. Add-on therapy in all groups consisted of beta-blockers, alpha-adrenergic agents, and directly acting vasodilators. The doxazosin arm was stopped early because of an increased risk of nonfatal myocardial infarction. The rates of the primary outcome, coronary heart disease and nonfatal myocardial infarction, were similar among the other treatment arms (Fig 35). Blood pressure control rates were slightly better in patients treated with chlorthalidone (Fig 36), and patients treated with chlorthalidone had lower rates of combined CVD outcomes and heart failure compared to patients treated with lisinopril and lower rates of heart failure compared to patients treated with amlodipine.107,301 Patients treated with chlorthalidone, especially African-Americans, had lower blood pressure and lower rates of stroke than African-Americans treated with lisinopril. Based on these data, JNC 7 recommends a thiazide-type diuretic as the preferred agent to lower blood pressure and to reduce CVD risk in patients at increased risk of coronary heart disease.
Fig 35. Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack (ALLHAT) Trial. Mean systolic and diastolic blood pressure by year during follow-up. Number measured at 6 years for chlorthalidone, amlodipine, and lisinopril are 2,721, 1,656, and 1,551, respectively. Reprinted with permission.107
Fig 36. Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack (ALLHAT) Trial. Cumulative event rates for primary outcome (fatal coronary heart disease or nonfatal myocardial infarction) by treatment group. No significant difference was observed for amlodipine (relative risk [RR], 0.98; 95% confidence interval [CI], 0.90 to 1.07; P = 0.65) or lisinopril (RR, 0.99; 95% CI, 0.91 to 1.09; P = 0.81) versus chlorthalidone with a mean follow-up of 4.9 years. Reprinted with permission.107
ALLHAT included 7,110 patients (17.6% of the total) with an estimated GFR <60 mL/min/1.73 m2 at enrollment, which represents a large "CKD subgroup."302 Analysis of patients with CKD Stage 3 (GFR 30 to 59 mL/min/1.73 m2) assigned to chlorthalidone, lisinopril, or amlodipine (n = 2,492) showed similar findings as in the whole group with respect to CVD.292 In addition, rates of kidney failure, and substantial decline in estimated GFR did not differ significantly among the three drug classes in the CKD subgroup, including analyses stratified by presence or absence of diabetes.293 However, the kidney failure event rate was low (approximately 5%), limiting statistical power for determination of the effect on this outcome.
ALLHAT differs in some important ways from other studies of antihypertensive agents in CKD. First, the ACE inhibitor and dihydropyridine calcium-channel blocker were prescribed without a diuretic. By contrast, other studies in CKD have compared classes of antihypertensive agents usually prescribed in combination with a diuretic. Second, the risk of kidney failure was lower than observed in other studies in CKD. Third, proteinuria was not measured in ALLHAT, either in baseline or in follow-up. By contrast, most studies in CKD have included patients with proteinuria. Thus, differences between ALLHAT and other studies in CKD may be due to the study design and the type of patient enrolled, rather than true differences in efficacy of combinations of antihypertensive agents used in CKD in slowing progression of kidney disease.
Loop diuretics have not been studied in large hypertension trials in the general population; thus, their effectiveness in reducing CVD risk is not known. However, they are effective in reducing ECF volume and have been used in combination with other antihypertensive agents in many studies in CKD. Loop diuretics have a shorter duration of action than thiazide diuretics; hence, they are less effective in patients with normal kidney function, unless they are given in multiple daily doses.303,304 However, since thiazide diuretics are of minimal effectiveness for ECF volume reduction at low levels of GFR,305 a loop diuretic is preferred for this purpose in patients with GFR less than 30 mL/min/1.73 m2. Patients with resistance to loop diuretics may benefit from a combination of a loop diuretic with metolazone, which has a mechanism of action at several sites in the renal tubule.306 As in patients without CKD, volume depletion may occur from the use of diuretics.
Thiazide and loop diuretics increase the delivery of sodium to the distal tubule, thereby increasing urinary potassium excretion. This may be a useful side-effect in CKD, especially in patients treated with an ACE inhibitor or ARB. Nonetheless, hypokalemia can occur, and if not treated appropriately, poses the same potential risks as in patients without CKD. Other side-effects of thiazide and loop diuretics include hyperuricemia and gout, hyperglycemia, and increased LDL cholesterol.
Potassium-sparing diuretics, triamterene and amiloride, are less effective as single agents in reducing ECF volume than thiazide and loop diuretics. They are generally used as an adjunct to thiazide and loop diuretics for prevention and treatment of diuretic-induced hypokalemia and in patients with edematous states. They are generally not used as antihypertensive agents in patients with CKD due to the increased risk of hyperkalemia. Aldosterone antagonists also act as potassium-sparing diuretics and can be used in the same circumstances as triamterene and amiloride.307
Beta-adrenergic blockers (Table 94). There are several classes of beta-blockers that differ in both clinical benefits and adverse effects. First, beta-blockers can be classified based on their effect on alpha and beta adrenergic receptors. Beta-1 receptors are found mostly in heart muscle. Activation of beta-1 receptors results in an increase in AV nodal conduction, contractility, and heart rate as well as a decrease in AV node refractoriness. Beta-2 receptors are found in bronchial and peripheral vascular smooth muscle in higher numbers than in heart muscle. Activation of beta-2 receptors results primarily in vasodilatation and bronchodilation. Selective beta-blockers are those agents that preferentially block the beta-1 receptor, while nonselective beta-blockers block both the beta-1 and beta-2 receptors. Due to their effect on beta-2 receptors, nonselective beta-blockers can cause bronchoconstriction and worsening of symptoms of severe peripheral vascular disease and can mask signs of hypoglycemia that are sympathetically mediated. These side-effects can also be seen when selective beta-blockers are used in high doses.
Beta receptors also stimulate cellular uptake of glucose and potassium. Beta-blockers can cause hyperkalemia due to altered transcellular distribution of potassium. Selective beta-blockers may cause lesser elevation in serum potassium than nonselective beta-blockers. All beta-blockers can cause an increase in serum levels of plasma glucose and triglyceride levels and in insulin resistance and a decrease in HDL cholesterol levels.308
Some beta-blockers also block the alpha receptor, and they may share some properties with alpha blockers, as described below. Both labetolol and carvedilol block beta receptors nonselectively and also block alpha receptors. Other beta-blockers have intrinsic sympathomimetic activity (ISA), causing activation of the beta-receptor, while also preventing catecholamines from binding to the receptor site. Acebutolol and pindolol have ISA. These agents may be associated with an increased risk of arrhythmias due to beta-receptor stimulation.
Second, beta-blockers can be classified by their solubility properties and routes of metabolism. Lipid soluble beta-blockers are eliminated by hepatic metabolism, have a short half-life, and do not require dose adjustment in CKD. However, their metabolism is slowed in heart failure and in the elderly, and they can accumulate causing an increased incidence of side-effects. In addition, they can enter the central nervous system in high concentrations, and are associated with a higher incidence of insomnia, hallucinations, nightmares and depression. Propranolol and metoprolol are examples of lipid soluble beta-blockers.
Water-soluble beta-blockers are excreted by the kidney, have a longer half-life, and may accumulate in CKD. They do not readily enter the CNS. Atenolol and sotalol are water soluble. Esmolol has a half life of less than 10 minutes due to rapid metabolism by both hepatic esterases and blood tissue.
Beta-blockers were often used in combination with thiazide diuretics in early clinical trials.5,15 However, without diuretics, the effects have been mixed.309 In the Medical Research Council trial of middle-aged patients with a diastolic blood pressure between 90 and 109 mm Hg, there was no difference in overall outcome between patients receiving either a thiazide diuretic or propranolol.310 Carvedilol, extended release metoprolol, and bisprolol are effective agents for the treatment of both essential hypertension and congestive heart failure.311-313 The results of trials comparing beta-blockers to other agents are discussed in subsequent sections.
Thus, beta-blockers are beneficial in patients with a prior history of angina, myocardial infarction, congestive heart failure (due to diastolic dysfunction and for certain agents also for systolic dysfunction), resting tachycardia, migraine headaches, and glaucoma.15,314,315 Conversely, beta-blockers should in general not be used in patients with bradycardia, second- or third-degree heart block, asthma, chronic obstructive pulmonary disease, severe peripheral vascular disease, or depression, as ß-adrenergic tone is beneficial in these circumstances.15,316,317 In addition, beta blockade may mask some of the early symptoms of hypoglycemia. Finally, propranolol can interact with a number of other medications, due to metabolism of propranolol by the cytochrome P-450 system and by decreasing hepatic blood flow.318-320 Other beta-blockers may also be substrates for cytochrome P-450 system interactions.321 In addition, the abrupt withdrawal of most (and perhaps all beta-blockers) can lead not only to rebound hypertension, but also to worsening angina, myocardial infarction, and even death.322-324 The mechanism of action is felt to be increased sympathetic activity due to adrenergic receptor upregulation during the period of sympathetic blockade.325
ACE inhibitors and ARBs (Table 95). ACE inhibitors and ARBs have many potential advantages for patients with CKD and associated comorbid medical conditions.326 As discussed in Guidelines 8 and 9, they slow the progression of diabetic kidney disease and nondiabetic kidney disease with proteinuria, and in addition, they reduce proteinuria, irrespective of the type of kidney disease.139,316,327-339
There is widespread agreement on the beneficial effect of ACE inhibitors and ARBs in heart failure340-344 and in patients with postmyocardial infarction.345-348 It is suggested that they regress LVH more effectively than other classes of antihypertensive agents.349
ACE inhibitors and ARBs may have a beneficial effect in preventing heart disease in high-risk patients. In the Captopril Prevention Project (CAPP), patients with a DBP of ≥100 mm Hg were randomly assigned to either captopril or a beta-blocker (the latter with or without a diuretic). There was no difference between the two groups in regard to the event rate for either fatal or nonfatal myocardial infarction.350 A subsequent subgroup analysis found that patients with diabetes mellitus, however, had a 40% reduction in the relative risk of all primary endpoints if they were randomized to the captopril group.351 In the HOPE trial, patients aged >55 years with diabetes and one or more CVD risk factors, or without diabetes but a history of CVD, had improved survival when treated with an ACE inhibitor.352 These findings are in contrast to ALLHAT, where lisinopril had a higher rate of combined CVD outcomes, stroke, and heart failure compared to patients treated with chlorthalidone.107 In low-risk patients, the Second Australian National Blood Pressure Study (ANBP2) showed a reduced risk of CVD in patients treated with an ACE inhibitor compared to a diuretic.352a
Beneficial effects in stroke prevention remain controversial. In CAPP, there was a mild increase in the risk of stroke in the group receiving captopril.350 The Losartan Intervention for Endpoint reduction (LIFE) study randomly assigned patients with markedly elevated blood pressures (SBP of 160 to 200 mm Hg and DBP of 95 to 115 mm Hg) and evidence of LVH on electrocardiogram to either losartan or atenolol therapy. The losartan group had a lower rate of the primary endpoint of cardiovascular death, myocardial infarction, or stroke compared to the atenolol group.134 This reduction in the primary endpoint was more pronounced in patients with diabetes mellitus.353
ACE inhibitors and ARBs have fewer metabolic side-effects than diuretics and beta-blockers. They do not cause ECF volume depletion or changes in serum cholesterol, triglyceride, or plasma glucose levels.354 However, they have other side-effects that limit their use. They cannot be used in pregnant women due to risks to the fetus.355 ACE inhibitors can cause a dry cough or angioedema due to inhibition of converstion of bradykinin to inactive metabolites. ARBs have a decreased incidence of cough and can be used in patients who do not tolerate an ACE inhibitor because of cough. Both ACE inhibitors and ARBs can cause hyperkalemia and mild decrease in GFR in CKD. The uses and side-effects of ARBs are discussed in more detail in Guideline 11.
Calcium-channel blockers (Table 96). The calcium-channel blockers can be subdivided into dihydropyridine and nondihydropyridine agents. The dihydropyridines preferentially block L-type calcium channels. They are potent vasodilators with little or no effect on cardiac contractility or cardiac conduction. The nondihydropyridines include verapamil, a cardiac depressant, and diltiazem, which has both mild vasodilator and cardiac depressant activity. In general, calcium-channel blockers are of particular benefit in patients with angina pectoris, recurrent supraventricular tachycardia (verapamil only), Raynaud’s phenomenon (dihydropyridines only), congestive heart failure due to diastolic dysfunction, migraine headaches, and esophageal spasm.356 Neither class causes an increase in cholesterol or triglyceride levels or in insulin resistance.308
The nondihydropyridine calcium-channel blockers have beneficial effects on CKD and CVD. As discussed in Guidelines 8 and 9, diltiazem and verapamil are effective in decreasing proteinuria in diabetic kidney disease.337,357-359 In addition, the combination of lisinopril and verapamil resulted in a greater reduction in proteinuria than using either drug at twice the dose used in combination therapy.358 Similar findings were seen with a combination of trandolapril and verapamil.360 A nonsignificant effect of ve rapamil on mortality was seen in the Danish Ve rapamil Infarction Trial II (DAVIT II) study in patients after myocardial infarction without a history of congestive heart failure.361 In two studies, CONVINCE362a and INVEST,362 including more than 38,000 hypertensive patients, CVD mortality was similar in the calcium-channel blocker and beta-blocker arms. In the Multicenter Diltiazem Post Infarction Trial Research group study, post-MI patients randomized to diltiazem (versus placebo) showed a nonsignificant trend for lower mortality in patients who did not have evidence of pulmonary congestion on chest x-ray. Conversely, there was an excess of deaths in diltiazem-treated patients with pulmonary congestion.363 In the Nordic Diltiazem (NORDIL) trial, more than 10,000 patients with diastolic blood pressure greater than 100 mm Hg were randomly assigned to either diltiazem or standard therapy, consisting of a diuretic, a beta-blocker, or both agents. There was no difference in the rate of the primary combined endpoint of stroke, myocardial infarction, or other cardiovascular death between the two randomized groups. Secondary analyses suggested, however, that the rate for stroke alone was less in the diltiazem group than in the beta-blocker and/or diuretic group.364
Nondihydropyridine calcium-channel blockers can diminish cardiac contractility and slow cardiac conduction.356 Therefore, these agents should not be used in patients with severe left ventricular dysfunction, sick sinus syndrome, or second- or third-degree heart block.365 In addition, constipation can be seen in up to 25% of patients prescribed verapamil.356
In ALLHAT, patients treated with amlodipine had a higher rate of heart failure compared to patients treated with chlorthalidone.107 In addition, in the Appropriate Blood Pressure Control in Diabetes (ABCD) trial, hypertensive diabetic patients who were treated with nisoldipine had a higher risk of fatal and nonfatal myocardial infarction compared to patients treated with enalapril.366 In the Intervention as a Goal in Hypertension Treatment (INSIGHT) study, patients with hypertension and at least one other cardiovascular risk factor were randomized to either amiloride with hydrochlorothiazide versus nifedipine Gastrointestinal Therapeutic System (GITS). There was no difference in the primary outcome of cardiovascular death, myocardial infarction, heart failure, or stroke between the two randomized groups. However, there was an increase in the rates of fatal myocardial infarction and nonfatal heart failure in the group receiving nifedipine GITS.367 Finally, in the Fosinopril Amlodipine Cardiovascular Events Trial (FACET) trial, patients prescribed amlopidine had increased cardiovascular complications compared to patients prescribed fosinopril.368 In contrast, the Syst-Eur369 and Syst-China370 studies showed a decrease in both fatal and nonfatal coronary events in patients prescribed nitrendipine. In the Hypertension Optimal Treatment (HOT) trial, a lower coronary event rate was seen in patients prescribed a higher dose of felodipine.371 Overall, controlled trial results are not altogether consistent, but it appears that dihydropyridine calcium-channel blockers, in association with a diuretic, are effective in lowering blood pressure and reducing CVD risk, but are less effective in the absence of a diuretic.
There are a number of dihydropyridine agents. Some have cardiac depressant activity, such as short-acting nifedipine, and longer-acting felodipine, isradipine, nicardipine, nisoldipine, and long-acting nifedipine. Long-acting agents that do not have cardiac depressant effects include amlodipine and lacidipine. In general, longer acting agents without cardiac depressant effects are preferred.
The dihydropyridines are associated with a number of other side-effects due to direct vasodilatation and can cause peripheral edema, dizziness, headache, and flushing.356 In one study there was less edema when dihydropyridines were used in combination with ACE inhibitors compared to use of dihydropyridines alone.372
Alpha-adrenergic agents (Table 97). Both centrally acting sympatholytic agents (methyldopa, clonidine, guanfacine and guanabenz) and selective a-1 blockers have beneficial effects on lipid metabolism (increase HDL cholesterol levels and decrease LDL cholesterol levels) and improve insulin sensitivity. In general, these agents should not be used as a first-line therapy for hypertension due to the relatively high incidence of side-effects. Side-effects of the centrally acting agents include dry mouth, sedation, and sexual dysfunction373 and for clonidine, side-effects are rebound hypertension after sudden discontinuation of therapy325 and sometimes even with gradual withdrawal of therapy.374,375 Side-effects of the selective a-1 blockers include headache, weakness, dizziness, and—on rare occasions—syncope. Dizziness and syncope can be minimized by starting with a low dose of a long-acting agent such as doxazosin and administering the initial dose at bedtime.376 The selective a-1 blockers may be of benefit in men with symptomatic benign prostatic hyperplasia. This benefit is balanced by the observation in ALLHAT that the use of doxazosin increased the risk of developing congestive heart failure compared to patients treated with the diuretic chlorthalidone.377
Peripheral vasodilators (Table 98). Minoxidil is a powerful vasodilator that can cause lower extremity edema, tachycardia, hirsutism, and—in rare cases—pleural or pericardial effusions, at therapeutic doses.378 The incidence of pericardial effusion in CKD patients is higher than that seen in the general population.379-381 This agent is almost always used in combination with a beta-blocker and loop diuretic in order to minimize reflex tachycardia and lower extremity edema. In one controlled trial of captopril versus minoxidil, improvement in blood pressure in the captopril group resulted in regression of LVH at 6 months while regression did not occur in the minoxidil-treated group.382 Therefore, minoxidil should be reserved for those patients who cannot obtain blood pressure control with the preferred agent and at least two of the other recommended agents.
Aldosterone antagonists (Table 99). Aldosterone plays a role in numerous cardiovascular effects, such as LVH, CHF, and vascular fibrosis, necrosis, and inflammation. Aldosterone receptor antagonists can be classified as "selective" (blocking the mineralocorticoid receptor) or "nonselective" (blocking the glucocorticoid, progesterone, and androgen receptors as well as mineralocorticoid receptors). Recently, aldosterone receptor antagonists have been identified as a treatment for congestive heart failure. In the Randomized Aldactone Evaluation Study (RALES), patients receiving the nonselective agent spironolactone compared to those receiving placebo had a reduction in mortality of 30%.383 Small doses of spironolactone resulted in an improvement in ventricular function and enhanced exercise tolerance. In the Eplerenone Post–Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS), patients with a left ventricular ejection fraction of 40% or lower and symptoms of heart failure were randomly assigned to receive the selective agent eplerenone an average of 7 days after they had had a myocardial infarction or placebo.384 During a mean follow-up of 16 months, the relative risk of death was reduced by 15% among patients receiving eplerenone and the risk of hospitalization for heart failure was reduced by 15% with eplerenone.385 There was a significantly greater increase in the serum creatinine concentration in the eplerenone group than in the placebo group, however, and hyperkalemia occurred in 5.5% of patients in the eplerenone group, as compared with 3.9% of patients in the placebo group. However, the study included only patients with CKD Stages 1-2. Side-effects are likely to be more frequent in CKD Stages 3-5.
Guidelines from the American Heart Association and the American College of Cardiology recommend considering low-dose spironolactone in patients with recent or current symptoms of systolic heart failure at rest despite the use of digoxin, diuretics, an ACE inhibitor, and a beta-blocker.300 These guidelines urge caution in prescribing spironolactone to patients with baseline elevations of either serum potassium or creatinine. In animal models, it appears that aldosterone receptor antagonists reduce proteinuria, nephrosclerosis, and glomerulosclerosis; however, clinical trials using these agents in patients with CKD have only recently been initiated.386 Thus, caution should be used when these agents are prescribed in patients with CKD.
Initiation and selection of antihypertensive agents in CKD (Moderately Strong). The algorithm in Fig 34 illustrates decision-making in initiation and selection of antihypertensive agents in CKD.
Initiation of therapy and dose-escalation with preferred agents. In patients not previously treated with antihypertensive agents, an agent from the preferred class for CKD is the first agent to be used (generally on ACE inhibitor or ARB). In patients already treated for CKD with other antihypertensive agents or other medications that lower blood pressure, an agent from the preferred class should be added to the regimen. Other agents may need to be reduced in dosage or discontinued in order to add the preferred agent. In patients already treated with an agent from the preferred class, consideration should be given to increasing the dosage. This may require reduction in dosage or discontinuation of other agents.
Monitoring the response to preferred agents. After the initiation of therapy, patients should be monitored for effects on blood pressure, for kidney function, and for agent-specific side-effects. Detailed protocols for monitoring response to ACE inhibitors and ARBs and to diuretics are given in Guidelines 11 and 12, respectively. An often-used "rule of thumb" is that addition of a new antihypertensive agent in appropriate dosage lowers systolic blood pressure by approximately 10 mm Hg. If blood pressure does not decline, then the clinician should consider nonadherence to medications or the use of medications that can raise blood pressure. A list of strategies to improve adherence is shown in Table 100, and a list of medications that can raise blood pressure is shown in Table 101. After exclusion or correction of these causes, the dose of the preferred agent should be increased. Dosage should not be escalated more frequently than every 4 weeks.
If the response to the preferred agent does not achieve the desired blood pressure response, then a diuretic is usually added as the second agent, and the dose is increased until the patient is euvolemic, target blood pressure is achieved, adverse effects are noted, or a high dose has been reached. A diuretic should be considered in patients for whom a single agent does not achieve blood pressure target even if there is no evidence on physical examination of volume overload. Thiazide diuretics are preferred in patients with GFR ≥30 mL/min/1.73 m2 because of their longer duration of action. Loop diuretics are preferred in patients with GFR <30 mL/min/1.73 m2, but may need to be given twice daily to achieve the desired natriuresis. Higher doses of loop diuretics are required in patients with lower GFR. Potassium-sparing diuretics should be avoided in patients with GFR <30 mL/min/1.73 m2 and in patients taking ACE inhibitors or ARBs. See Guideline 12 for a more detailed discussion on the use of diuretics in CKD.
Addition of other agents. Additional agents are selected based on CVD-specific indications to achieve therapeutic and preventive targets, and on avoidance of drug interactions or known side-effects (Table 86). Many patients with CKD, especially those with a GFR <30 mL/min/1.73 m2, require three or four antihypertensive agents in order to reach the desired blood pressure goals.387 Some antihypertensive agents have adverse interactions and should be used in combination with caution (Table 102). In addition, there are also a few specific instances where a combination of specific antihypertensive agents has been shown to be beneficial in specific patient populations. Additional antihypertensive agents should be started one at a time, at the lowest recommended dose, then escalated at intervals of 4 to 8 weeks until either the desired blood pressure goal is achieved, a high dose is reached, or a side-effect occurs.
The antihypertensive regimen should be simplified as much as possible (Moderate). Patients have been shown to have a lower rate of compliance with medications prescribed once per day compared to medications prescribed more than once per day. In addition, antihypertensive medications that have a half-life of greater than 24 hours are more likely to sustain a significant and sustained decrease in blood pressure over a 24-hour period compared to antihypertensive medications with a half-life of less than 24 hours.
In patients who are at least 20 mm Hg above their goal blood pressure, it is unlikely that a single agent will be effective in reaching the target blood pressure, even at maximal dosages. In these situations, it may be beneficial to initiate therapy with two agents either as separate prescriptions or as a fixed-dose combination containing a preferred agent as initial therapy.5,5a For patients with GFR >30 mL/min/1.73 m2, a preferred agent in combination with a thiazide diuretic is often an appropriate choice.
After therapeutic goals are reached, it may be more convenient to change to a fixed-dose, once-daily combination of antihypertensive agents. Pharmaceutical companies produce a variety of combination antihypertensive agents. These combinations can be used to simplify the antihypertensive regimen and are shown in Table 103.
There are few studies on the treatment of hypertension in CKD. Most of the largest clinical studies in patients with CKD were designed to evaluate the efficacy of therapy in slowing the progression of CKD rather than reducing risk of CVD. Therefore, most of the recommendations in Guideline 7 are extrapolated from clinical studies performed in the general population.
Data from NHANES III document the low rate of control of hypertension in CKD (Figs 3, 4, and 5). The problem of attaining high rates of adherence to antihypertensive therapy for CKD is similar in many ways to that in the general population, in which careful studies report adherence with declared, desirable outcomes in only 50% to 60% of patients.5,5a In particular, it is necessary to develop the appropriate framework for description, as well as for intervention.
The control of hypertension in the individual patient clearly involves difficulties of measurement and response to treatment.388-390 These are reflected in the statistical description of any given patient population, which is the currency of reporting clinical outcomes at facility/practice level. Systolic blood pressure values follow an approximately Gaussian distribution in most populations, with standard deviations (SD) that are typically 15 mm Hg or more. Because of the variability of values and a relatively fixed dispersion of blood pressure levels, a high rate of adherence to guidelines must necessarily involve mean/median population values well below the desired goal. The percentage achievement of goal blood pressure level depends on these outcome distributions for any patient population. Therefore, the lower the mean, the higher the percent adherence rate.
For example, since about 85% of patients can be expected to be one SD above the mean, for a performance measure that "85% of patients should have a blood pressure <130 mm Hg," then the mean systolic blood pressure for the population might need to be <115 mm Hg (130 - 15 = 115 mm Hg). These statistical determinants of overall (population) performance are not generally included in guideline statements. Furthermore, there is no generally accepted vocabulary for the values below the goal blood pressure level that are necessary to achieve adherence to performance measures for a clinical population, nor for the yet lower values that would act as prompts in an individual patient to achieve adherence at the population level. This problem becomes even more complicated if one takes into account time-to-time variability in individuals.
Clinicians will need to adopt an appropriate system for monitoring individual patients in regard to achieving treatment goals, evaluating for ECF volume overload, and evaluating for potential adverse effects. Members of the health care team will need to be assigned specific roles. In addition, it is likely that a systematic approach will be necessary to review patient medications. Several software programs are available that will check a list of patient medications for potential drug interactions. Pharmacists are a valuable resource for identifying potential drug interactions, interpreting the clinical relevance of known interactions, and developing and monitoring plans based on pharmcodynamic and pharmacokinetic characteristics of individual agents.391-394 Patients need to be instructed to call their physician if they develop volume overload or worsening blood pressure control between clinic visits. This latter point is of particular importance to patients with CKD as worsening kidney function can lead to either of these complications. Patients will also need to be instructed in the possible adverse effects for each of the antihypertensive agents that are prescribed to them. Socioeconomic issues must be considered.
Additional clinical studies are needed on the treatment of hypertension in patients with CKD. The variation in blood pressure within the population and the time-to-time variation in blood pressure within an individual need to be determined to permit definition of the blood pressure goal for the population. The effect of blood pressure control on rates of CVD in patients with CKD needs to be ascertained. A comparison of the effects of different antihypertensive agents on cardiovascular events in patients with CKD needs to be determined.