In Patients with CKD Stages 2-4:
6.1 If serum phosphorus levels cannot be controlled within the target range (see Guideline 4), despite dietary phosphorus restriction (see Guideline 5), phosphate binders should be prescribed. (OPINION)
6.2 Calcium-based phosphate binders are effective in lowering serum phosphorus levels (EVIDENCE) and should be used as the initial binder therapy. (OPINION)
In Patients with CKD Stage 5 (Dialysis):
6.3 Both calcium-based phosphate binders and the non-calcium, non-metal-containing phosphate binders, such as sevelamer HCL, are effective in lowering serum phosphorus levels. (EVIDENCE) As of this writing, calcium-based phosphate binders should be used as primary therapy in infants and young children. In older children and adolescents, either drug may be used. (OPINION)
6.4 In dialysis patients who remain hyperphosphatemic (above the upper target value) despite the use of either calcium-based phosphate binders or other noncalcium, non-metal-containing phosphate binders, the dialysis prescription should be modified to control hyperphosphatemia. (OPINION)
6.5 The total dose of elemental calcium provided by the calcium-based phosphate binders and dietary calcium should not exceed up to 2X DRI for calcium, based on age (OPINION), and the total intake of elemental calcium (including dietary calcium) should not exceed 2,500 mg/day. (OPINION)
6.6 The dosage of calcium-based phosphate binders should be lowered in dialysis patients with corrected serum calcium of >10.2 mg/dL (2.54 mmol/L), or with serum PTH levels <150 pg/mL (16.5 pmol/L) on two consecutive measurements. (EVIDENCE)
6.7 In adolescent patients with serum phosphorus levels >7.0 mg/dL (2.26 mmol/L), aluminum-based phosphate binders may be used as a short-term therapy (up to 4-6 weeks), and for one course only, to be replaced thereafter by other phosphate binders. (EVIDENCE)
6.8 In children receiving aluminum-based phosphate binders, concurrent use of citrate-based products should be avoided, due to the risk of increasing aluminum absorption and potential toxicity. (EVIDENCE)
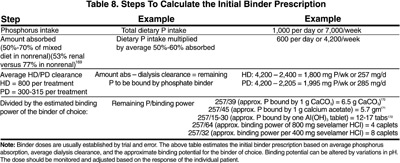
When dietary phosphate restriction is inadequate to control serum levels of phosphorus and/or PTH, phosphate binders should be administered. Different phosphate binder compounds have been utilized to control serum phosphorus levels, but the search still continues for the best possible binder. A combination of binders may be used to control serum phosphorus levels to minimize the potentially serious side-effects of any specific binder. The willingness of the patient to adhere to the binder prescription is paramount to control phosphorus absorption from the gastrointestinal tract and, subsequently, serum phosphorus levels. Table 8 describes the steps to calculate the initial prescription of phosphate binders, and Table 9 describes the characteristics of various phosphate-binding agents.
In children, calcium-based phosphate binders have been shown to be safe and effective.158-162 Recently, pediatric experience with sevelamer HCl is accumulating, and it appears to be safe and effective as well.163a Long-term use of aluminum-containing phosphate binders has been associated with severe complications of bone disease and encephalopathy.164-166 Thus, only a short-term course (4-6 weeks) of aluminum can be recommended for control of hyperphosphatemia. Data demonstrate that concurrent administration of citrate containing compounds dramatically increases enteral absorption of aluminum and must be avoided if aluminum-containing phosphate binders are used.167,168
The goal of phosphate-binder therapy is to maintain serum phosphorus levels within the range as outlined in Guideline 4 without adversely affecting nutritional status or causing serious side-effects. It is recommended to initiate phosphate binder therapy when: (a) serum phosphorus levels remain elevated, despite restriction of dietary phosphate restriction; or (b) the restriction of phosphate intake hinders the intake of other critical nutrients.
The majority of research in the recent decade has focused on calcium-based binders, which have been shown to be safe and effective in children with CKD. Recently, other non-calcium, non-metal containing, binder forms are available, but are incompletely studied in children. With recent concern that soft-tissue calcification may be worsened by calcium-based phosphate binders and vitamin D analogs, noncalcium, nonaluminum binders are being used more frequently in adults with CKD. As further data on efficacy and safety in children accumulate, it is expected that the frequency of use will increase for children with CKD.
An increase in the frequency of dialysis can enhance phosphorus clearance in hemodialysis patients.176 Among patients treated with thrice-weekly nocturnal hemodialysis, serum levels of phosphorus were reduced despite increased dietary intake and reduced use of binders.177 Some patients treated with nocturnal dialysis six times per week have required phosphate supplements in the dialysate to correct hypophosphatemia.178 Where the escalation of phosphate-binder dose is either incapable of controlling serum phosphorus levels or is not tolerated, modification of the dialysis prescription in both hemodialysis and peritoneal dialysis patients should be strongly considered to improve phosphate clearance. During the use of aluminum-based phosphate binders, patients should be monitored to avoid additional morbidity described with their prolonged use179,180 (see Guidelines 12 and 13).
Studies of the efficacy and safety of phosphate binders in children with CKD Stages 3-4 are limited to uncontrolled case series.160,161,181 Three studies reported effective control of phosphorus with calcium carbonate160,161,181; the largest series reported treatment in 45 children with a follow-up period of 6-54 months.160 All subjects were on a phosphate-restricted diet and 42 were also treated with vitamin D sterols; transient hypercalcemia occurred in 11 patients. The two smaller series161,181 also reported transient hypercalcemia that responded to adjustments in vitamin D and binder doses. The required doses of calcium carbonate ranged widely, from 64-1,578 mg/kg/day in one study,161 to 21-228 mg/kg/day in another.160 One study provided data on the absolute dose of elemental calcium required to control PTH: 240-6,000 mg elemental calcium per day.161
Additional case series have been published in children with CKD Stage 5.159,162 One of these suggested that episodes of hypercalcemia were more common in children with a history of prior aluminum therapy.159 Another study reported a comparison of calcium acetate with calcium carbonate in nine hemodialysis patients.158 Calcium carbonate was administered for 7 weeks, followed by withdrawal of therapy; then calcium acetate was administered for an additional 7 weeks. Both agents lowered the serum phosphorus concentration significantly. Although significantly less elementary calcium was ingested with calcium acetate (mean 750 [range 375-1,500] mg calcium/day) than with calcium carbonate (mean 1,200 [range 0-3,000] mg calcium/day), the number of episodes of hyperphosphatemia or hypercalcemia did not differ between treatments.
Studies that evaluated the efficacy and adverse effects of phosphate binders were analyzed. There were no prospective, controlled studies that evaluated phosphate binders in CKD Stages 3 and 4. However, since serum PTH levels in these patients are elevated in association with hyperphosphatemia, it is the opinion of the Work Group that the use of phosphate binders may become necessary if the serum levels of PTH cannot be lowered to the target levels (see Table 3, Guideline 1) by dietary phosphate restriction and/or vitamin D therapy.
In CKD Stage 5, there were 16 prospective, controlled studies in adults that evaluated 552 patients for various outcomes to quantify the efficacy of serum phosphorus control by phosphate binders. In all these studies, the patients were treated with dialysis and the primary focus of the analysis was on the use of calcium carbonate and calcium acetate, although some data on aluminum hydroxide, calcium gluconate, calcium carbonate plus magnesium carbonate, and sevelamer HCl were also available. A meta-analysis of these studies was performed to compare the efficacy of the phosphate binders on outcomes, including: serum levels of phosphorus, PTH, and calcium; bone biochemical markers; and extraskeletal calcification.173,182,183 No studies evaluated the effect of phosphate binders on patient quality of life, mortality rate, incidence of bone disease or fractures. Recently, the use of both calcium based binders and non-calcium, non-metal containing P binders, such as sevelamer HCL, have been shown to be effective phosphate binders in children on peritoneal dialysis and bone biopsy proven secondary hyperparathyroidism.163a Furthermore, the skeletal lesions of high-turnover bone disease markedly improved with both binders and active vitamin D sterols. However, therapy with sevelamer HCL allows the use of higher doses of active vitamin D without increments in serum calcium levels.163a
Effect on Phosphorus
In all studies, serum phosphorus was lowered by the phosphate binder studied. In assessing the relative efficacy of the various phosphate binders in controlling serum phosphorus levels, 15 studies were evaluated: nine studies examined calcium carbonate and six examined calcium acetate. Two sets of meta-analyses were performed. The first analysis compared the relative effectiveness of various phosphate binders to that of calcium carbonate and no significant difference was observed. The second meta-analysis compared calcium acetate to a variety of phosphate binders.182,184-188 It showed that calcium acetate decreased serum phosphate levels to a greater degree than the other phosphate binders, although it should be emphasized that the “other” phosphate binders group was a mixture of different phosphate binders such that this comparison may not be completely valid. A subgroup analysis of four studies that directly compared calcium carbonate to calcium acetate185-188 found that post-treatment serum phosphate levels were significantly higher following treatment with calcium carbonate compared to calcium acetate (Figure 5). One possible explanation for this difference is that calcium acetate leads to less hypercalcemia (see below), thereby allowing more binder to be administered to control phosphorus better.
Fig 5. Meta-Analysis of Size of Effect on Serum Phosphorus Levels of Calcium Acetate versus Calcium Carbonate
Fig 6. Meta-Analysis of Size of Hypercalcemic Effect of Calcium Carbonate versus Other Phosphate Binders
Two studies included a placebo group for comparison against calcium acetate173 and sevelamer,189 and both showed that efficacy of these binders was superior compared to placebo.
A single study evaluated magnesium as a phosphate binder: it was a crossover study that evaluated patients on calcium carbonate compared to a combination of calcium carbonate and magnesium carbonate.190 The magnesium arm had equivalent phosphorus control. However, the Work Group cautions that, in this study, the magnesium concentration in the dialysate was decreased. This is difficult to do in most units due to centralized dialysate delivery systems. Furthermore, there are no long-term studies on the safety and efficacy of magnesium as a phosphate binder, and thus the Work Group agreed that the use of magnesium-based phosphate binders may be justified only if all other compounds fail and the appropriate precautions are undertaken.
Effect on Calcium and CaXP
Ten studies evaluated the effect of different phosphate binders on corrected serum calcium levels, ionized calcium, total calcium, or CaXP.173,185-189,191-194 Five of these studies compared different binders to calcium carbonate,173,186,187,190,193 but a meta-analysis failed to detect a difference in the corrected serum calcium levels. A placebo-controlled study found higher total calcium levels and lower CaXP in the calcium acetate-treated group compared to placebo.173 Although the overall change in serum calcium levels in 10 studies was not affected, meta-analysis of the data showed that calcium carbonate led to more hypercalcemic events compared to other phosphate binders, or when directly compared to calcium acetate only (Figure 6).183,185-188,190,192-195 Six studies assessed calcium-phosphorus product, one placebo-controlled and the others comparing different phosphate binders. Differences were observed in only two of these studies. Calcium acetate led to a lower calcium-phosphorus product than placebo,173 and calcium carbonate led to a greater product than calcium ketoglutarate.194 This latter study found that ionized calcium levels were higher in patients treated with calcium carbonate compared to calcium ketoglutarate.194 Thus, the available data do not provide guidance regarding the choice of the appropriate calcium-based phosphate binder. The choice is a prerogative of the physician and depends on the patient's tolerance of the binder.
Other Outcomes
The major side-effects observed as a result of phosphate-binder therapy were hypercalcemia, as described above, or gastrointestinal side-effects. A meta-analysis indicated that gastrointestinal side-effects were lowest with patients treated with calcium carbonate compared to other binders, although the effect size was small and thus no firm conclusions could be reached.186,188,190,192,194,195
Six studies evaluated the effect of phosphate binders on nutritional outcomes,182,184,189-191,194 but different outcome measures were utilized, precluding comparative analyses. Two studies found that sevelamer HCl led to lower serum cholesterol levels compared to placebo or calcium acetate, primarily due to a decrease in LDL cholesterol levels.184,190 In addition, sevelamer HCL allows the use of higher doses of active vitamin D without inducing changes in serum calcium levels.163a
Patient compliance with prescribed binder therapy was not reported consistently, but ranged from 30%-100%.149,156,196-202 None of the available data dealt with the effect of noncompliance on clinical outcomes. One study suggested that noncompliance was related to gastrointestinal side-effects. While maintenance of high serum phosphorus levels could be due to noncompliance with phosphate binders, other factors—such as dietary indiscretion and phosphate release from the bone—must also be considered.
There are few studies that demonstrated optimal timing for ingestion of phosphate binders, but the general consensus among the Work Group is that binders should be taken 10-15 minutes before, or during, the meal.
In a study comparing calcium carbonate and aluminum hydroxide, bone mineral content was lower in aluminum hydroxide-treated patients. Minor, and inconsistent, differences were found. Because of the potential for neurotoxicity and osteomalacia associated with aluminum-containing phosphate binders,179,180,203 the use of these compounds should be reserved for patients with serum phosphorus >7.0 mg/dL (2.26 mmol/L) and only for short-term therapy. However, the Work Group acknowledges that, while there is morbidity associated with long-term aluminum intake, there is also increased mortality with phosphorus levels >6.5-7.0 mg/dL (2.10-2.26 mmol/L). Thus, the two issues must be balanced. At the present time, there is no evidence that short-term use of aluminum-containing phosphate binders is associated with the development of aluminum bone disease or neurotoxicity. Therefore, the short-term (4 weeks) use of these compounds is not contraindicated. However, calcium citrate should be avoided during treatment with aluminum-based compounds, since citrate increases the absorption of aluminum from the intestine203 and may precipitate acute aluminum toxicity.
In summary, the available evidence supports the hypothesis that all of the current phosphate binders are effective in controlling serum phosphorus levels. The majority of studies evaluated calcium-containing phosphate binders. However, recent studies on the use of the non-metal-containing phosphate binder sevelamer HCl suggest that it was effective,184,189,204-206 and the Work Group felt that this agent has an important emerging role in the control of serum phosphorus in dialysis patients. Sevelamer HCL has been shown to be an effective binder in children on dialysis.163,163a
In CKD Stage 5, the current evidence and the opinion of the pediatric Work Group support the recommendation that the choice of calcium-based phosphate binder should be determined by patient preference (number and size of binder, tablets or capsules), compliance, comorbid illnesses, side-effects, cost, and the ability to control serum phosphorus levels while maintaining the desired CaXP, and limiting the total calcium intake. Additionally, the pediatric Work Group also recommends reducing the dosage of calcium-based phosphate binder in dialysis patients with low PTH levels. The rationale for this recommendation is that these patients will usually have low-turnover bone disease, and the bone will be unable to incorporate a calcium load,207 predisposing to extraskeletal calcification. Also, calcium-based phosphate binders should not be used in patients with hypercalcemia or with severe vascular calcification (see below). In such patients, one should consider the use of sevelamer HCL to control serum levels of phosphorus while avoiding excessive calcium intake.
The available data do not quantify an exact amount of calcium that can be given safely as a calcium-based phosphate binder. This is an important issue as recent studies suggest that excessive calcium intake may worsen vascular and other extraskeletal calcification.80,84,208 Additional data that either did not fully meet the inclusion criteria, or that became available after the evidence report was completed, support the consensus of the Work Group about limitation of calcium intake from phosphate binders. These data were reviewed by the Work Group and are summarized as follows.
In a cross-sectional study evaluating the presence of vascular calcification as assessed by electron-beam computed tomography (EBCT) scan in children, adolescents, and young adults, the CaXP, prescribed calcium intake from phosphate binders, and duration of CKD were much higher in the young adult patient group with calcification. In the group with calcification, the mean dose of prescribed binder was 6.456 g/day (elemental calcium/day), compared to 3.325 g/day in the group with no calcification.80 Another cross-sectional study evaluating risks for significant vascular calcification assessed by ultrasound found, by multivariate analysis, that the calcium load from phosphate binders was greater in those with calcification compared to those without calcification.84 There was a progressive increase from 1.35 ± 1.10 g/day of elemental calcium in patients with no calcification by ultrasound, to 1.50 ± 0.81 g/day in those with a calcification score of 2, and 2.18 ± 0.93 in those with a calcification score of 4 (P = 0.001 by ANOVA).84 Lastly, a prospective, randomized, controlled trial compared sevelamer HCl to calcium-based phosphate binders in 202 dialysis patients. The study compared the effect on serum phosphorus, calcium, CaXP, cholesterol and LDL levels, and aortic and coronary artery calcification evaluated by EBCT. Sevelamer and calcium-based phosphate binders achieved control of serum phosphorus levels similar to the recommended KDOQI levels; calcium-phosphorus product was slightly higher in the calcium-treated group. There were more hypercalcemic episodes and more suppression of PTH in the calcium-treated group. Blood levels of cholesterol and LDL were significantly lower in the sevelamer-treated group. In the 80% of patients with calcification at baseline, there was significant progression in aortic and coronary artery calcification in the calcium-treated group, but no progression in the sevelamer-treated group. In the calcium arm, the average dose of calcium acetate was 4.6 g/day (1,183 mg elemental calcium per day). The average dose of calcium carbonate was 3.9 g (1,560 mg elemental calcium). It should be cautioned that the observed results could be due to calcium load or lowering LDL cholesterol. However, taken together, these studies support the conclusion that calcium intake from phosphate binders should be limited in CKD patients on dialysis (Stage 5) to under 1,500 mg/day, and possibly lower.
The total calcium intake from diet, calcium-containing phosphate binders, and dialysate ideally should be equal to the recommended daily adequate intake (AI) for adults (1,000-1,500 mg/day). Given that the daily dietary intake of calcium for most dialysis patients is only 500 mg due to the restricted phosphorus diet, this leaves only 500-1,000 mg elemental calcium from calcium-containing phosphate binders. However, the pediatric Work Group recognizes the overwhelming importance of controlling serum phosphorus levels, and recognizes the difficulty of doing so with calcium-containing phosphate binders while adhering to this limited daily calcium intake. Based on this and the above data, the pediatric Work Group recommends that the amount of calcium provided by calcium-based phosphate binders and diet should not exceed 2X the age-specific DRI (maximum to not exceed 2.5 g/day). This recommendation is not evidence-based and thus the clinician must individualize therapy taking into account cost, other vascular risk factors, and the patient's tolerance of calcium-containing binders. For further discussion of the issue of daily calcium intake in CKD patients, see the discussion in the section “Strength of Evidence” in Guideline 6.
For those patients who are on calcium-containing phosphate binders in whom the total elemental calcium intake, (including dietary sources) exceeds the upper limit recommended, the pediatric Work Group recommends consideration of adding a non-calcium, non-metal-containing phosphate binder to decrease the total calcium intake.
The best phosphate binders are those that the patient will take consistently and as prescribed while limiting total calcium intake. The ability to adequately control serum phosphorus rests on appropriate education, patient compliance, and the use of tolerable phosphate binders. The latter needs to be individualized for patients and thus will require continuous monitoring with renal dietitians.
Longitudinal studies are needed to evaluate phosphate binders and their efficacy, side-effects, and impact on morbidity and mortality. A recently completed study in adults demonstrated an advantage of sevelamer HCl compared to calcium-based phosphate binders in preventing progression of aortic and coronary arteries calcification. Further studies in both adults and children evaluating cardiovascular morbidity and mortality in dialysis patients are needed.